Using Technology to Establish Clinical Context
January / February 2008
Using Technology to Establish Clinical Context
 |
|
| The association between the patient’s wristband active-RFID tag and the one worn by the nurse can be used to measure direct-care time. |
As health systems continue to extend evidence-based medicine by implementing EHRs, CPOE and clinical decision-support tools, other, complementary, IT-enabled tools are maturing to help transform the clinical enterprise. One of these technology enablers combines automatic identification (autoID) and real-time location systems to establish clinical context, the set of circumstances that surround a particular patient-centered event.
Clinical context provides us an associative view of the patient — a coherent view of the patient in time and space — that can result in a smoother, more integrated flow of the patient through the health enterprise. It’s where high-tech logistics meet clinical transformation.
Clinical context begins with smart use of available autoID technology. We all use autoID technology regularly. In essence, autoID technology is a computer system that can identify people or things. The barcode is one of the simplest forms of autoID: when we pass through the store checkout and our items are electronically scanned by the clerk, the system sends each product’s barcode to a computer that records product price and description. Because this form of autoID has been used ubiquitously for years, most of us take it for granted. Barcodes have increasingly found their way into hospitals to allow the identification of patients, staff, drugs, and medical devices (HIBCC, 2007).
We use a slightly more sophisticated form of autoID in the card that allows us into our hospital, garage, or office. This card has a small electronic circuit in it called a passive radio frequency identification, or passive RFID, chip that identifies you the bearer to the computer in the box next to the door. A swipe of the card by the box allows the computer to compare data from the RFID chip to a list of those folks authorized to unlock the door. If you’re on the list of this “in crowd,” the door unlocks.
AutoID systems tend to be short-range in operation; the RFID card to unlock the door needs to be brought up quite close to the reader. And, while location can be inferred from some of these systems — the system knows you were at a specific door at a specific time — it doesn’t know where you were before you got to the door or after you walked through it. In contrast, real-time location systems (RTLS), offer the identification that other autoID systems provide, but also continuously update location data. RTLSs typically use a small tag with a radio in it and then transmit the radio signal to receivers planted throughout the hospital and linked to a computer network. Once the central server receives the signal, it calculates the location of each tag. The whole process, which takes only milliseconds, works only if antennas are in place — that way the radio signal can be “heard” — so the coverage area can be set up to preclude tracking of people or things in sensitive areas like bathrooms or lounges. Unlike the more common passive RFID systems, which are short range (~ 3 inches), these RTLS have a longer range (~ 30 feet).
![]()
AutoID, RTLS and Context
As mentioned earlier, context is the set of circumstances that surround a particular event. AutoID systems create the foundation for context via identification and location at a specific point in time. RTLS extends this ability much further by determining identification and location continuously over an extended period of time. For example, an organization may be interested in the “event” of a clinician logging onto a PC. In this scenario, the clinician can walk up to a computer terminal, “present” their ID card — containing an RFID chip, magnetic stripe or barcode, depending on the type of autoID technology being used — to the computer, which would recognize the clinician as authorized and log them on. Here the AutoID system is establishing the context or set of circumstances around use of the PC.
What if, rather than merely barcodes, the system used an RTLS? How would this enrich our contextual knowledge? Let’s assume the same scenario as above, but add an RTLS tag to the computer so its location can be established. Now when the clinician walks in front of the computer she is automatically logged on, triggered by a “knowledge engine” that determines both her location and that of the PC. Perhaps more importantly, should the clinician walk away from the computer — calculated as a distance/time algorithm — the computer either logs her off or displays a screen saver as a security measure. Again, the context of the computer’s usage is established, but this time with the added richness of location.
RTLS vendor Radianse has patented technology based on a software algorithm that can determine when people and devices come into proximity — for example, the clinician and the computer — and undertake an action: logging on. We call this an association.
The concept of establishing context in healthcare provides a powerful foundation for everything from improved hospital management to the practice of evidence-based medicine. An increasing number of hospitals are using RTLS at its basic level, for example, to quickly locate lost or misplaced equipment. Using RTLS as an asset-management tool in this way allows hospitals to save potentially hundreds of thousands of dollars in equipment purchase and rental, as well as saving staff time otherwise spent “hunting and gathering.” A simple web-based query — “Find me a bariatric wheel chair” — can save a lot of time and grief. Adding a bit of context — “Find me a bariatric wheel chair that is in a clean equipment room” — can save even more time and resources.
RTLS can also help dramatically streamline the revenue cycle, especially billing processes, by triggering automatic billing and encounter documentation. Knowledge of the location of staff members and patients allows automatic documentation of the time and duration of their encounters. This can simplify billing related to such charges as anesthesiologist time in the OR, patient care in the ED, and other services.
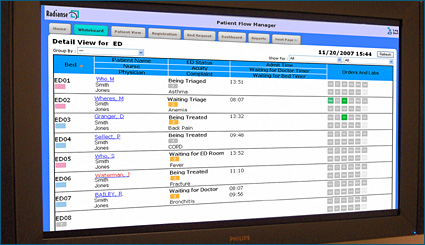
Patient flow is another area greatly amenable to application of RTLS technology. In the last 3 to 5 years, hospitals have discovered that ED overcrowding often has nothing to do with the ED. Instead, it arises from bottlenecks “downstream” on med/surg floors from mismanaged bed capacity. While systems to automate clunky manual white boards have added great efficiency in this area, RTLS takes this process even further.
By identifying the location of patients and staff, next-generation RTLS-based patient-flow systems can infer that a patient has been discharged (by knowing when they leave the building for a long enough period of time), automatically page housekeeping to clean the patient’s old room, and then document that the room is ready for a new patient (by inferring from the location of the housekeeping staff that they’re done cleaning the room). All of this happens automatically — no calls or pages to and from nursing, housekeeping, transport, or the bed coordinator.
Supporting Evidence-Based Medicine
Many hospitals have documented hard and fast returns from their investments in RTLS through such applications, including returns from reduced costs (buying less equipment) and increased revenues (serving more patients). However, that’s just the beginning. Once in place and financially justified, these systems can support evidence-based medicine as part of the clinically transformed enterprise. Indeed, we believe use of RTLS should become a critical foundation for the advancement of evidence-based medicine.
Evidence-based medicine is defined as “the judicious use of the best current evidence in making decisions about the care of the individual patient” (Sackett, et al., 1997). While comprehensive, peer-reviewed scientific studies define the “best current evidence,” implementing best practices from that evidence can be another matter altogether. Frenetic clinical environments, patients with co-morbidities, and patients who fail to comply with regimens can thwart even the best-laid clinical plan — and local circumstances may ultimately dictate different approaches. Even the most robust CPOE system can be rendered ineffective if execution fails.
Enter RTLS. The same technology used to establish the context of a clean patient room can be used to establish the context of evidence-based medicine by documenting what is really happening with the logistics of patient care. When was the drug given? Who was working with the patient for how long? Where exactly was the patient in the care path?
The Potential to Transform Stroke Care
Stroke is a case in point. When a patient presents in the ED with stroke symptoms, one of the first decisions is to diagnose the stroke as hemorrhagic or ischemic. If the stroke is hemorrhagic, thrombolytic therapy is contraindicated, dangerous. If the stroke is ischemic, a powerful clot-busting drug is recommended. A CT scan of the brain typically determines the type of stroke — and timeliness is critical: Aggressive and timely management can spare a patient’s brain damage and future disability. Neurologists often describe this as, “Time lost is brain lost” (Shaw, 2005).
Giving a stroke patient an RTLS tag upon admission, however, empowers the ED care team with “eyes” to view what’s actually occurring with the patient along the care pathway. Clinicians can visually determine via screen displays if and when the patient is hitting certain milestones — we call “moments of truth” — within acceptable timeframes. Adding triggers and alerts — patient flow’s version of clinical decision support — helps ensure these moments of truth are met.
For example, if a CT scan was ordered but the patient has not entered an imaging room within 15 minutes of hospitalization, the system can trigger care-team intervention. Hospitals can design how these automatic triggers are delivered — page, phone, VoIP. Again, the system associates identification (the patient) with location (CT scan) and time. Nearly every moment of truth in the continuum of care is amenable to RTLS. Further granularity in the CT-scan process, for example, might involve triggering an alert if a technician has not arrived to transport the patient to imaging. Other moments of truth:
- Portable chest X-ray — associates the RTLS tag on the device with the RTLS tag on the patient;

- Testing blood glucose — associates the RTLS tag on the glucometer to the patient;

- Performing a12-lead ECG — associates the RTLS tag on a technician or machine to the patient;

- Time seen by neurologist — associates the neurologist’s RTLS tag to the patient;

- Administration of clot-busting drugs — associates the RTLS tag with the medication to the patient.
This context — associating the patient with a location, device or clinician — can potentially transform stroke care by significantly helping the care team achieve pathway requirements. In this way it enables physicians and other healthcare professionals to provide evidence-based medicine. RTLS can prove to be an invaluable tool to improving the handoffs, communication, and the treatment necessary for positive outcomes.
Monitoring Contagious Disease Transmission
RTLS can also be a wonderful tool in monitoring contagious disease transmission across hospitals. A big challenge in identifying super bugs such as MRSA (methicillin-resistant staphylococcus aureus), tuberculosis, or influenza is the hours-to-days time delay required to culture and diagnose the infection. During this period, the patient is within “droplet range” of multiple caregivers and other vulnerable patients. Once the patient is diagnosed, a hospital faces a time-consuming retrospective chart review to determine who was near that patient during this infectious time.
It’s unlikely that EMR will track every encounter. Not every healthcare worker, volunteer, or patient who was in close vicinity to the patient can be documented in the record, especially given such unmonitored activities as waiting for the elevator, delivering a newspaper, or assisting in positioning the patient. However, if the patient was paired with an RTLS tag at admission, and each healthcare worker wore an RTLS tag, the system can automatically log each encounter. The system would not only know who was near the patient but exactly where and for how long, making the forensic epidemiology of tracking an infectious patient from admission through discharge quite manageable, allowing the hospital to respond more quickly.
Conclusion
To date, the work that clinicians, researchers, and quality experts have done in advancing evidence-based medicine can only be described as heroic, given the obstacles and the promise. EHRs, CPOE, and clinical decision support provide a foundation for evidence-based medicine. However, it’s becoming increasingly clear that clinical rules, protocols, and guidelines, no matter how accurate, cannot transform the clinical enterprise alone. Execution is key. That’s where auto-ID and real-time location systems (RTLS) come in. They provide the context in which evidence-based medicine can thrive.
Mike Dempsey applies his more than 20 years’ experience in wireless medical communications as an investigator at the Sims Lab, which resides within Massachusetts General Hospital’s departments of Biomedical Engineering and Anesthesia. He is also a co-founder and chief technology officer of Radianse, a provider of asset and patient tracking and workflow and analytics solutions for healthcare. Dempsey may be contacted at mike.dempsey@radianse.com.
Sue Niemeier joined Radianse as director of clinical operations in 2006 after more than 16 years of nursing and business leadership experience, most recently as manager of Research and Development for Ascension Health, the nation’s largest nonprofit health system. In that role she led a large, multi-site time and motion study co-sponsored by the Robert Wood Johnson Foundation, Ascension Health, and Kaiser Permanente — essentially another example of understanding clinical context to make informed decisions about designing the care environment. Niemeier may be contacted at susan.niemeier@radianse.com.
References
HIBCC (Health Industry Business Communications Council). (2007). The health industry bar code (HIBC) provider applications standard. Available at http://www.hibcc.org/AUTOIDUPN/docs/ANS-HIBC%20PAS%201.2-2006.pdf
Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t. BMJ 312(7023), 71-72.
Shaw, G. (2005, November). Hospitals adopt new protocols for stroke care. ACP Observer. Available at www.acponline.org/journals/news/nov05/stroke.htm
