Technology – Advancing Patient Safety in Laparoscopy: The Active Electrode Monitoring System
May / June 2005
Technology
Advancing Patient Safety in Laparoscopy: The Active Electrode Monitoring System
In the past, use of monopolar electrosurgery in open surgical procedures involved the risk of external skin injury due to an alternate return path or compromised return electrode. In the 1970s and 1980s, perioperative nurses championed the adoption of technologies that prevented these problems (isolated generators and return electrode monitoring). As a result of their efforts, the risk of external skin injuries was almost completely eliminated. However, the introduction in the early 1990s of laparoscopic application of monopolar electrosurgery introduced the risk of stray electrosurgical burns (internal thermal burns to non-target tissue). This is an important issue for the perioperative staff to address; unlike skin injuries, stray electrosurgical burns during laparoscopy can be fatal.
As the advanced technology coordinator at Gwinnett Hospital System in Lawrenceville, Georgia, I have responsibility for evaluating new technology as well as the maintenance of Gwinnett’s laparoscopic service. This service has grown considerably over the last 15 years. One of the most difficult challenges is assessing our service lines in order to maintain cost with an emphasis on quality care and patient outcomes. The seriousness of the issue of stray electrosurgical burns convinced me that Gwinnett should take a proactive stance in ensuring patient safety during laparoscopic monopolar electrosurgical procedures.
In this article, I will explain why Gwinnett made the decision to implement active electrode monitoring and how we did it. In sharing this information, I hope that perioperative nurses will come to see the issue of stray electrosurgical burns as I do — an unacceptable risk to patient safety that we, as patient advocates, must actively take up in our hospitals.
Laparoscopic Monopolar Electrosurgery Today
Laparoscopy has had a significant impact on surgery in the past two decades. Currently, there are over 4.4 million laparoscopic procedures performed annually in the United States. At Gwinnett, we perform 3,600 laparoscopic procedures each year, including general, gynecological, and urological procedures. Gwinnett’s physicians are continually advancing their skill mix, and this volume is steadily increasing. The widespread increase in the use of laparoscopic techniques, and the fact that 85% of surgeons employ monopolar electrosurgery for laparoscopy (INTERactive SURVeys, 1993), means that more and more patients are being exposed to the risk of stray electrosurgical burns, with resulting complications including “vessel hemorrhage, and organ damage, perforation, and peritonitis” (Brill, et al. 1998, p. 222).
The electrosurgical unit (ESU), a standard surgical tool since the 1930s, is utilized to cut, coagulate, and vaporize tissue. Unfortunately, the majority of perioperative nurses and surgeons setting up, programming, and using the ESU have not been adequately educated to ensure safe practices during laparoscopy. While surgeons wanting to use a laser must be credentialed on the equipment — trained on specific wavelengths, in specific specialties, and proctored, by most hospitals, before using it independently — use of the ESU, with far more variables to control, requires no such credentialing.
The Problem of Stray Electrosurgical Burns
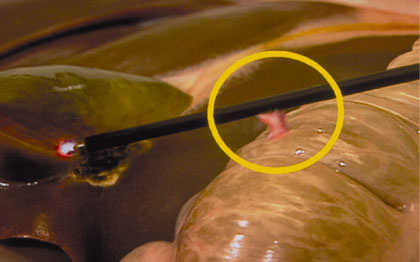
Every time a surgeon steps on the monopolar foot pedal during laparoscopy, the patient is at risk for a potentially fatal stray electrosurgical burn. Burns are caused by stray energy resulting from insulation failure (a break in the insulation surrounding the active electrode — see Figure 1) and capacitive coupling (an electrical phenomenon whereby current passes through intact insulation — see Figure 2). Insulation failure and capacitive coupling cause electrical current to come in contact with non-target tissue, causing unintended injury. Unlike external skin burns at the site of the patient return electrode, which are usually recognized immediately following a case, stray electrosurgical burns occur outside the view of the laparoscope, unbeknownst to the surgeon. “Unaware that electrical currents may be dangerously straying, the surgeon cannot intervene to prevent injury, let alone treat such injury” (Perantinides, et al., 1998, p. 49).
![]()

![]()
In a 1994 study, the Physician Insurers Association of America (PIAA) found that in “3 out of every 4 cases in which a [laparoscopic] injury [including thermal injury] occurred, it was not recognized prior to the conclusion of the procedure.” In fact, it may be several days before the patient who has suffered a stray electrosurgical burn returns to the physician with clinically significant symptoms. According to PIAA 2000 data, injuries related to the electrosurgical equipment account for 5.4% of all injuries that occur with laparoscopic surgery. Further complicating the situation is the fact that patients who have suffered from stray electrosurgical burns often present with what seem to be relatively normal postoperative symptoms: “low-grade fever, abdominal pain, and moderately elevated white blood count” (Harrell, et al., 1998, p. 1200). In a 1995 OBG Management article, Joseph S. Sanfilippo, MD, described the difficulty of diagnosing burns, warning surgeons that “when using a [monopolar] coagulation system, peritonitis may be the only evidence of a bowel burn with perforation” (p. 54). The fact that stray electrosurgical burns usually occur unnoticed, the fact that it takes a relatively long time for symptoms to appear after the procedure, and the fact that, upon presentation, those symptoms often seem unremarkable, all add up to dangerous delays in the diagnosis and treatment of stray electrosurgical burns.
Significant morbidity is associated with stray electrosurgical burns, including physical pain and suffering, a prolonged recovery, extensive follow-up medical treatment, and corrective surgeries that significantly affect a patient’s physical abilities and quality of life. The most feared complication of a stray electrosurgical burn is bowel perforation, resulting in leakage of the intestinal contents into the peritoneal cavity (i.e., fecal peritonitis). Bowel injury and resulting complications account for most of the fatalities associated with laparoscopic procedures. Even with modern “antibiotics, the mortality rate from peritonitis is approximately 25%” (ECRI).
The Laparoscopic Surgery subgroup of the Association of Trial Lawyers was founded in 1994, making it clear that laparoscopy was an area ripe for liability claims. In 1995, Tony Tsarouhas, Esq., a founding member, indicated that the group had “identified stray electrosurgery current during laparoscopy as a promising basis” for malpractice cases (p. 87). A 1999 article in the Journal of Healthcare Risk Management stated that “a physician might be deemed liable for stray energy burns — even those of which he or she is unaware — by virtue of … the failure to employ certain available safety equipment, given the known risks of thermal injury caused by stray energy released during laparoscopic electrosurgery. The article continued, stating that “the hospital might also be criticized for its failure to employ certain available safety equipment — such as active electrode monitoring” (Perantinides et al., p. 50).
Investigating Potential Solutions
Gwinnett is part of a buying group called Partners Co-op. This group consists of 6 hospital systems and over 24 facilities within the metropolitan area of Atlanta, Georgia. The General Operating Room Advanced Technology steering committee is a task force made up of members with both clinical and financial backgrounds. This group meets routinely to evaluate products and equipment and to simultaneously assess issues of cost and clinical outcome. As the committee chairperson, I informed my fellow members about the active electrode monitoring (AEM) system, which prevents stray electrosurgical burns by preventing stray energy. I had attempted implementation of active electrode monitoring several years prior, but at the time, clinical literature, limited number of laparoscopic procedures, and references did not support the financial investment from the perspective of the hospital administration’s budget (a common situation that, as clinicians, we are all faced with resolving). As the laparoscopic volume grew and the various types of procedures diversified in severity and techniques, I felt that the AEM technology could be justified both clinically and financially. The Partners General Operating Room Advanced Technology Task Force decided to evaluate the AEM system as well as recommend two other potential solutions (neither of which are fail-safe):
- Establish a hospital policy to visually inspect each instrument before and after each procedure and record the results in the patient’s perioperative record.
- Use a device designed to test insulation before and after each procedure and record the results in the patient’s perioperative record.
- Use active electrode monitoring (AEM) technology designed to dynamically monitor for stray electrosurgical energy and turn off the electrosurgical unit in case of insulation failure.
The following criteria were used in the evaluation process:
- Was it fail-safe?
- Was it cost-effective?
- Would it affect the time spent in the OR?
- Would it affect the surgeon’s clinical practice/technique?
- What did the laparoscopic community have to say about it? (Society of Laparoendoscopic Surgery, Association of Operating Room Nurses, American Society for Healthcare Risk Management, ECRI/Health Devices).
Option #1:
Visual Inspection
One of the two main causes of stray electrosurgical burns in laparoscopy is insulation failure. Conventional monopolar laparoscopic instruments contain a single layer of insulation.
Manufacturers of conventional instruments warn hospitals that when this insulation fails, it poses a serious threat to the patient; they say it is the hospital’s responsibility to inspect and maintain instruments. Unfortunately, it is virtually impossible to track instruments on a case-by-case basis. Most hospitals have no formal policies or procedures in place to ensure that the surgeon is supplied with an instrument free from insulation defects for each procedure. Over 500 surgeons surveyed at a meeting of the American College of Surgeons (ACS) were asked if they had ever “seen or heard of insulation degradation on monopolar electrosurgical probes.” Seventy-one percent of respondents answered “yes” (INTERactive SURVeys).
We wondered if it was feasible to demand that the biomedical engineering department at Gwinnett assume this responsibility. We also debated the merits of a hospital policy that would hold the surgeon accountable, requiring him or her to perform a visual inspection of instruments before each procedure. But in the end, we realized that placing this responsibility on biomedical engineers and surgeons was not appropriate, and, furthermore, visual inspection wouldn’t solve the problem of stray energy for three reasons:
The smaller the insulation defect — to the point of being invisible to the naked eye — the more dangerous it is. Microscopic insulation defects can concentrate the current density transferred to nearby non-target tissue, increasing the chance of a severe internal burn.
Visual inspection does not prevent insulation failure from occurring during surgery, as a result of the stress of high voltages or contact with the sharp edges of other laparoscopic instruments. The temperature of electrosurgical current can be up to 700C. The resting temperature of tissue is 32C, and tissue death occurs at 44C. If an insulation defect occurs during a procedure, the surgeon will not notice a change in the current delivered at the tip.
Visual inspection does not prevent capacitive coupling from occurring during surgery. Capacitive coupling can transfer current to nearby non-target tissue through intact insulation. In short, visual inspection, done by anyone, was not the answer.
Option #2:
Test Insulation Before and After Each Procedure
This product is a wand, used on the sterile field, connected to a sensing device. The wand is passed over a laparoscopic instrument before and after surgery to detect insulation failure. It can detect insulation defects that are invisible to the naked eye, but does nothing to prevent insulation failure or capacitive coupling from occurring during surgery. While the committee generally agreed that verifying whether or not an instrument had intact insulation before the procedure was better than not at all, the fact remained that it did not provide continual monitoring, and that was not enough protection for the patient. In fact, the manager of Gwinnett’s central processing department became alarmed when this device was used on some laparoscopic trays in for cleaning, and 3 out of 9 instruments were found to have insulation failure. That incident was proof enough for Gwinnett’s perioperative management team. We concluded that this technology was not an option.
Option #3:
Active Electrode Monitoring (AEM) Technology
Active electrode monitoring is a system in which shielded and monitored instruments continuously direct stray energy, the cause of stray electrosurgical burns, away from the patient via a protective shield.
In the event insulation failure occurs or capacitively coupled energy reaches dangerous levels, the electrosurgical unit (ESU) shuts down automatically and the surgical staff are alerted. With the AEM system, the patient is never at risk for stray electrosurgical burns due to insulation failure and capacitive coupling.
AEM technology is fail-safe, cost-effective, and does not significantly affect the surgeon’s clinical practice/surgical technique or time in the OR. Additionally, active electrode monitoring has received favorable views from the laparoscopic community. In 1995, ECRI/Health Devices tested the first generation of active electrode monitoring and rated it “Acceptable” (meets all major performance and safety criteria and has no serious shortcomings), stating that:
we … prefer it over other protective measures because we believe that it is the most effective means currently available of minimizing the potential for patient injuries due to active electrode insulation defects or capacitance (ECRI, 1995, p.18).
In a 1995 technical bulletin on electrosurgical safety the American Association of Gynecologic Laparoscopists suggested their members “consider active electrode monitoring” (p. 6). In a 1998 article appearing in the Journal of the Society of Laparoendoscopic Surgeons, Brill et al. stated that “active electrode monitoring (AEM) should be strongly considered for all laparoscopic monopolar electrosurgical procedures” (p. 224). In 1999, an article appearing in the Journal of Healthcare Risk Management recommended “the use of active electrode monitoring technology to shield electrosurgical instruments and monitor for stray current” as a way to “help reduce electrosurgery injuries” (Perantinides et al., 1998). Finally, in 1999, our own AORN published their Recommended Practices for Endoscopic Minimally Invasive Surgery, stating that “use of active electrode monitoring devices minimizes chance insulation failure and capacitive coupling” (p. 227).
Justifying a New Product Acquisition
Purchases involving capital are difficult to justify, especially when a hospital is under pressure to control costs. A new product acquisition that involves capital expenditure is even more difficult to justify, although active electrode monitoring promised to manage a significant patient safety risk. As a patient advocate, I believe that a perioperative nurse should practice according to his or her good judgment, not according to the pressures of liability. Again, with the large volume of laparoscopic procedures performed at Gwinnett, we felt strongly that our decision to purchase and implement active electrode monitoring shouldn’t wait until patient injury occurred. We needed to protect all of our patients before any one of them was injured.
Surprisingly enough, the cost justification for AEM technology was relatively easy. Through attrition, laparoscopic instruments are replaced yearly. The average life expectancy of a reusable instrument is one year, and institutions on an average use their equipment much longer. At Gwinnett we replaced our worn and defective instrumentation with reusable AEM instrumentation, which, in our case, actually reduced our overall cost per procedure. Use of AEM instruments eliminates the chance of catastrophic patient injury from instrument insulation failure, thereby reducing the hospital’s liability exposure in laparoscopy. Active electrode monitoring is the only technology recognized by ECRI/Health Devices that we, as perioperative management, could have used that would allow us to say we had done everything in our power to protect that patient during the time he or she spent in our OR.
The Decision to Standardize on Active Electrode Monitoring (AEM) Technology
After reviewing all the information with our risk manager, administrative team, and physician-based committees, it became evident to us that perioperative management had the utmost responsibility for the procurement and maintenance of operative devices. As a patient advocate, the perioperative nurse has the power and the opportunity to protect patients from the danger of stray energy burns. Gwinnett Hospital System’s perioperative management team made the final decision to implement AEM technology to optimize patient outcomes. We felt then and feel today that we made the right call and fulfilled our professional responsibility to protect our patients. To support the decision of the management team, the General Operating Room Advanced Technology steering committee also voted on the implementation of the technology.
After we decided to standardize on AEM technology, we were faced with the task of implementing our decision. We had already concluded that active electrode monitoring was transparent to the surgeon — in other words, it did not impact the surgeon’s clinical practice/surgical technique. 5mm AEM instruments looked and functioned like the conventional instruments our surgeons were used to using. Therefore, we decided that active electrode monitoring did not require a clinical evaluation. The decision to use AEM technology was a purely perioperative decision to optimize patient outcome by ensuring patient safety.
Implementation of Active Electrode Monitoring (AEM) Technology
The logistics of implementation were quite simple; we replaced our conventional electrified instruments with AEM instruments. We did not throw out the conventional instruments, keeping them instead for dissecting and grasping, but we did remove and discard the black monopolar cords that went with them so that they could not be activated. Four centers were involved, and implementation at each occurred a week apart. We sent informative letters to our physicians, and we also informed Gwinnett’s physician-based committees about the imminent conversion to active electrode monitoring. Again, we were proceeding based on the idea that this was not an evaluation, but a conversion. Furthermore, it was a conversion that did not affect clinical practice. Central processing and all perioperative staff were in-serviced on the processing and handling of AEM instruments and equipment. Signs were placed strategically throughout our operating rooms. Champions were staffed in all the initial procedures to troubleshoot problems and be available for staff and physician questions. The conversion was successful and was completed in 60 days. We are now preparing to launch a marketing/public relations effort to educate and inform our patients and the community that our facility, through our AEM implementation, is maintaining the highest level of patient safety possible.
After Implementing Active Electrode Monitoring (AEM) Technology
At our hospital, active electrode monitoring has been in place for approximately one year. Approximately 200 surgeons on our staff were quick to agree with our perioperative decision to be proactive in the elimination of a known risk to patient safety during laparoscopy. We had taken the guesswork out of detecting stray energy due to insulation failure and capacitive coupling, and they recognized that we improved overall confidence in the surgical staff. Use of active electrode monitoring technology at Gwinnett has actually made minimally invasive surgery more accurate by guaranteeing that 100% of the electrosurgical current is delivered where the surgeon intends it to be delivered. In this way, active electrode monitoring has helped both our surgeons and our hospital to be more productive. We have changed our perioperative record to document that active electrode monitoring was used on each patient. This we believe will assist Gwinnett with our next JCAHO audit to reflect that we have taken proactive action to meet the Revision to Joint Commission Standards in Support of Patient Safety and Medical/Health Care Error Reduction (effective July 1, 2001).
References
American Association of Gynecologic Laparoscopists Technical Bulletin Committee. (1995 January). AAGL Technical Bulletin: Electrosurgical Safety.
Association of Operating Room Nurses. (2004). Standards, recommended practices, and guidelines.
Brill, A. I., et al. (1998). Patient safety during laparoscopic monopolar electrosurgery — Principles and guidelines. Journal of the Society of Laparoendoscopic Surgery 2(3).
ECRI/Health Devices. (1995). Guidance Article: Evaluation of Electroscope Electroshield System 24(1).
ECRI/Health Devices. Clinical Perspective: The Risks of Laparoscopic Electrosurgery.
Harrell, G. J., et al. (1998). Home study program: Minimizing patient risk during laparoscopic electrosurgery. AORN Journal 67(6).
INTERactive SURVeys, Inc. Barrington, Illinois. Conducted at American College of Surgeons (ACS) Convention. October 11-14, 1993. Sponsored by American Hydro-Surgical Instruments.
Laparoscopic Surgery Update. (1995). Lap electrosurgery targeted by malpractice attorneys. 3(8).
Perantinides, P. G., et al. (1998). The medicolegal risks of thermal injury during laparoscopic monopolar electrosurgery. Journal of Healthcare Risk Management 18(1).
Physician Insurers Association of America. (2000). Laparoscopic injury study. Retrieved from http://www.piaa.us/storefront/SearchResult.aspx?CategoryID=12
Physician Insurers Association of America. (1994 May). Laparoscopic procedure study.
Sanfilippo, J. S. (1995 November). Avoiding complications at laparoscopy. OBG Management.
