The Universal Bed Care Delivery Model: Facility Design and Operations Combine to Impact the Patient Experience
March / April 2007
The Universal Bed Care Delivery Model
Facility Design and Operations Combine to Impact the Patient Experience

![]()
The United States population is older than ever before, which places added and intensifying stress on our healthcare system. In fact, according to the Administration on Aging, the over-65 population currently accounts for one out of eight Americans, and by 2030, this population will more than double. The over-85 population is steadily increasing as well, resulting in 9 million elderly Americans, many of whom have a high incidence of co-morbidities and require increasingly complex care (Administration on Aging, 2006). This scenario also impacts the nursing profession. The average age of the typical nurse has increased to 47, a number predicted to increase as younger men and women consider a multitude of other professions. Furthermore, new medical technologies allowing less seriously-ill patients to receive more care in an outpatient setting compounds the problem, leaving only the sickest to be cared for on an inpatient basis (Stanton, 2004).
Care across the Continuum
The focus of healthcare professionals must always be safe, high-quality care for patients. The traditional “conveyor belt” approach, where patient location determines the level of care, can be a hindrance to receiving appropriate and timely treatment. When patients on a general medical-surgical floor become acutely ill, they are often cared for by staff not usually accustomed to intensive care patients until a critical care bed becomes available. On the other hand, a patient’s rehabilitation is not usually a priority when being cared for in an intensive care unit with other more critical patients while waiting for a telemetry or general care bed vacancy. The aggregation concept focused on intensive care, step-down, telemetry, and general medical-surgical care was more successful in the past when most patients did not have multiple acuity needs; however, now many patients require intensive care sometime during their hospitalization. In fact, estimates show that the continued growth in intensity of care requirements will increase the 10% to 13% of current critical care hospital beds to 20% to 30% in the near future (Anderson, 2004).
The universal bed/acuity-adaptable care delivery model is a concept based on the labor, delivery, recovery, post-partum (LDRP) care process, where patients stay in one room during their hospitalization with the appropriate level of care brought to them. Corazon has worked with multiple community hospitals initiating open heart surgery programs that have chosen to utilize this model of care delivery. These clients have consciously chosen this approach to patient care as recent entrants to the advanced cardiac services arena, oftentimes having the capabilities to choose a facility design and patient flow for new or expanded services. Often they are competing with well-established academic medical centers and other tertiary institutions with positive patient outcomes. To be successful in this highly competitive environment, they choose to implement the universal bed, believing that this care approach will lead to higher-quality patient outcomes, eliminate patient safety concerns that stem from multiple patient transfers, decrease overwhelming nurse-to-patient ratios seen on general care floors, and provide a healing environment. Tertiary hospitals, including all 10 physician-owned MedCath heart hospitals across the nation, utilize universal beds. In 2004, Corazon worked with The Ohio State University Medical Center (OSUMC) to open the Richard M. Ross Heart Hospital, the first full-service academic heart and vascular hospital in the nation. Non-cardiac hospitals have followed in the footsteps of these trailblazers, developing universal bed units focused on the care of general and vascular surgery, along with neurology and neurosurgery patients (Brown, 2006).
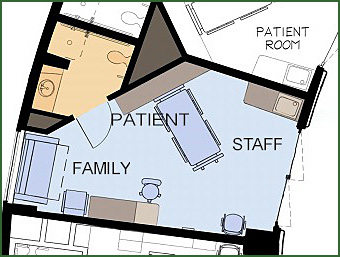
To successfully implement the universal bed care delivery model, the facility design and the operations and staffing approach must support the concept. The design of the universal patient room must safely accommodate the critical care needs of the ICU patient with space for high-tech equipment, adequate staff access to the patient, and an efficient room layout to decrease wasted staff motion during treatment, which can be accomplished with dedicated space for the staff and patient (Figure 1). The room must also meet the needs of a recovering/telemetry patient, with space for patient ambulation and family visitation. A focus on comfort and privacy, including separate space for family visitation without crowding the caregiver, are hallmarks of optimal universal bed room design.
![]()
Operationally, the universal bed unit is staffed by nurses able to provide for all of the patient’s care needs for the entire hospitalization — from the most intense, including hemodynamic monitoring and critical care therapies, to recovery needs such as progressive ambulation/rehabilitation and education — enabling the patient to be safely discharged. By providing care across the entire continuum, no longer does the patient with unstable vital signs in the general medical-surgical unit need to wait for an ICU bed to become available. Instead of focusing on the transfer process, nurses can continue to concentrate on the patient’s acute care needs. Some institutions cross-train all nursing staff in the universal bed unit to enable them to provide ICU and progressive recovery care; other institutions hire a mix of critical care and telemetry/general medical-surgical nurses, and then staff the unit to meet daily acuity needs. Hiring an integrated nursing staff (ICU and telemetry) is beneficial for institutions during the current nursing shortage, especially because telemetry nurses can be productive, tending to the progressive care patient while being oriented to the critical care patient.
The Inclusion of Family
For the universal bed concept to positively impact patient safety and quality outcomes, the facility design must support the operations approach promoted by the care delivery model. The universal bed concept’s focus on the inclusion of the family, with a dedicated zone for visitation, including sleeping accommodations, has the potential to reduce patient falls due to increased family involvement in patient care and recovery, as most falls occur in patients’ rooms when they are alone. Hospitals using the universal bed model of care delivery often have relaxed family visitation policies, supporting liberal visiting hours or overnight stays. We have seen the impact of enhanced family participation on customer satisfaction at OSUMC, as The Ross Heart Hospital’s latest patient satisfaction scores were the highest of all of the OSU hospitals at 85.3%, compared to 76.3% (Brown, Davis, & Moreland, 2006). Staff attributes this high level of patient/family satisfaction to the universal bed care delivery model’s focus on patient and family needs. Additional studies have shown that improved family involvement may also reduce patient stress and expedite recovery (Chaudhury, Mahmood, & Valente, 2005).
Universal Bed Impact on Patient Safety
The layout of a universal room incorporates principles that are not necessarily unique to the concept; in fact, these design elements can improve patient safety and quality outcomes with any care delivery model. For instance, more than 50% of all patient falls are related to the patient’s toileting needs (Hendrich, 2006). Because the universal bed room must accommodate the critical care as well as the progressive care patient, an outboard toilet is usually present. The bathroom located away from the hall allows unimpeded visualization of the patient. At The Ross Heart Hospital, as seen in Figure 1, the bathroom was creatively placed behind the bed to not only minimize the patient’s walking distance, but also allow even a patient who is wired to a critical care monitor safe access to the bathroom.
Because the universal bed (UB) concept focuses on enhanced family participation, UB rooms should be designed for private occupancy, a building trend reinforced by the 2006 American Institute of Architects (AIA) guidelines for the new construction of general medical-surgical beds. Furthermore, the single occupancy room decreases nosocomial infection rates, even when controlling for hand washing practices and air quality (Ulrich, 2003). Unfortunately, many institutions not utilizing the universal bed concept continue to operate multiple occupancy rooms, thereby raising infection rates and other unnecessary complications of an already serious hospitalization.
Institutions building universal bed units commonly elect to decentralize the nurse station, which can greatly impact patient safety as well. Nurses in universal bed units tend to care for a smaller number of patients with varying levels of care needs. One nurse may care for an ICU patient or an intermediate care patient, as well as one who is ready to be discharged; therefore, nurses work in fewer patient rooms, making the option of decentralized nurse stations between rooms possible. By decentralizing the nurse station, nurses spend more time in the rooms monitoring patients and providing care and less time walking to multiple destinations to obtain supplies and information. To truly un-tether the nurse from a central station, all technology and supplies must be available at these mini-stations, including computers to access patient information and documentation, wireless communication options to respond to patient call bells, phone options for reaching physicians and required personnel, medications, and other required supplies and equipment.
Nurse mini-stations are often placed between two patient rooms as seen in the cardiac universal bed unit at Clarian Health System’s Methodist Hospital (Hendrich, 2004). After decentralizing the nurse station, Clarian experienced a 75% decrease in patient falls. Desert Samaritan Medical Center in Arizona’s surgical universal bed unit placed mini nurse stations outside of the patients’ rooms as well, but in addition, also built four substations throughout the unit — set away from the hallway so staff could converse regarding patient issues in private (The Universal ICU, 2006).
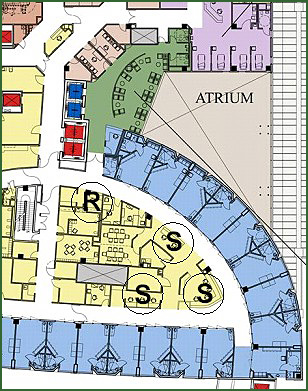
At OSUMC’s Ross Heart Hospital, different types of nurse support stations were built to accommodate the varying levels of patient acuity within the unit. Nurses utilize the well-organized mini station located in the patient room as seen in Figure 2. Electronic patient charts are located at these stations, along with supplies and medications locked in the movable supply cart. As the patient improves and requires more privacy, the nurse can utilize the multiple substations (S) for documentation and reporting (Figure 3). Because of the large size of the universal bed unit (30 beds), the nurse support areas are mirrored on both sides of the floor. One clerical/reception area (R) is provided for the entire unit with the goal of directing traffic for families, physicians, and ancillary departments passing through. Early outcomes from decentralizing the nurse stations are positive, as patients state that the unit, although large, is relatively noise-free.

![]()
Reduction of Patient Transfers
By caring for the patient in one room during their entire hospitalization, the universal bed care delivery model reduces the multiple inter-unit transfers linked to patient acuity needs and associated safety concerns. Patient transfers are often chaotic events, involving up to nine hospital employees from nursing to pharmacy, dietary, and clerical staff. With so many involved, the potential for miscommunication is high, which can result in errors from transcription mistakes to late-delivered drugs. Who knows how many of the more than 7,000 deaths related to medication errors can be reduced with the elimination of transfers (AHRQ, 2001). Supporting this claim is Clarian Health System’s Methodist Hospital cardiac universal bed unit, which experienced a 90% reduction in monthly transfers resulting in a 70% reduction in medication errors with implementation of the UB delivery model (Hendrich, 2004).
In addition to reducing the potential for medical errors, eliminating patient transfers elevates the entire patient care experience overall. In a past survey, 20% of all patients moving out of the intensive care unit were highly distressed regarding the new level of care. They experienced a noticeable decrease in monitoring by the nurses and an increase in the length of time required to obtain assistance. Patients who were accustomed to a large amount of support from the ICU staff become worried about the level of care they were going to receive in the telemetry unit (Leith, 1999). In an universal bed unit, patients often feel that the continuity of care offered with this type of delivery model results in enhanced care coordinated, which is supported by the high patient satisfaction scores at OSUMC’s Ross Heart Hospital, as compared to the rest of the health system (Brown, Davis, & Moreland, 2006).
![]()
Healing Environment
and Patient Outcomes
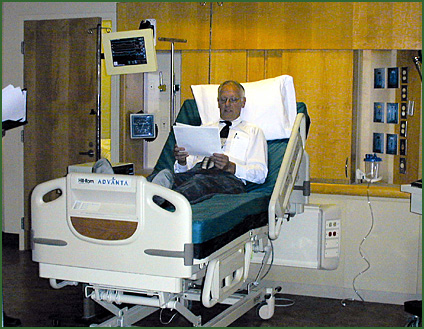
When designing the universal bed rooms, a goal of The Ross Heart Hospital was to offer high-tech care, such as heart transplants and ventricular assist devices, with academic medical center capabilities in a patient-focused environment to truly provide “world-class care.” Despite the critical care technology in every room, patients also experience a relaxing atmosphere with all of the “comforts of home” — soothing wood tones, muted lighting, and access to natural light, along with a view of the trees and outdoor green space common at the medical center campus (Figure 4). The objective to reduce patient stress levels and offer positive distractions to encourage healing is founded on evidence-based design research wherein post-surgical patients with views of trees experienced a lower length-of-stay and less use of pain medications than those patients overlooking a brick wall (Ulrich, 1984).

![]()
The universal bed rooms at The Ross Heart Hospital further reduce patient stress levels by allowing patients to assert some control over their surroundings. While designing the patient rooms, the architects evaluated the impact of medically necessary lighting versus reading lights and muted general lighting in the patient room. The design team made alterations as needed to increase the patient’s command of the hospital environment.
Meeting Patient Needs Through
Acuity-Based Staffing
Multiple studies have linked the ratio of total nurse staffing to patients to in-hospital mortality, controlling for patient characteristics (Sasichay, 2001). An increase in nursing hours has also been found to reduce patient length-of-stay and adverse outcomes (Needleman, et al., 2006). Traditionally, nurse-to-patient ratios are pre-set numbers based on the unit itself; but, depending on patient acuity, one nurse’s patient assignment may be more difficult than another’s. On general medical/surgical floors, nurse-to-patient ratios may climb as high as 1:7, whereas in a UB unit, staffing models are created to accommodate the ICU patient, intermediate patient, and the medical/surgical patient. Nurse assignments consider a patient’s clinical acuity, as well as the impact of prescribed nursing tasks and time-intensive treatments. One nurse in the unit may have a 1:3 patient assignment, while another may have a 1:5 patient load, depending on each of their patients’ needs. The total assignment acuity for each nurse will be equal since universal bed units utilize numeric calculations of patient severity to determine nurse-to-patient ratios, though ratios in universal bed units typically do not exceed 1:5 (Johnson, Brown, and Neal, 2003).
![]()
Conclusions
The universal bed care delivery model rises to the callenge of meeting the complex needs of sicker patients entering the hospital system with multiple comorbidities by elevating staff and unit capabilities. Patients can obtain the care they need based on acuity rather than the location where they are receiving care. The universal bed care delivery model is a holistic approach to patient care, not just focusing on clinical outcomes, but also addressesing psychosocial and family needs to augment patient health and wellness. Founded on evidence-based facility design, a healing environment will not only increase patient satisfaction, but can also expedite patient recovery. However, to enhance patient safety and outcomes, both facility design, as well as the operational approach, must support tending for the patient across the entire continuum of care. Institutions such as The Ohio State University Medical Center’s Ross Heart Hospital are paving the way for future care delivery models based on patient acuity versus the traditional nursing approach.
Katherine Kay Brown is currently a director of consulting at Corazon — The Heart & Vascular Experts. She gained her expertise in cardiovascular services through a variety of clinical and operational leadership positions focused on the entire continuum of cardiovascular care, and has been consulting for over a decade. An expert on the universal bed, Brown has worked at numerous hospitals to establish this innovative model, understanding its benefits from clients’ experiences and multiple research projects on the topic. Brown serves as assistant professor in graduate studies at Duquesne University and La Roche College in Pittsburgh, Pennsylvania, and as faculty at the American Healthcare Institute. She has held editorial board positions on both Critical Care Nursing Quarterly and Advanced Practice Nursing Quarterly and has published in a variety of professional journals on cardiac and critical care topics. Brown earned both her MSN and BSN from the University of Pennsylvania and may be contacted at kbrown@corazoninc.com.
References
Agency for Healthcare Research and Quality. (2001). Making health care safer: A critical analysis of patient safety practices. Evidence Report/Technology Assessment 43(Pub. No. 01-E058). http://www.ahrq.gov/clinic/ptsafety/
Anderson, T. (2006). Out with the old, in with the new in hospital room luxury. www.bizjournals.com/baltimore/stories/2004/06/14/focus2. Accessed August 15, 2006.
Brown, K. (2006). Impacting patient outcomes through design. Critical Care Nursing Quarterly, 29(4), 326-341.
Brown, K., Davis, R., & Moreland, S. (2006). The Richard M. Ross Heart Hospital facility design and functionality: Reinventing patient care delivery. The Center for Health Design Conference Ç Healthcare Design 06, Chicago, IL, November 5, 2006.
Center for Health Design. (2006). The universal ICU. www.healthcaredesignmagazine.com Accessed November 23, 2006.
Chaudhury, H., Mahmood, A, & Valente, M. (2005). Advantages and disadvantages of single versus multiple occopancy rooms in acute care environments. Environmental Behavior, 37(6), 760-786.
Department of Health and Human Services Administration on Aging. (2006). www.aoa.gov/prof/statisctics/statistics.asp. Accessed December 29, 2006.
Hendrich, A. (2006). Inpatient falls: Lessons from the field. Patient Safety and Quality Healthcare, 3(3), 26-30.
Hendrich, A., Fay, J., & Sorrells, A. (2004). Effects of acuity-adaptable rooms on flow of patients and delivery of care. American Journal of Critical Care, 13(1), 35-45.
Johnson, J., Brown, K., & Neal, K. (2003). Designs that make a difference: The cardiac universal bed model. Journal of Cardiovascular Management, 14(5), 16-20.
Needleman, J., Buerhaus, P., Stewart, M., Zelevinsky, K., & Mattke, S. (2006). Nurse staffing in hospitals: Is there a business case for quality? Health Affairs, 25(1), 204-211.
Sasichay, T. (2001). The relationship between nurse staffing and patient outcomes. University of Pennsylvania- Electronic Dissertations. Accessed at: http://repository.upenn.edu/dissertations/AAI3015367/
Stanton, Mark (2004). Agency for Healthcare Research and Quality, Research in Action, 14(Pub No. 04-0029).
Ulrich, R. S. (2003, October 10). Creating a healing environment with evidence-based design. American Institute of Architects Academy of Architecture for Health Virtual Seminar — Healing Environments.
Ulrich, R. (1984). View through a window may influence recovery from surgery. Science, 4647, 420-421.
The universal ICU. (2006). www.healthcaredesignmagazine.com. Accessed November 23, 2006.
