Toyota Production System: Transforming Healthcare Organizations for the 21st Century
November / December 2009
![]()
Toyota Production System
Transforming Healthcare Organizations
for the 21st Century
A transformation to 21st century healthcare system is dramatically impacting patient safety and quality healthcare. New federal legislation will likely influence how healthcare will be managed and compensated in this new era. By promoting waste reduction, quality, accountability, pay-for-performance, evidence-based medicine, modernization/automation, workflow optimization, core measures, and transparency, the country is embracing the tenets of the Toyota Production System.
The Centers for Medicare and Medicaid (CMS; 2008) have added fuel to the fire by no longer paying for 11 “reasonably preventable never events,” leaving hospitals to foot the bill. This development and CMS pay-for-performance rewards are further incenting hospitals to minimize errors and maximize performance. Even with the government’s substantial investment in information and decision-support technology and other patient-safety initiatives to reduce these types of medical errors and oversights, healthcare providers are being pressured to do even more with even less than before. Many feel compelled to cut valuable staff and services. This is evidenced by the AHA Report on the Economic Crisis: Initial Impact on Hospitals (2008). The report also notes that hospitals, which employ 5 million people nationwide, could be facing uncertain times as their financial health falters and the ability to borrow funds for improving facilities and updating technology is squeezed.
Despite these seemingly insurmountable challenges, there is a viable solution that healthcare administrators can implement to optimize their existing, though dwindling, resources and enable their organizations to economize through greater efficiencies and waste reduction: the Toyota Production System (TPS).
The TPS Difference
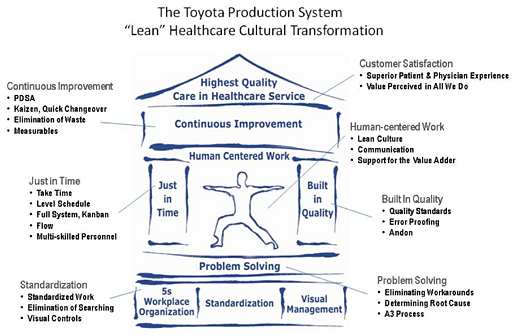
The Toyota Production System is a human-centered (versus tool-based) business performance improvement process that enables organizations to minimize waste and errors while optimizing performance and quality.
Like many quality solutions, TPS strives for the complete elimination of waste. Though many consider TPS synonymous with lean manufacturing systems (Lean) or just-in-time (JIT) systems, it is not. While Lean/JIT solutions revolve around a set of select applications or tactical tools that facilitate waste reduction and mandate organizational change, the Toyota Production System is a complete management system that focuses on people and on improving how they work together to reduce waste. TPS methodologies focus on every facet and all aspects of the value stream or patient/care provider experience. TPS — based strategies and solutions offer uniquely systemic and sustainable transformations at all levels of a healthcare organization.
And, though instituting a TPS-based transformation requires an initial investment by healthcare providers, TPS advocates insist that the rewards outweigh the drawbacks; the initial investment is typically recouped within the first year. They claim that implementing these solutions now will ensure hospitals and other healthcare providers ride out the healthcare revolution — and improve the quality of care in the process, ensuring systemic, sustainable improvement.
How TPS Works
By focusing on people and processes instead of tools and technologies, TPS offers healthcare providers and their staff the flexibility they need to respond to daily changes that emerge due to regulations, patient conditions, market conditions, and more.
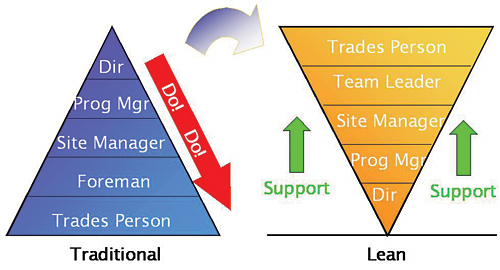
Where many quality solutions are essentially executive directives, with TPS, individuals and teams within the healthcare organization drive the TPS transformation. Participants identify and implement the tools and procedures that they determine will minimize waste and errors and improve the “flow” or smoothness of their work.
|
The focus of every process, investment, decision, and change is on establishing or improving the way that individuals closest to the patient are able to serve them. In implementations, the organization develops a system that makes problems readily apparent and then provides employees with the tools to identify and eliminate them. In healthcare this means first understanding what the patient needs, then rallying around those who provide patient services, and giving them the facilities, processes, systems, and leadership support they need to deliver this to every patient, every day. |
By improving the flow of work through the entire medical facility — and not focusing solely on a single department, process, or issue — TPS impacts all aspects of the value stream or total patient (and staff) experience from arrival to discharge.
Though flexible, the principles of TPS are also highly structured. This dynamic approach enables each TPS implementation to mould specifically to the individual culture of each organization.
Essential to this is the adoption and standardization of each organization’s best practices. By identifying and instituting the processes which consistently minimize all aspects of waste and/or errors and optimize patient safety and care, each hospital or healthcare organization assures greater efficiencies and patient outcomes.
Individuals trained in best practices then improve on their own jobs, processes, and the organization, as a whole, in a blame-free environment. Participants soon realize the benefits outweigh resistance or discomfort typically associated with organizational change. Individual teams meet and confer daily, documenting their processes, issues, and solutions. That information is shared with the department leaders who share with the administration and so on.
|
Originally intended as a means of ensuring smoothness in operations by having what is needed, when it is needed, and in the quantity and quality needed, JIT has more often become the mantra for reducing the cost of materials and expenses in the supply chain. Returning to the first premise of Operator Centered, JIT ensures that the organization provides employees, i.e. care providers, with what they require (information, knowledge, access, equipment, etc.) when they need it — to safely and efficiently serve each patient’s needs, every time, as part of the normal, standardized process. An example of JIT information would be providing the visual or verbal queues indicating room and nurse availability prior to calling patients back from a waiting room. JIT would include the processes that ensure room, surgical supplies, patient and provider readiness to ensure on-time starts in the OR. |
Organizational and process transparency emerges, and competition becomes a positive facet of the transformation. Departments strive to exceed industry and regulatory standards, area competitors, and even each other. Smart organizations encourage friendly competition with awards and incentives.
Fundamental in the evolution of the workplace is everyone’s ability to recognize normal from abnormal, and have the ability to do something about it. This “stop and look” approach minimizes errors and inefficiencies while quickly addressing and resolving issues as they arise.
Also key is organizing the workplace, especially a shared workplace (like the emergency room, an operating room floor/station, or specific department), and keeping it organized. Techniques such as Visual Management ensure that processes, progress, and problem-solving exist in a highly visible, shared workspace. Value Stream Mapping helps analyze the flow of patients, nurses, staff, samples, and results required to deliver a product or service.
|
In every aspect of the delivery of care, clear expectation and demonstrated capability is fundamental and essential to establishing confidence in ourselves, our peers, our patients, and our families that what we say will indeed occur. Whether assessing a patient or drawing and processing a sample, documenting, training, and ensuring compliance to this best known practice is the foundation upon which we can improve. Though situational change is a constant in the healthcare environment, process standards must be applied in all applicable areas to reduce the controllable variances and ensure regulatory compliance, patient and staff satisfaction, and outcomes. This by no means implies that a person is like a car, or the situation is always or ever “textbook.” What research repeatedly shows is that in a patient’s experience, nearly 80% of their time and interactions are not clinical in nature. That means most of the time, cost, effort, and experiences are related to process execution such as providing information, waiting, or being transported and are subject to error or delay, in and of themselves, or worse. With that in mind and a fair dose of reality, Toyota and medical practitioners alike must hone their ability to predict, recognize, remediate, and eradicate the very potential for these occurrences through a structured problem solving approach that is driven and utilized on the floors where problems occur. |
Additional systems and controls offer signals, cues, and visual aids to help workers better manage workflow, inventory and chain-supply management, and patient turnaround time with greater efficiencies and fewer errors or workarounds. Tasks become easier and more effective, and organizational morale and performance are enhanced as well. Increased efficiencies lead to better care and to better outcomes. Every change has a ripple effect, multiplying exponentially across the organization. Time gained by newly realized efficiency is time that staff can reinvest in better quality healthcare.
For the Toyota Production System transformation to succeed… hospital leaders, physicians, staff and even the patients must fully embrace the new processes. This engages and empowers workers to readily and eagerly participate in the transformation.
|
The most often cited element of TPS is continuous improvement (or Kaizen in Japanese). To ensure deep and continuous cultural transformation, change must involve people at every level. Therefore, hospital leaders, physicians, staff must relentlessly seek to identify small areas of improvement and fully embrace the new processes defined as part of the kaizen process. Once processes have been standardized and demonstrated with predictable results, the organization can focuses on raising performance of these standardized practices. |
Ironically, a successful Toyota Production System transformation ultimately makes the TPS solution provider obsolete to the very organization it transforms as it passes the reins to the transformed healthcare organization. Change is no longer a solution but a self-perpetuating circle of life, and excellence is measured by consistency, achieved by total involvement, institutionalized progressively by experience over years of calculated transformation. It starts with the next patient admitted or specimen drawn, the next triage in ER or recovering patient sent home.
Mike Olive is director of the Healthcare Performance Solutions Practice with RWD Technologies, where he has 17 years of first-hand experience in application and consulting in the adoption, training, and implementation of the Toyota Production System. Olive holds a bachelor of science degree from Boston University College of Engineering. He is an active member and contributor to American College of Healthcare Executives (ACHE), Association of periOperative Registered Nurses (AORN), Maryland Association of Healthcare Executive (MAHCE), and the American Hospital Association (AHA). Olive may be contacted at MOlive@rwd.com.
References