The Cooperative High Reliability Organization: Approaching a Zero-Defect Culture
In a CHRO, the Performance Improvement Coordinator (PIC) (Johansson et al., 2016) monitors for task failure risks, while the PIC and support teams intercept tasks, either executing or reassigning them using MAM, to enable optimal cognitive load balancing (since knowing the load limits of key members of the team is crucial, given that different people have different task limits). The study facility’s prevention layers consisted of the ED team receiving and doing preliminary work with the patient, then a present on admission support team as a prevention layer to capture infections before they could become sepsis or worse (based on alerting).
In its first month, the study tested mobile app–based alerts intended for the ED that were initially sent to the PIC to validate the information presented by the model. In the second month, alerts were sent directly to the ED during all shifts (with the exception of the 12 a.m.–6 a.m. shift). 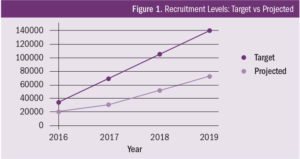
Results
In the second month of the study, antibiotics administration compliance increased from 50% to approximately 65%. However, in the third month, the hospital’s network malfunctioned, blocking phones in the ED from obtaining the alerts. This meant that only the day shift PIC received alerts, similar to what took place in the first month. This malfunction helped confirm that the loss of alerting led to degradation of antibiotics compliance.
In spite of the loss of evening, night, and weekend notifications, we were able to provide a comparison against a baseline of what would occur when prevention layers downstream were not notified of tasks that were likely going to fail (based on predicted task saturation). This essentially offered a double-blind study. Loss of micro-targeting on tasks at risk of failure led to compliance on antibiotics dropping to 43% in month three.
In the fourth month, alerts were restored, not just for 18 hours per day, but a full 24 hours per day, and the overall compliance on the cohort rose within five days (i.e., once training could take place on an additional team) to 70%. Compliance ultimately increased to 75% by the end of the study, once full alerting was added to include all shifts in the ED. Moreover, rate of incidence (one way to measure the outcome of addressing tasks at risk of failure) of sepsis, severe sepsis, and septic shock was reduced by 24% in the same month (Figure 1).
Table 1 shows the three types of cohorts examined during the study. The second and third cohorts had tasks at risk of failure in infections leading to sepsis, which impacted failure to recognize and failure to act in time for antibiotic administration. The cohorts were defined to show the full capability of micro-targeting on tasks at risk of failure in preventable complications when fully implemented, rather than the current results for the entire pneumonia cohort. There were many challenges ranging from technical to training issues in the last month of the study, which meant the team could not properly employ the micro-targeting. Thus, the cohorts depicted in the table show the potential benefit for the early (and more limited) use of micro-targeting, versus the more robust, optimal use of the method during the study (i.e., with full network access and properly trained staff), and the team’s force multiplication when variables for access and training were taken into account.
