The Cooperative High Reliability Organization: Approaching a Zero-Defect Culture
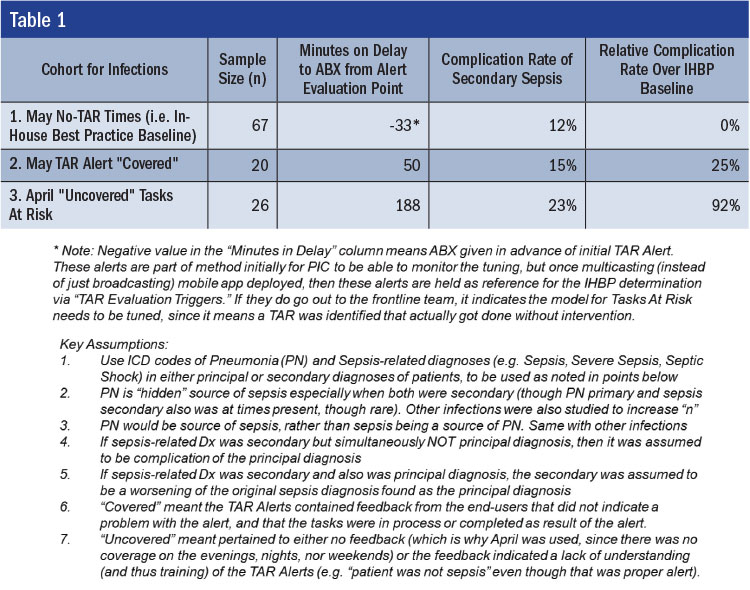
As the footnotes in the table describe, cohort 1 is the “current optimal” level of the team recognizing the need for an antibiotic in a timely fashion—the In-House Best Practice (IHBP) (Veluswamy, 2008). This IHBP level, as we would expect, would be without delays by the team (that would otherwise require the next prevention layer to intervene) because there was earliest possible recognition of the need in the facility. Cohort 2 is the comparison to IHBP once tasks fail at the prior prevention layer (i.e., the ED team), and how quickly the next prevention layer intervenes (due to being “covered” by the next layer). Cohort 3 is the “uncovered” contrast to the covered tasks at risk of failure. The cases in the third month of the study that were triggered for alerting but were not received by anyone in the organization due to the network access issues were compared for time-to-treatment (TtT) delays and also secondary complication rates (i.e., diagnoses considered more severe than the diagnosis that brought the patient to the hospital, such as pneumonia as principal diagnosis, and sepsis or severe sepsis as a secondary, as well as sepsis at admission, but severe sepsis as a secondary).
The TtT delay was longer between IHBP and covered task execution (IHBP being starting time, and covered being on average 83 minutes delayed in antibiotic administration). However, uncovered task execution was significantly longer (221 minutes past IHBP, or 2.66 times longer) than covered. 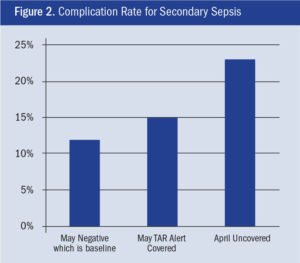
Delays from IHBP, as expected, increased complication rates. The rate for IHBP timing of antibiotic administration was determined to be 12%. This rate could be reduced through faster identification and administration than the IHBP currently offers (e.g., through new monitoring equipment, better-trained staff, etc.), but was still used as the baseline. The delay of 83 minutes in antibiotic administration appeared to lead to an increase from 12% for cohort 1 to 15% for cohort 2 (Figure 2). However, cohort 3 appeared to have a complication rate of 23%—nearly double that of the IHBP level of task performance. If we consider the 12% IHBP baseline complication rate as not preventable (at least in the current state), then any delay in antibiotic administration past that can be viewed as preventable.