To Do No Harm, Rethink How to Measure Hand Hygiene
By Paul Alper, BA
Primum non nocere is a Latin phrase that means, “First, do no harm.” It is a precept taught to healthcare students around the world and paraphrased in the Hippocratic Oath. Unfortunately, a vast amount of avoidable harm still takes place in healthcare settings worldwide. The good news is that a new technology can provide a solution to a decades-old challenge to patient safety professionals: how to accurately and reliably monitor hand hygiene—the simplest and most effective way to prevent healthcare-associated infections (HAI).
Personal and financial effects of HAIs
Ellen Hargett, RN, is the director of quality and process improvement at DeKalb Regional Health System in DeKalb, Georgia. She is trained in Lean and Six Sigma for controlling and improving quality and staff performance in the healthcare environment, and is a skilled and passionate patient safety proponent dedicated to helping her system find ways to avoid harm.
When Hargett became a cancer patient and had surgery at her own hospital, she knew the risks associated with her surgery, but infection was the last thing on her mind. She didn’t imagine that she would join the 700,000 people in the United States who, according to the latest data available from the Centers for Disease Control (CDC), contract an HAI each year, though she was thankfully not one of the 75,000 people who die from the infection (CDC, 2016). After undergoing further surgery to address complications from the cancer surgery, Hargett contracted a severe surgical site infection caused by methicillin-resistant Staphylococcus aureus (MRSA), bacteria that are easily transmitted, often as a result of improper hand hygiene. Hargett had to fight sepsis and deal with an abdominal abscess for months after the second surgery. She was informed that the best option was a third surgery, which would leave an opening in her abdomen for a week. She consented, and it likely saved her life.
Eight months following the initial surgery, Hargett returned to work, though her experience had left her with chronic complications. Hargett’s insurance company was billed $79,000 for the cancer surgery and $239,000 for treatments related to the MRSA infection.
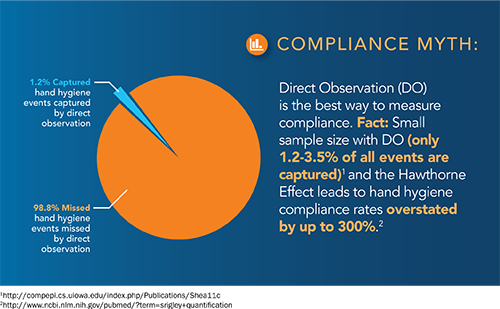
Using direct observation to measure compliance
Having had time to observe healthcare worker behavior during her ordeal, Hargett came to realize that true hand hygiene compliance at DeKalb Regional was less than 50%, which is typical for healthcare settings worldwide (McGuckin, Waterman, & Govednik, 2009). Many hospitals, however, boast compliance in the 90% range (Coyne, 2014). That discrepancy often results from hand hygiene compliance being measured by “secret shoppers,” human observers equipped with clipboards and pens—surprising in an age of highly sophisticated automation and technology. This approach to monitoring is also known as direct observation. Observers capture only a tiny fraction of all hand hygiene behavior, typically well below a sample size that would be statistically significant. Also surprising is the lack of mandated standards or guidelines for measuring hand hygiene compliance, leaving hospitals free to design their own measurement and feedback programs. Further compounding the problem, healthcare workers—no matter how discreet the secret shopper is—know when they are being observed and behave differently. This phenomenon is known as the Hawthorne effect: People behave differently when they know they are being watched.
A recent study in Canada found that direct observation resulted in 300% overstatement of hand hygiene behavior (Srigley, Furness, Baker, & Gardam, 2014). Reporting on the study, the Toronto Star said, “Healthcare workers wash their hands three times more often when under the watch of an observer than not” (Coyne, 2014). Collected weekly and published monthly, most Ontario hospitals boast hand-washing rates above 90%. That means for every opportunity hospital staff had to wash their hands, they did at least nine times out of 10.
But in reality, those numbers are less than 30%, according to Michael Gardam, Toronto University Health Network’s director of infection prevention and control and co-author of the study. This can have real consequences for patient health. Gardam was quoted in the Star:
If our numbers are above 90% but we’re still having infections, one obvious explanation for that is because you’re not washing your hands nearly as much as you think you are. We’re fooling ourselves. The numbers that we are getting and we are posting publicly are not real, they’re artificial. (Coyne, 2014)
This is not the only study to reveal a huge overstatement of compliance when using direct observation. A German study demonstrated a 275% Hawthorne effect in 2009 (Scheithauer et al., 2009). To sum up the problem, direct observation—the way that most hospitals around the world measure hand hygiene—gives hospitals a false sense of security, which leads to complacency and inaction. As a result, infections occur, causing pain and suffering and costing lives. Perhaps if hospitals knew their real rates, they would have a sense of urgency about improving them.
New technology offers a different solution
Over the past few years, Hargett has become aware of electronic monitoring systems, an emerging technology that can measure 100% of hand hygiene events accurately and reliably. As a result, she calls for a change to the standards and guidelines:
It is now time to recognize that direct observation is no longer the “gold standard” for measuring hand hygiene. With the availability of accurate and reliable electronic systems, it is essential that organizations that accredit hospitals, along with the government and private payors of healthcare, mandate that hospitals adopt technology that will lead to better outcomes and help eliminate the risk of avoidable HAIs.
Leaders in healthcare face daily pressure to drive quality improvement and economic efficiencies. This trend has become more prominent as the Centers for Medicare & Medicaid Services (CMS) levies penalties that demand hospitals improve quality or lose revenue. With the new penalty for hospital-associated conditions, including HAIs, imposed under the Affordable Care Act (ACA), hospitals can lose 1% of their total CMS revenue if they fall into the lowest-performing quartile of U.S. hospitals, so there are serious dollars at stake. In 2015, 724 hospitals were penalized, and 758 are being penalized in 2016, 54% of which are in the penalty zone for the second time (Evans, 2015). Today’s quality leaders and patient safety professionals must find new evidence-based ways to improve practices and standards of care, choosing methods that are both effective and relatively easy to implement in their organization’s culture.
Just as other areas of healthcare are adopting advanced technologies for improved efficiencies and care, electronic monitoring can measure compliance accurately and reliably. It has been shown to help drive true improvement in hand hygiene compliance and reduce avoidable infections and their associated costs. Thankfully, awareness of the connection between accurately measuring hand hygiene compliance and improving patient care while reducing cost is beginning to grow among senior hospital leaders.
EHCO alliance
To put the significance of hand hygiene compliance in the spotlight, eight companies that offer electronic monitoring technologies formed an alliance in September 2015 and announced their purpose and vision with the launch of their website in February 2016: the Electronic Hand Hygiene Compliance Organization (EHCO). EHCO’s purpose is to increase safety, reduce avoidable harm, and eliminate unnecessary costs at hospitals nationwide. It promotes changes in hand hygiene measurement policy and guidelines at accreditation organizations, government agencies, health insurers, and hospitals. The companies engaged in EHCO include Airista, BioVigil, CenTrak, Clean Hands-Safe Hands, DebMed, Hill-Rom, SwipeSense, and Versus Technology. All produce technology that can capture 100% of hand hygiene events and report compliance accurately and reliably.
EHCO’s goals align with those of hospital leadership: to reduce the risk of HAIs along with associated costs and potential penalties. EHCO invites patient safety and quality leaders to consider the real cost of using antiquated methods of measuring hand hygiene compliance and suggests that now is the time for hospitals to change how they measure this key performance indicator of patient safety and quality.
Outcomes achieved by early adopters
Electronic monitoring has only become widely available over the past four to five years. Now, evidence is beginning to emerge that it is accurate and reliable and can help reduce the incidence of infections.
A number of hospital systems have conducted early research and pilots to help develop and validate these systems. One of them is Greenville Health System (GHS) in Greenville, South Carolina. Connie Steed, director of infection prevention at GHS, has been working with one electronic hand hygiene company for the past seven years to help develop and perfect its system.
“We are excited to have electronic hand hygiene compliance measurement throughout our seven hospitals,” says Steed. “We now have a better understanding of the compliance rate for all of our hand hygiene behavior 24/7. We switched away from direct observation, the most common monitoring methodology, because it only gave us data for a small snapshot in time and healthcare workers behave differently when being observed. Thus, our rates with direct observation were much higher than our 24/7 reality.
“We have seen consistent double-digit increases in hand hygiene compliance and reductions in healthcare-associated infections,” continues Steed. “These benefits have come with cost savings that can justify the cost of the system.”
In an early study at GHS, hand hygiene compliance was measured on the same patient population for 15 months in three ways: direct observation, video monitoring (with patient consent), and electronic monitoring. Rates of compliance measured by video and electronic monitoring were statistically equivalent for the final 12 months of the study, while direct observation overstated compliance by an average of 33%. This study proved the accuracy and reliability of an electronic monitoring system and showed that the Hawthorne effect produces overstated and unreliable hand hygiene compliance rates (Diller et al., 2013).
In another study, staff feedback on soap versus sanitizer usage enabled by data from an electronic monitoring system significantly increased hand hygiene compliance with the hospital’s Clostridium difficile (C. diff) protocol. The protocol says to shift from sanitizer to soap-and-water hand washing when C. diff is identified because sanitizer does not kill C. diff spores; they need to be washed off with soap and water. During the study, the C. diff infection rate decreased from 7.03 cases per 10,000 patient days to 2.38 per 10,000 (Robinson, Boeker, Steed, & Kelly, 2014).
A third study, pending publication, will show MRSA rates decreased significantly when an electronic system was implemented and staff were properly trained on how to use and engage with the data to drive improvement.
Other hospitals are beginning to achieve similar results. Following implementation of an electronic monitoring system at a suburban Chicago hospital, overall hand hygiene compliance increased from 57% in December 2013 to 79% in September 2015—a 39% increase. Additionally, the rate of hospital-acquired MRSA dropped from 3.94 to 1.98 cases per 10,000 patient days—a 50% reduction. The facility paid no readmissions penalties in 2015 and was one of only seven hospitals in Illinois that paid no ACA-related penalties in 2015. In comparison, the facility had paid a 0.24% CMS readmissions penalty in 2013 (Bouk, Mutterer, Schore, & Alper, 2016).
Conclusion
Now, for the first time since Ignaz Semmelweis first proved the linkage between hand hygiene and deadly infections, there is a way to really know how well staff members are doing. Just as alcohol emerged as the new way to clean hands in the 1980s and 1990s and changed the way we think about and perform hand hygiene, electronic monitoring will likely change the paradigm for measuring compliance.
Direct observation still has an important role to play in hand hygiene, as an interventional tool for discovering and overcoming barriers and obstacles, as well as for giving feedback on technique and evaluating performance of specific groups, such as units or disciplines. However, the evidence is clear that its use as a measurement tool needs to be eliminated in the interest of patient safety and healthcare quality.
Just as we look down a hospital corridor today and see alcohol-based hand sanitizer dispensers as the standard of care, we will likely see unit managers looking at compliance rates for their unit on a monitor in real time, with pens and clipboards—along with many avoidable HAIs—a thing of the past.
Paul Alper is chairman of EHCO, the Electronic Hand Hygiene Compliance Organization (www.ehcohealth.org). He may be contacted at ehcohealth@gmail.com.
References
Bouk, M., Mutterer, M., Schore, M., & Alper, P. (2016). Use of an electronic hand hygiene compliance system to improve hand hygiene, reduce MRSA, and improve financial performance. Accepted for presentation at the annual conference of the Association for Professionals in Infection Control 2016.
Centers for Disease Control and Prevention. (2016, March 2). HAI data and statistics. Retrieved April 28, 2016, from http://www.cdc.gov/HAI/surveillance/#survey
Coyne, T. (2014, July 25). Ontario hospital staff not washing hands as often as reported: Study. Toronto Star. Retrieved from http://www.thestar.com/life/health_wellness/2014/07/25/ontario_hospital_staff_not_washing_hands_as_often_as_reported_study.html
Diller, T., Kelly, J. W., Blackhurst, D., Steed, C., Boeker, S., & McElveen, D. C. (2014). Estimation of hand hygiene opportunities on an adult medical ward using 24-hour camera surveillance: Validation of the HOW2 Benchmark Study. American Journal of Infection Control, 42(6), 602–607. doi:10.1016/j.ajic.2014.02.020
Diller, T., Kelly, J. W., Steed, C., Blackhurst, D., Boeker, S., & Alper, P. (2013). Electronic hand hygiene monitoring for the WHO 5-moments method. Paper presented at the 2nd International Consortium on Prevention and Infection Control, Geneva, Switzerland.
Evans, M. (2015, December 10). Half of hospitals penalized for hospital-acquired conditions are repeat offenders. Modern Healthcare. Retrieved April 17, 2016, from http://www.modernhealthcare.com/article/20151210/NEWS/151219988
McGuckin, M., Waterman, R., & Govednik, J. (2009, March). Hand hygiene compliance rates in the United States — A one-year multicenwter collaboration using product/volume usage measurement and feedback. College of Population Health Faculty Papers, 24(3), 205–213. doi:10.1177/1062860609332369
Robinson, N., Boeker, S., Steed, C., & Kelly, W. (2014). Innovative use of electronic hand hygiene monitoring to control a Clostridium difficile cluster on a hematopoietic stem cell transplant unit. Paper presented at the annual conference of the Association for Professionals in Infection Control.
Scheithauer, S., Haefner, H., Schwanz, T., Schulze-Steinen, H., Schiefer, J., Koch, A., Lemmen, S. W. (2009). Compliance with hand hygiene on surgical, medical, and neurologic intensive care units: Direct observation versus calculated disinfectant usage. American Journal of Infection Control, 37(10), 835–841.
Son, C., Chuck, T., Childers, T., Usiak, S., Dowling, M., Andiel, C. … Sepkowitz, K. (2011). Practically speaking: Rethinking hand hygiene improvement programs in health care settings. American Journal of Infection Control, 39(9), 716-724. doi:10.1016/j.ajic.2010.12.008
Srigley, J. A., Furness, C. D., Baker, G. R., & Gardam, M. (2014). Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: A retrospective cohort study. BMJ Quality & Safety, 23, 974–980. doi:10.1136/bmjqs-2014-003080
Steed, C., Kelly, J. W., Blackhurst, D., Boeker, S., Diller, T., Alper, P., & Larson, E. (2011). Hospital hand hygiene opportunities: Where and when (HOW2)? The HOW2 benchmark study. American Journal of Infection Control, 39(1), 19–26. doi:10.1016/j.ajic.2010.10.007
World Health Organization. (n.d.). About SAVE LIVES: Clean your hands. Retrieved from http://www.who.int/gpsc/5may/background/5moments/en/
