Understanding Care Transitions as a Patient Safety Issue
May/June 2011
Understanding Care Transitions as a Patient Safety Issue
The global re-hospitalization rate of a community reflects the cumulative quality of care provided across diverse healthcare settings and providers. Nationally, almost 20% of Medicare beneficiaries are readmitted to the hospital within 30 days of discharge (Jencks, et. al., 2009). The Medicare Payment Advisory Commission (MedPAC) estimates that up to 76% of these re-hospitalizations may be preventable (MedPAC, 2007).
Despite the best intentions of healthcare professionals, each setting tends to operate independently, leaving professionals unaware of issues that impact care as patients move across the care continuum. Incidents associated with poor transitions of care can lead to patient safety issues, medication errors, and miscommunication among patients, caregivers, and providers, which endanger patients’ lives, waste resources, and frustrate healthcare consumers.
The term “care transitions” refers to the movement of patients between healthcare practitioners and settings as their conditions and care needs change during the course of a chronic or acute illness (The Care Transitions Program, 2007). Interventions that identify and rectify system-level drivers of fragmented cross-setting care coordination are associated with reductions in re-hospitalizations. The success of improvement efforts depends on the development and strengthening of community partnerships that collectively acknowledge the patient as the center of focus when planning for the patient’s healthcare needs.
Cross-Setting Collaboration
IPRO, the Medicare Quality Improvement Organization (QIO) for New York State, is one of fourteen QIOs funded by the Centers for Medicare & Medicaid Services (CMS) nationally to improve care transitions for Medicare patients, their families, and caregivers. IPRO’s 3-year project (August 2008 to July 2011) is being conducted in five contiguous counties in upstate New York, involving 50 providers and impacting more than 68,000 Medicare beneficiaries (Figure 1). These providers represent the hospital, home health, skilled nursing, short-term rehabilitation, hospice, dialysis, and physician practice settings.
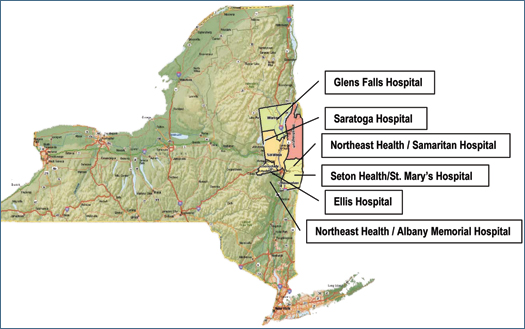
Figure1. IPRO’s Care Transition Initiative five-county target community is located in the Upper Capital Region of New
York State
Courtesy of IPRO
The goals of this project include:
- development of cross-setting provider partnerships, with the patient at the center of attention;
- improvement in communication between provider settings to strengthen care coordination;
- facilitation of streamlined access to patient-specific information across provider settings;
- improvement in patient satisfaction regarding the care transition process, and enhancement of patient chronic disease self-management skills; and
- implementation of systems to decrease adverse drug events during the transition process.
Initial Focus: Facilitating Partnerships
The focus of this initiative has been to facilitate cross-setting partnerships among providers that share care management of Medicare beneficiaries within each community and to develop a shared learning collaborative model for all participating providers to learn from one another’s successes and challenges. The initial strategy was to improve the patient and caregiver experience and outcomes by bringing providers together to shift the paradigm of care management away from “siloed” care delivery with little direct communication between providers, to patient-centered care that spans the healthcare continuum.
The six participating hospitals have taken an active role in collaborating with their community partners to address care coordination, information exchange, patient education, and medication reconciliation on a cross-setting level. They have also investigated their own internal systems and processes in these areas to target opportunities for improvement and to implement strategies and interventions to improve care coordination. Following are some of the New York Care Transitions Initiative hospital providers’ experiences so far.
Bringing Together a Care Community
Ellis Hospital
Schenectady, New York
For Ellis Hospital, a 455-bed acute care facility serving both urban and surburban municipalities, all healthcare providers in the community are key partners in reducing potentially avoidable readmissions. “The community has worked together to develop systems of care management,” says Stephen Wright, RN, BS, cardiology program director, who has spearheaded the hospital’s efforts to reduce heart failure (HF) readmissions.
The effort has brought together providers including community-based cardiologists and primary care physicians, as well as the leadership of skilled nursing facilities (SNFs) and home health agencies (HHAs), in an effort to address this issue.
The project began in 2008, shortly after Wright and colleagues were contacted by IPRO about participating in the community-wide care transitions program. Medicare claims data analyzed by IPRO showed that HF patients had the highest 30-day readmission rate at Ellis.
Wright worked with Director of Medical Staff Quality James Desemone, MD, to begin outreach to the healthcare community, and pulled together an internal care transitions team, which includes case managers, hospitalists, discharge planners, nurses, and representatives from hospital pharmacy, nursing education, medical records, and information services.
Monthly meetings, which include IPRO, are held to discuss issues, share information, and measure progress against benchmarks. The team has two subgroups—one works on issues related to medication reconciliation, while the other focuses on other care transitions issues, including information sharing with HHAs and SNFs. One of the team’s first projects was the creation of a patient-centered HF pathway. “Patients need to be involved in this pathway from the day of admission, so they are well prepared for when they return home,” says Wright.
Starting on Day 1 of hospitalization, patients learn about heart failure, their medications, tests, and other key information. On Day 2, Wright and his colleagues begin using “teach back” methods—asking the patient to explain back to the clinician what he or she has learned. All elements of how to care for oneself on returning home are taught through videos, one-on-one reinforcement, and teach back, beginning on the patient’s second day in-hospital.
One educational tool developed as part of this initiative is a brief self-care guide for heart failure patients. The guide is arranged into green, yellow, and red “zones,” each using bulleted lists to describe symptoms, activities, and action steps corresponding with how well controlled the patient’s HF is. This and other tools are explained while the patient is in the hospital and are reinforced during the discharge process to enhance the patient’s understanding of his or her chronic illness, increase adherence, and improve self-management skills.
A large percentage of Ellis’ HF readmissions are from skilled nursing facilities, so early on in the project, the hospital’s care transitions team began meeting with the leadership and medical directors of the region’s SNFs to strengthen communication and reduce avoidable hospitalizations. HF patients discharged to home are referred to the Care Transitions Intervention Coaching program.
The Coleman Care Transitions Intervention (CTI) Coaching Model (The Care Transitions Program, 2007) was developed by Dr. Eric Coleman from the University of Colorado. In this model, a Care Transitions Intervention Coach works closely with high-risk patients and their caregivers to help them better understand management of their chronic illness and to facilitate self-empowerment by conducting a follow-up visit and phone calls to help provide continuity and reinforce learning.
The Coleman CTI Model is built on four pillars:
- Physician follow-up appointments within 1 to 2 weeks of hospital discharge.
- Completion of accurate medication reconciliation.
- Red Flags (patient education regarding high-risk symptoms).
- Use of a personal health record (PHR).
In the Ellis program, a care transitions coach visits the patient at the hospital prior to discharge to go over self-care instructions, the importance of follow-up doctor visits, and to review medications. The coach then visits the patient at home as well, with subsequent follow-up phone calls for a 30-day period to ensure appropriate follow-up care post-discharge.
Interdisciplinary Teams Work to Improve Communication
Northeast Health / Albany Memorial Hospital
Albany, New York
Northeast Health / Samaritan Hospital
Troy, New York
Northeast Health is a large healthcare system in New York’s capital region, comprised of two hospitals, an acute rehabilitation hospital, a large home health agency, and a number of skilled nursing facilities. Readmission reduction efforts have centered on improving processes of care, according to Karen Julian, RN, and Valerie McMahon, RN, case management coordinators for Albany Memorial and Samaritan Hospitals, both of whom have played key roles in these efforts. An interdisciplinary team that meets daily at each hospital has been the key to Northeast Health’s attempts to reduce readmissions at the system’s hospitals by 30%.
Northeast Health began working on care transitions with the Institute for Healthcare Improvement (IHI) in 2009, and then started working with IPRO in early 2010. A major emphasis has been placed on improving communication with patients and their families. “What we learned from both IHI and IPRO, is that in order to improve patient communication we need to problem solve every day about what is and is not working,” says Julian.
Interdisciplinary teams at both hospitals hold daily meetings to ensure that a comprehensive plan is in place for all patients. Included on the team are representatives of dietary, nursing, pharmacy, nursing education, respiratory therapy, and physical therapy departments; case managers; nurse directors; and representatives of Northeast’s visiting nurse association and rehabilitation facilities.
Northeast Health makes use of information technology to identify patients who are at high risk for readmission. Among the ways high-risk patients are identified are: key diagnoses (CHF, diabetes etc.); known readmissions within 30 days; and more than one readmission per calendar year. The team had some data when it started the readmission reduction initiative, but key elements were missing.
“Because we didn’t have readmission data on patients discharged from one of our hospitals and readmitted to hospitals outside our health system, readmission rates were underestimated,” says Daniel Silverman, MD, vice president of medical affairs. IPRO was able to share Medicare paid claims data that provided a more comprehensive rehospitalization picture. While the retrospective review required a major time commitment, it did help the team identify patients at high risk, allowing for pro-active interdisciplinary case management.
It became critical to engage primary care physicians in the community to ensure that there was continuity when patients were discharged, as hospitalists provide most inpatient care in Northeast’s hospitals. One care transitions goal is to have patient discharge summaries dictated by the hospitalist for immediate transcription, with a copy provided to each patient/family member and a copy automatically faxed to the patient’s PCP. Hospital staff members also work with physician practices to establish a follow-up appointment within 7 days following acute discharge. The appointment is incorporated into discharge instructions to ensure that patients receive timely follow-up care.
A unique strategy at Northeast for all transfers (including rehab and SNF) is a verbal “nurse to nurse report,” says Julian. The verbal report, which is given by the hospital nurse to the nurse receiving the patient, includes detailed information on diet, activities of daily living, medications, social issues, and many other areas. For short-term rehabilitation transfers, the patient and family are educated on and engaged in the discharge plan by being included in this discussion when possible.
A number of additional strategies are used to improve care transitions, including transition coaches, teach back, and ongoing meetings with community providers.
Medication Reconciliation, Seven-Day Appointments Reduce Readmissions
Seton Health / St. Mary’s Hospital
Troy, New York
In 2008, at the start of the care transitions initiative at Seton Health/St. Mary’s Hospital, hospital leadership looked at what diagnoses were most likely to lead to readmission. Seton Health is a health system that includes a hospital and a home care agency, as well as a significant number of affiliated practices and clinics. Respiratory conditions—COPD, pneumonia, adult asthma—were found to have the highest rates.
The team started the initiative on a nursing unit populated mainly by high-risk patients with these and other conditions. The first priority was to establish a comprehensive, individualized discharge plan for the high-risk patients, which includes a 7-day follow-up physician appointment post-discharge, coordinated by case managers. Even when family members had to shift their schedules to accommodate physician appointments, they were grateful for the help, says Case Manager Margo Walsh-Perras, RN. The program is now house-wide.
Another key care transitions intervention at Seton has been the design and development of a cross-setting medication reconciliation process, involving close collaboration between hospitalists, hospital nursing, unit-based pharmacists, and home health agency nurses.
Prior to discharge, the discharge summary, discharge orders, prescription list provided by home health, lab results, and a list of active medications from the patient’s hospital stay are given to the physician to review, compare, and write prescriptions for discharge. The pharmacist performs the discharge medication reconciliation process and confirms that prescriptions are correct.
Before the first post-discharge home visit, the home health nurse reviews the patient’s final discharge medication list from the hospital electronic health record system and is able to address any medication-related questions directly with the pharmacist.
Medication discrepancies significantly decreased from 81% in the first 6 months of 2009 to 65% for the first 6 months of 2010, as a result of this intervention. System-level discrepancies decreased from 84% to 56% for the same time period.
Walsh-Perras emphasizes that the interdisciplinary nature of the care transitions team is one of the most important factors in reducing readmissions. Home care, case management, pharmacy, hospitalists, community-based primary care physicians, and others working together have helped Seton address a number of issues.
The team, facilitated by Jean Endryck, FNP-BC, NE-BC, director of palliative care and transitional care intervention coach, meets monthly to trouble shoot and discuss specific cases. Endryck’s expertise in palliative care management is an asset to the team and the program in addressing the care needs of patients with chronic, co-morbid health conditions.
Partnerships, Patient Education, and Follow-Up Pay Off
Saratoga Hospital
Saratoga, New York
Saratoga Hospital, which began work with IPRO on the Care Transitions initiative in 2008, has focused on heart failure patients, a high readmission population for this hospital.
One of the first things the hospital did was send letters to all physicians in the community, to engage them in the initiative right away. The care transitions team sought partnerships with others in the community: home health agencies, dialysis centers, nursing homes, and senior centers. “We wanted to create a safety net of partnerships to keep patients safe in the home setting,” says Cindi Lisuzzo, BS, RN, CCM, director of care management.
The care transitions program was piloted on a medical-surgical cardiac telemetry unit, incorporating daily rounding on patients, with special focus on HF patients. The interdisciplinary readmissions team, which includes the director of care management, direct care staff from the nursing unit, charge nurses, cardiologists, hospitalists, care managers, registered dieticians, the core measure specialist nurse, and pharmacists, meets monthly. In addition, Lisuzzo regularly discusses discharge issues with home care, and strategizes on how to help keep patients safe at home. Patient education and follow up are ongoing, and involve caregivers as well.
“In order to help high-risk patients, we have found that it is necessary to do care management outside the walls of the hospital. A family of healthcare professionals is needed to take care of our patients,” says Lisuzzo.
Communication between hospitalists and primary care physicians in the community is also critical, and information technology helps make this possible. On patient arrival in the emergency department, staff are able to determine from the hospital’s electronic medical record whether the patient has been readmitted within 30 days. The patient’s primary care physician receives an electronic notification from the hospitalist service when the patient is admitted. To improve communication, the hospitalists are starting a new process that includes a call back to the patient’s primary care physician that makes him or her aware of the admission and provides critical patient-related information to both parties.
Post-discharge patient follow-up is critical. Nurses and social workers also follow up with home care once the patient is discharged to discuss various aspects of care such as medication reconciliation, dietary guidelines, support systems, and a physician appointment within 7 days of discharge. Nurses are responsible for placing a follow-up phone call within 48 hours for all patients they discharge, and if there are issues requiring the involvement of a physician, nurse, or care manager, they are resolved within hours. This strategy has helped the team anticipate individual patient/family needs and has promoted increased patient satisfaction.
Using the “Four Pillars” of Coleman Model
Glens Falls Hospital
Glens Falls, New York
Glens Falls Hospital is located in a rural region of New York that has a very large geriatric population. At the start of the readmission reduction project, the hospital had a 19.35% all-cause 30-day readmission rate. That number has been reduced by 2%.
To address readmissions, the hospital and the Hudson Headwaters Health Network group practice first sought and received a grant to reduce the hospital’s 30-day readmission rate. The team began working with IPRO on the Care Transitions Initiative at around the same time and dovetailed the two projects. The grant incorporated many of the practices included within Dr. Eric Coleman’s CTI Model. The group developed a work team from Hudson Headwaters and Glens Falls hospitalists, as well as representatives from two referring home health agencies. The team drew on IPRO for resources, educational programs, tools, data collection methods, and high-risk discharge screening criteria (Figure 2).
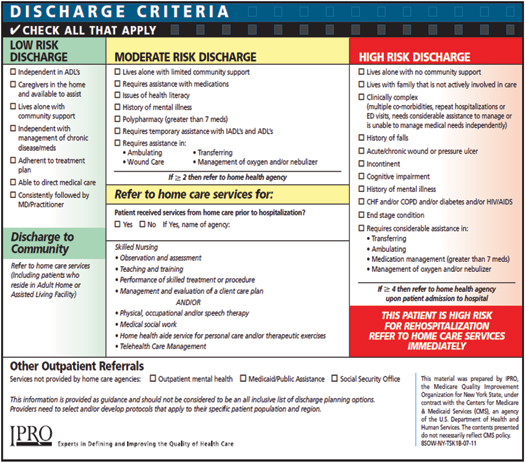
Figure 2. IPRO’s Discharge Planning Guide for referral to home healthcare services
Courtesy of IPRO
(click here to view a larger version in a separate browser window)
The project initially focused on patients with HF, acute myocardial infarction, and pneumonia. These criteria were soon expanded, however. “We found we needed to expand the target population because patients with other co-morbidities presented with similar, unmet needs,” says Chris Freire, LMSW, director, care management. “The average patient had 7 to 12 co-morbid conditions.”
The CTI coaches included a physician assistant from the Hudson Headwaters practice who educated hospitalized patients regarding the program and two care transition coaches to conduct home visits within 48 hours of discharge. Hospital-based care managers and physicians encouraged patient participation in this program.
Care Transitions Intervention staff visited physician practices and developed relationships with office personnel. This would prove key as they later worked to get expedited post-discharge appointments for patients. The team worked closely with the home health agencies to eliminate duplication and develop a patient-friendly “hand off” process that caused minimal disruption for patients and their families.
“What others can learn from our experience is that the consumer is always the constant,” says Freire. “The more we can engage the consumer, the more likely we are to succeed in developing an effective care transitions plan.”
In addition to work with the group practice and home health agencies, the hospital expanded its collaborative efforts to include nine regional skilled nursing facilities, as data analysis identified the SNF population as another source of patient readmission. This team adopted MOLST (Medical Orders for Life Sustaining Treatment) as a regional advanced directive standard. MOLST is a document that functions as an actionable medical order, which transitions with a patient through all healthcare settings and defines his or her wishes for life-sustaining treatment. The collaboration between the hospital and SNFs on MOLST facilitated resident/family education regarding treatment options.
IPRO instructed the SNFs on a variety of INTERACT (Interventions to Reduce Acute Care Transfers) strategies, which are designed to improve the quality of care by providing tools and resources that will help staff reduce avoidable acute care transfers. These practical tools aid in the early identification of residents’ change of status, guide staff through a comprehensive resident assessment and improve documentation when a change has been identified, and enhance communication with other healthcare providers on status changes. This training helped engage SNF staff in recognizing and communicating these changes, and fostered earlier communication and evaluation on whether hospitalization was needed.
The team supports a number of additional processes and interventions, including on-site care transitions liaisons from the two county home health agencies; scheduling follow-up physician appointments; and daily follow up and monitoring of all-cause 30-day readmissions by care managers.
Glens Falls Hospital and other regional providers continue to collaborate on a variety of initiatives, creating shared goals for its patient population, and implementing processes to support an improved community healthcare model.
Improvement Throughout Targeted Region
At the beginning of the Care Transitions Initiative, IPRO worked with each participating provider to identify patient populations at high risk for rehospitalization, and to conduct an organizational assessment of each provider setting. These analyses help determine which interventions and strategies would best address causes of readmission and opportunities to improve both internal and cross-setting systems and processes.
Throughout this initiative, a shared learning model has been in place across the individual communities and within all of the participating providers to support efforts to improve the patient/caregiver experience during transitions of care. Each of the Care Transitions hospital partners has taken an individualized approach to reducing hospital readmissions, yet each organization has demonstrated that collaboration and a focused effort can make a major difference for patients across the continuum of care.
Equally important, each provider community has established collaborative relationships that have enabled the respective providers to communicate more effectively, understand the challenges within one another’s setting, and continue to work on readmissions drivers on a cross-setting level. These collaborations are the foundation for sustaining and building on the improvements and successes within the program achieved to date.
This material was prepared by IPRO, the Medicare Quality Improvement Organization for New York State, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents do not necessarily reflect CMS policy. 9SOW-NY-THM7.2 11-17
Sara Butterfield serves as the theme lead for the IPRO CMS 9th Scope of Work Care Transitions Initiative. She may be reached at sbutterfield@nyqio.sdps.org.
Christine Stegel serves as a senior quality improvement specialist on the IPRO CMS 9th Scope of Work Care Transitions Initiative Project Team. She may be reached at cstegel@nyqio.sdps.org.
Shelly Glock serves as a quality improvement specialist on the IPRO CMS 9th Scope of Work Care Transitions Initiative Project Team. She may be reached at sglock@nyqio.sdps.org.
Dennis Tartaglia, a writer and communications consultant, is president and founder of Tartaglia Communications. He may be reached at dtartaglia@tartagliacommunications.com.
References
