VLEHR: Virtual Longitudinal Electronic Health Records – An Approach to Quality Improvement
January / February 2005
VLEHR
Virtual Longitudinal Electronic Health Records – An Approach to Quality Improvement
![]()
Previous contributions to the idea of an electronic health record (EHR) have set the healthcare industry on the right path, and many companies are beginning to adopt these solutions. Solutions are often built around a simple concept: An enterprise can obtain a single vendor EHR application system, administer clinical data into a repository and provide a computer program that delivers reminders, data specific to a given patient at a specific time, in essence a repository-based clinical decision support system (DSS). While this goal is admirable, clients are realizing that a single data repository administered by the enterprise is not adequate for enabling widespread utility and adoption in the entire medical community.
The answer is an integrated composite application that spans multiple provider enterprises and administrators and provides a logical integration capability resulting from the appropriate architecture approach. One such client has been able to intelligently cross-index more then 9 million patient records, across 28 hospitals while eliminating duplicate records, removing duplicated and inconsistent data, and linking over 70 healthcare software systems. These are the results that integrated systems can provide and the value a VLEHR can begin to offer.
Despite many efforts such as health maintenance organizations (HMO), staff model medical teams, longitudinal care-management applications, patient-centric approaches, community-based initiatives, and medical records that are centered on application service provider (ASP) browser-based Internet technology, care delivery is typically not controlled by any single enterprise or organization, and seldom by a well integrated set of organizations. Medical care delivery is disjointed, spanning multiple agents (doctors, labs, pharmacies, insurance company care managers, hospitals, offices, and team members) and multiple locations.
To further complicate the issue, each enterprise usually has a unique and often proprietary desire to manage specific data flows. The above referenced organization is bringing together the diverse business needs of 15 sponsored hospitals, 13 affiliated hospitals, 3 specialty institutions, 6 long-term care facilities, 11 home health agencies, 62 satellite primary care centers, 12 physician groups, and 4 managed care entities. As can be imagined, the required set of data and data flows are varied, patients are mobile across agents, and administration of current data frequently lags behind these migrations.
The healthcare industry has not found a single system, repository, application, or enterprise that could, should, or would want to administer the complete set of all the data related to this diverse environment, let alone attempt to integrate it all into concise and accurate patient information. Bringing together large-scale cost issues with the extensive goal of coordinating a single medical record is an enormous effort. Healthcare clients are also constantly finding more ways to extend their business requirements and hence data needs, including emerging radio frequency identification, robotic image-guided systems, e-prescribing, and implanted medical record chips advancements. Healthcare groups that begin utilizing data in an organized and methodical fashion provide better business results while increasing the quality of care patients receive.
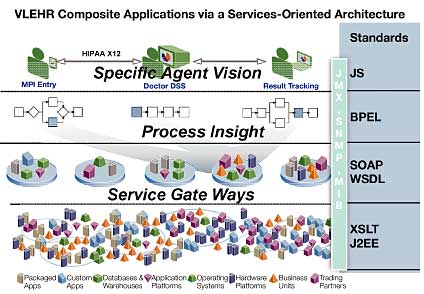
Only when data is assembled relevantly, based upon specific criteria by an intelligent agent, does it become meaningful information. Relevance is a key concept that leads to deeper insights into providing the right patient, with the right data, at the right time, and in the right place. To make this data more meaningful requires new functionality that is made available by composite applications, including both customized and packaged solutions. The composite application approach in a network setting permits contributions that surpass the capabilities of single enterprise clinical information systems. The composite application will expose data from among multiple locations in a network-specific query set that in effect becomes an agent-specific view into a virtual longitudinal EHR, presenting relevant and specific data. The view will understand care state transitions when moving location, integration demands, and workflow and will also be orchestrated in a fashion that allows flexible access and total privacy control.
There are other significant technical insights and capabilities that clients are adding to take the potential of the VLEHR to the next level, including the addition and correct integration of components:
- Object-oriented hardware and operating system-independent technology such as JAVA to leverage multiple modalities and devices. Devices include wireless handheld and real-time hardware such as the hospital computer network-integrated controllers and robotics.

- Rapidly adopting architectures that require virtually no programming or additional tools and near zero programming architectures and tool sets that integrate your existing technology and orchestrate automatically to provide rapid business process transformation.

- Business process management control models and tools that will deliver and demonstrate workflow-based composite integration.

- Business activity monitoring capability and tools.

- Care delivery state transition management capability and tools; without state transition management, data can be inaccurate or have no relevance.

- Composite applications delivery and administration capability.

- Relevance engines and algorithms.

- Virtual service-oriented, architecture-based composite applications that span the multiple agents in the healthcare delivery process.

- Agent-specific access and views.

- Security and access controlled by the owner of the privacy rights to the data.
When correctly added to legacy and foundation systems, the components listed above allow for the evolution of the VLEHR. Challenges surrounding the need for true integration and hindrances to employing an integrated composite application network in the medical environment should be addressed as well. Challenges include:
- Privacy and security: Who controls who sees what and when and what records are maintained of access.

- Regulatory compliance: What are the relationships between agencies, who enforces, who inspects; today this is very sporadic and loose.

- Administration of architectures, data, and systems: Today they span many technology generations. I have seen systems running on software that is no longer vendor-supported; huge costs are associated with the lack of elegance in this area. A great many monolithic systems are not adaptable and transformable, yet huge expense goes into maintenance just to keep them in place. Many systems no longer satisfy the users, but those systems and vendors appear to be too engrained to remedy the problem at reasonable costs.
Most attempts document in part rather than integrate across the whole care delivery cycle including:
- Computerized medical records (CMR) usually make some documents of a medical record available electronically.

- Electronic medical records (EMR) typically add the ability to restructure and optimizes documents.

- Electronic patient records (EPR) typically are patient-centered records with information from multiple institutions; these do a better job of integration but are seldom complete.

- Electronic health records (EHR) typically add general disease-related information to the EPR.
The VLEHR would encompass these approaches but focus on relevance derived from all instances of care, organized around appropriate insights of state transitions in the care delivery process. The key is accurate, current, and relevant data appropriate to the time, place, provider, and patient need: nothing more and nothing less. The VLEHR naturally would allow the provider to branch out from the initial access point as needed.
Incorrect Assumptions in Place Today
Several incorrect assumptions have hindered the evolution, utility, and widespread adoption of the electronic health record.
A single, repository-based solution to the need to integrate medical records within an EHR is not realistic for most organizations primarily due to high development and maintenance costs. It is certainly not economically feasible due to the limited resources and budgets of healthcare facilities. Further complicating the adoption process is the difficulty in administering such programs, keeping them legal, secure, current, and accurate. Maintaining the data needed for the full continuum of care is a particular challenge when no single enterprise administrates all the data. Even with the consolidation of healthcare companies, data must be integrated from multiple independent administrators, and in effect enable a logical virtual repository that physically is based in a multitude of data stores and applications. For true integrity, data ideally should only be stored and maintained at the source of origin, thus providing decision support elements that are relevant to the specific agent and can be accessed via integrated composite application networks regardless of administration site.
Single master patient indexes (MPIs) provide identity management and unique identifiers, but as clients employ these solutions, they find there are subtle differences between indexes, directories, catalogues, and other management approaches. No single MPI can accomplish all of the myriad functions required to accomplish the optimal coordination of data. For the VLEHR to function, state transition management of all data is key; as data is transformed and modified across the care delivery process, the “state” of the data must be tracked across the multiple “transactions,” and appropriate management of the meta data needs to be accounted for at all instances of access.
Also necessary for the VLEHR is relevance matching of data presentation. Only data that is appropriate to a specific provider, based upon specific clinical need, should be presented; more data or less data complicates decision support and hinders care delivery. Today the master patient index alone does not manage relevance or state transition across agents or data elements relative to agent-specific related decision support system requirements. Today many national and international applications and approaches attempt to use the MPI in this fashion, but clients are finding that an MPI alone will not accomplish the goal. The ability to integrate and remediate multiple MPIs and non-unique identifiers across multiple geographic, political, and business boundaries in a secure integrated fashion is required.
Some national healthcare programs, large integrated delivery networks, large insurance companies, healthcare informatics companies, and government agencies currently attempting to provide and administer EHRs, outcome data bases, and MPIs at the enterprise level are beginning to determine that a single agency will find difficulty administering a meaningful and adequate data and service set. The reality is that there is no single EHR, index, database, or spine (central data repository that applications can plug into or build upon) that can ever be comprehensive and monolithic enough to embrace the full continuum of data and care delivery activity and state transitions, regardless of the amount of preplanning undertaken. To be useful and relevant, a VLEHR must be built on a composite application that spans multiple agents and episodes of care, delivering views into a longitudinal set of services at a specific point in time. The virtual VLEHR will also have to fully manage state transition and relevancy across all agents, episodes, and all data in order to present meaningful data and orchestrate that data into agent-specific requirements. Additionally that composite application will need to provide adequate security and patient privacy rights to determine which agents see which data at a specific time and place.
It is apparent that the future state of enterprise-level clinical information systems, EHRs, and repositories require an integrated network of composite applications to enable a virtual longitudinal electronic health record.
![]()
Current Capabilities
Current technologies, architectures, and approaches finally allow evolution to wide adoption and utilization of electronic health records. Service-oriented architectures (SOA) indicate that the current generation of technology vendors understands the needs of global business integration and transformation. They are moving away from “siloed” applications, such as those traditionally found in government programs, toward integrated solutions in which the appropriate information is supported for global enterprise integration and transformation.
Technology advances have taken healthcare to a new level, delivering flexible, adaptable SOA composite applications that leverage disparate legacy and foundation systems. These advances allow individualized standards for user workflow processes and service-specific views to be integrated across all enterprise data. These capabilities form a basis for the advance of the next generation of EHR.
In emergency rooms, doctors often need to see patient data that is specific about the time, place, and multiple episodes of care or other providers of care. Imagine also that the data resides across several systems that are under diverse management. This situation takes place at hospitals every day, often with critical care components. To maximize patient safety, the data must be current, complete, concise, and readily available.
New technology deployed by a large hospital system in Seattle has allowed practice physicians to leverage and reuse existing technology to securely view current patient data at the point of care in real time, helping providers react to trends in a patient’s history, review allergy and medication information, and better understand and suggest proper next steps or protocols — ultimately improving quality of patient care and patient satisfaction.
There are many benefits associated with using composite EHR applications to leverage an infrastructure, including:
- The ability to share patient information.

- Accurate documentation that is in line with current legislation and avoids opportunities for human error, such as handwriting documents and misreading information.

- Workflow and increased economies of scale are achieved by reducing manual labour, which is evident for example in chart pulls. At $35 dollar a chart pull, in a hospital of 95,000 patients, the cost savings alone are significant.

- Reuse of infrastructure and information stored in electronic format.
Evolving VLEHRs support a business process management tool with:
- A model of the episodes of care flow, which allows entities to query across multiple enterprises.

- A business activity monitor to know what data is current and what may be off line.

- An MPI remediation tool to pull an index together to query the multiple systems.

- A network of integrated composite applications to enable the orchestration and presentation of the relevant data from multiple enterprises.
With an integrated composite application network, doctors can see patient-specific information: blood type, allergies, prescriptions, appointments for specific sets of problems, etc., with full drill-down capabilities in other critical areas. The patient would have the ability to review and approve or deny access for specific data and providers. With these activities in place, the correct views of information would be presented, the query structure would be stored for audit trail purposes, but the actual data information result set would not have to be retained because the data is all stored in source systems or origin.
Conclusion
In conclusion, healthcare entities have the ability to access information with flexibility, security, and efficiencies never before available, optimizing patient care and fiscal responsibility. To begin accessing patient information in a timely, relevant, and safety-oriented fashion, these enterprises must embrace VLEHR technologies while grasping the requirements of moving business and care processes into the new millennium. The systems in place today can be better integrated and data exposed through integrated composite application networks. This architecture approach will enable virtual longitudinal access of data that can composite into an electronic health record that enables data state transition management and relevance matching appropriate to care delivery. The list of components for the VLEHR must include:
- Integrated composite application networks are required to enable VLEHRs.

- The VLEHR composite application must span multiple data repositories and foundation/legacy systems.

- The VLEHR composite application must, in a network fashion, logically span multiple geographic locations, agents, enterprise, and time frames.

- The VLEHR composite application must be object-oriented, standards-based, support service-oriented architectures and be capable of spanning multiple modalities and delivery technologies.

- Clinical workflow and process management-based multiple MPI remediation is required to support the VLEHR.

- Agent-specific decision support that understands state transition and can conduct data relevance matching is required. Each agent only wants to see specific data items at specific times and only on demand.

- The owners of privacy rights need to control access by data domain and agent on demand in order to effectively enable the VLEHR.
The healthcare industry now has standards in place, such as HIPAA, HL7, and others; Web services; integrated composite application network tool sets; and the ability to deliver composite applications supported by service-oriented architectures to enable VLEHRs that span enterprises, agents, states, and time.
Lindsy E. Strait is chief technology strategy officer for healthcare at SeeBeyond, a supplier of integration and composite application development solutions, based in Monrovia, California. Prior to SeeBeyond, Strait served as senior manager III, as well as subject matter expert/consultant for healthcare at Cap Gemini, Ernst & Young, LLP, (CGE&Y), a healthcare consulting company. Prior to CGE&Y, Strait held the position of senior vice president business transformation and SVP new ventures groups at HealthNet, Inc.
Strait graduated from the University of Southern California with a master’s degree in systems science computers & logistics and the University of Virginia, Mary Washington campus, with a bachelor’s degree in philosophy and law, and drama. Strait is also a graduate of the U.S. Marine Corps Computer Sciences School. He may be contacted at lstrait@seebeyond.com.
