Step Up Your Game: Staying Compliant With Joint Commission Hand Hygiene Requirements
By Ron Chappuis
When you think of your healthcare organization, what’s the first word that comes to mind? If you’re among the clear majority of healthcare organizations whose real hand hygiene compliance rates average 50% or less, The Joint Commission (TJC) has one word for you: deficient.
Starting January 1, 2018, TJC began citing observation of healthcare workers failing to perform hand hygiene during patient care with a “deficiency.” Previously, an individual failure like this was not cited if the facility had a hand hygiene compliance program in place. While TJC has always recognized hand hygiene compliance as an essential element of patient safety, this significant change will affect hospitals accredited by TJC and increase focus on hand hygiene behavior by all staff involved with patient care.
Bottom line: This new focus on compliance will deliver increased patient safety, enhanced quality of care, and improved economic outcomes. And all of these fit right in with the drive for healthcare organizations to achieve high reliability.
Time for change
With TJC’s renewed emphasis on compliance, 2018 could prove to be a banner year for hand hygiene. So far, there has been real momentum in the healthcare community to recognize that by following current guidelines and standards, and by striving for 100% hand hygiene compliance, a significant reduction in healthcare-associated infections (HAI) and zero preventable deaths by 2020 is a real possibility (Patient Safety Movement Foundation, 2018).
Studies have shown that hand hygiene compliance plays a critical role in reducing HAIs. In fact, according to the latest HAI Progress Report from the Centers for Disease Control and Prevention, when healthcare professionals actively engage in infection prevention measures, including effective hand hygiene protocols, it’s possible to reduce the rates of certain HAIs by more than 70% (Centers for Disease Control and Prevention, 2016).
But hand hygiene can prevent HAIs only if it’s followed consistently—and in the current healthcare climate, actual hand hygiene compliance rates are estimated to average 50% or less, meaning a vast amount of avoidable harm still takes place in healthcare settings worldwide (McGuckin, Waterman, & Govednik, 2009). This is clearly unacceptable in TJC’s view. In its January 2018 statement, the accreditor said it’s widely known that hand hygiene is the most important intervention for preventing HAIs, and while HAIs have multiple causes, failure to perform hand hygiene should no longer be one of them (The Joint Commission, 2017).
There are many ways to encourage healthcare workers to comply with hand hygiene protocols, such as holding daily huddles with staff, posting reminders in breakrooms, providing quality hand-healthy products, and implementing electronic monitoring systems. To establish a culture of safety, implementing an effective hand hygiene performance improvement program is vital.
However, one question remains: If healthcare facilities and workers already know the critical role proper hand hygiene protocol plays in patient safety, quality care, and high reliability, then why is compliance an issue?
Changing a behavior: Establishing a culture
Creating a culture of compliance within a healthcare organization requires a fundamental behavior change from top to bottom, from board members and hospital executives to environmental services staff. This includes taking full responsibility for major changes like zero harm, as well as valuing when errors are identified by “owning” them and not just supporting the culture change.
There have been many theories on how to encourage a culture of hand hygiene compliance within a healthcare facility, but perhaps the most promising is from the Patient Safety Movement Foundation (PSMF), which recommends an overall shift in the safety culture. This starts by building acceptance of the hand hygiene process changes with those who will be charged with implementing and sustaining the new processes, and then establishing a method of accountability to sustain the changes.
Similarly, the Joint Commission Center for Transforming Healthcare’s Targeted Solutions Tool (TST) also suggests a process to improve hand hygiene acceptance and compliance that mirrors the recommendations of the PSMF:
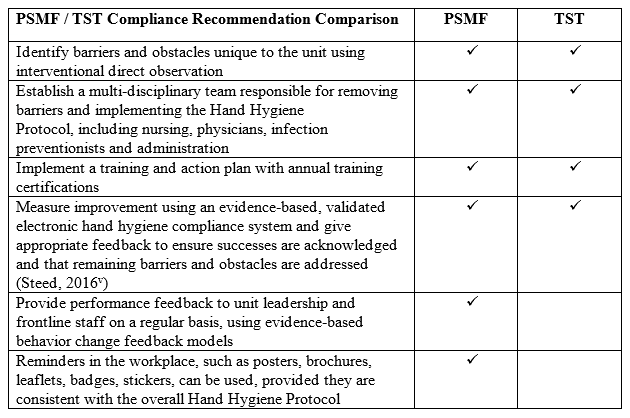
Interestingly, both organizations recommend using evidence-based, validated electronic hand hygiene compliance systems for measuring compliance as well as sharing feedback with staff to ensure success. These systems provide clinical, evidence-based data, which is critical to training employees on appropriate hand hygiene behavior.
The effectiveness of electronic monitoring systems, as well as their ability to produce clinically important organizational change and improved patient safety, was illustrated in a 2016 study published by Kelly et al. in which researchers found a significant correlation between improved hand hygiene compliance due to electronic monitoring and reductions in methicillin-resistant Staphylococcus aureus (MRSA) infection rates (Kelly, Blackhurst, McAtee, & Steed, 2016).
However, not all systems monitor for hand hygiene during direct patient care, so be sure your organization selects a system that follows the World Health Organization’s “My Five Moments” to stay in compliance with TJC’s requirements. Badge systems, for example, only monitor entry and exit from patient rooms; they do not monitor activity within the room during patient care.
Maintain a culture of compliance
Establishing a culture of compliance is important, but maintaining that culture leads to increased patient safety, improved quality of care, higher reliability, and better clinical and economic outcomes. Some strategies and tactics to help maintain a culture of safety include:
- Top-down commitment. Employees are more likely to comply with hand hygiene protocols if they witness hospital leaders doing the same. Encouraging leadership to demonstrate commitment by practicing good hand hygiene, as well as regularly communicating its importance to staff, can help foster a culture of compliance.
- Daily huddles. Multilevel communication works to disseminate important health and safety information. Implement daily meetings or “huddles” to encourage communication between all levels of hospital staff. Take this time to also discuss and report potential safety issues, as well as provide an overall awareness of what’s happening throughout the organization.
- Tracking and reporting. Electronic monitoring programs provide powerful information that healthcare professionals can use to understand, track, and improve their hand hygiene performance. The data can complement the use of observations for real-time coaching and feedback. These systems also provide reliable data that, when shared with healthcare staff, can help them visualize the direct impact hand hygiene has on lowering incidences of infection. Without accurate data, this is not achievable. In fact, when compliance is dramatically overstated—as it typically is, sometimes by as much as 350%, with direct observation by so-called “secret shoppers”—leadership is lulled into a false sense of complacency (Srigley, Furness, Baker, & Gardam, 2014).
- Hand-healthy products. Maintaining healthy hands gives greater protection for healthcare workers because damaged, broken, and open skin is vulnerable to pathogenic infection. Educate healthcare staff about the importance of skin health and the steps they can take to ensure it. Discussions should focus on which products should and shouldn’t be used and why, the proper techniques for application, and the recommended frequency of use.
- Reminder collateral. Reinforce hand hygiene education efforts with hospital staff by posting reminders in staff breakrooms, restrooms, locker rooms, and other high-visibility locations. Reminder discussions should also take place during every meeting, whether individual or all-staff.
- Sharing of results. Share consistent and reliable data correlating HAI rates to hand hygiene compliance rates with employees so they can visualize the direct impact of hand hygiene on lower incidences of infection. Clinically validated data lends credibility to the message and has been shown to lead to higher performance.
Even with TJC cracking down on hand hygiene compliance, avoidable HAIs and deaths may still take place in healthcare settings nationwide due to simple handwashing failures. Instead of focusing on these TJC audits as a negative, view them as an opportunity to review your organization’s hand hygiene compliance program for gaps and raise your healthcare facility to the next level.
Ron Chappuis has worked as a business leader, researcher, innovator, and strategist in the healthcare products markets for over 30 years. During this period, he has been a significant contributor to advancements in the area of infection prevention and control. Chappuis is currently the vice president of North American marketing for DebMed, a part of SC Johnson Professional.
References
Centers for Disease Control and Prevention (2016). National and state healthcare-associated infections progress report [updated March 2016]. Retrieved from https://www.cdc.gov/hai/surveillance/progress-report/index.html
The Joint Commission (2017, December 20). Effective Jan. 1, 2018: Individual hand hygiene failures to be cited under IC, NSPG standards. Joint Commission Online. Retrieved from https://www.jointcommission.org/issues/article.aspx?Article=IlZJaLJCiRBZC2IRvnKkJTqEEU2n1Rxv3fqmsKqKPb0%3D.
Kelly, J. W., Blackhurst, D., McAtee, W., & Steed, C. (2016). Electronic hand hygiene monitoring as a tool for reducing health care-associated methicillin-resistant Staphylococcus aureus infection. American Journal of Infection Control, 44(8), 956–957. doi:10.1016/j.ajic.2016.04.215
McGuckin, M., Waterman, R., & Govednik, J. (2009). Hand hygiene compliance rates in the United States—a one-year multicenter collaboration using product/volume usage measurement and feedback. American Journal of Medical Quality, 24(3), 205–213. doi:10.1177/1062860609332369
Patient Safety Movement Foundation (2018). Patient Safety Movement | ZERO preventable deaths by 2020. Retrieved from https://patientsafetymovement.org
Srigley, J. A., Furness, C. D., Baker, G. R., & Gardam, M. (2014). Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: A retrospective cohort study. BMJ Quality & Safety, 23(12), 974–980. doi:10.1136/bmjqs-2014-003080
Steed, C. (2016, May). Use of the Targeted Solutions Tool and electronic monitoring to improve hand hygiene compliance. Paper presented at the 2016 SHEA Conference, Atlanta, GA.
