Six Sigma: Reducing Surgical Site Infections Through Six Sigma & Change Management
July / September 2004
![]()
Six Sigma
Reducing Surgical Site Infections Through Six Sigma & Change Management
![]()
Hospital-acquired infections represent a significant patient safety concern, causing increased injury, mortality, and healthcare costs. In 2002, the Centers for Medicare & Medicaid Services (CMS) and the Centers for Disease Control and Prevention (CDC) launched a national quality improvement project aimed at reducing the occurrence of postoperative surgical site infections (SSIs).
The CMS/CDC Surgical Infection Prevention Project (SIPP) focused on preventing SSIs by improving the selection and timing of prophylactic antibiotic administration. Five common procedures were targeted: cardiothoracic, vascular, colon, hip or knee replacement, and vaginal or abdominal hysterectomy.
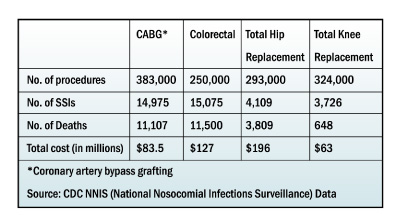
![]()
This is an important public health issue, since the CDC estimates that 500,000 surgical site infections occur annually in the United States, out of approximately 30 million surgical procedures performed. For each infection, patients may spend an additional seven days in the hospital and incur an extra $3,000 in charges. They are also 60% more likely to spend time in an ICU, five times more likely to be readmitted to the hospital, and have twice the incidence of mortality.
As a result of the national project, new guidelines for the use of antibiotics to prevent SSIs were published, acknowledging that surgical site infections can be largely avoided if hospitals administer the right antibiotics, at the right time, and in the right dosage. The SIPP collaborative agreed that care processes for surgical patients should include:
- Antibiotics administered within 1 hour before surgical incision (Due to the longer infusion time required for vancomycin, it is acceptable to start this antibiotic, when indicated for beta-lactam allergy, within 2 hours prior to incision.)
- Prophylactic antibiotic consistent with current recommendations
- Discontinuation of prophylactic antibiotics within 24 hours after surgery
Unfortunately, only 55 percent of surgical patients in the United States currently receive antibiotics within an hour of surgery, and usage is continued for an average of 40 hours following a surgical procedure. Clearly, healthcare providers will need to implement better process control in order to meet the new standards.
Reaching consensus on guidelines, however, is just the first hurdle. In March 2002, Charleston Area Medical Center (CAMC) in West Virginia decided to take the next step through a Six Sigma project to reduce the risks of postoperative infections. Since 2000, the hospital had been using Six Sigma methodology and related techniques to achieve cultural change and had successfully completed a variety of projects across the organization.
Scoping the Project
To improve existing processes, Six Sigma uses a five-phased DMAIC method that helps to Define, Measure, Analyze, Improve, and Control process capability. For this project, CAMC assembled a multidisciplinary team including two surgeons, an anesthesiologist, an epidemiologist, safety personnel, the chief of CRNAs, and two Six Sigma specialists (one black belt and one green belt).
The team began by setting parameters and establishing measurable goals. An essential part of any Six Sigma project involves determining what is in scope or out of scope, and identifying objectives. Overlooking this aspect can cause a project to derail at a later point or deliver disappointing results.
The CAMC team decided their project would encompass the immediate pre-operative phase and extend to 30 days post-discharge for colon and vascular surgery patient populations only. Since the focus was on prophylaxis, patients already on antibiotics for any reason prior to surgery would not be included in the scope of the project.
The following indicators would be measured for antibiotic administration:
- Recommended antibiotic appropriate for specific surgery.
- Dose administered at the right time (0-60 minutes prior to incision, with the exception of vancomycin, which is in the 0-120 range). Antibiotic must be completely infused prior to tourniquet inflation.
- Administration of right dose based on weight. Medication and antibiotics are not “one size fits all.”
- Appropriate intraoperative re-dose if the surgery is longer than 240 minutes.
- Discontinuing the prophylactic antibiotic within 24 hours of surgery. The development of resistant organisms has been linked to excessive use of antibiotics. If patients receive the antibiotic past 24 hours, there must be a documented valid reason for the therapeutic antibiotic.
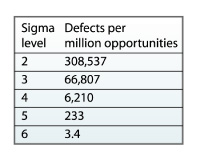
The object of Six Sigma is to limit errors or defects to 3.4 per million opportunities, and in this project a “defect” was defined as any variable not meeting each antibiotic indicator. At the beginning of the project, the process was actually at “0” sigma, with 660,828 defects per million opportunities.
Define and Measure
During the initial phases of the project, the team developed a detailed business case and collected data on the percentage of surgery patients acquiring an infection during their hospital stay. Critical factors such as mortality and morbidity rates and length of stay were also taken into consideration.
 |
|
Capturing the data was quite arduous, but the project team took steps to mitigate the difficulties associated with this process. The Black Belt and Green Belt developed an abstraction tool along with detailed guidelines, and educational sessions were provided for everyone to help ensure consistency. Initially, several of the registered nurses on the team abstracted the electronic medical records retrospectively. Eventually, however, with complete support from administration, a nurse was dedicated to the monthly task. Initial Gage R&R revealed variation in the measurement process, but further education resolved this issue. The data were entered into a database and then imported into Minitab for statistical analysis. Quarterly results were sent to each surgeon and anesthesiologist with individual as well as aggregate data.
 |
|
Measuring the current process provided interesting information. Baseline data indicated that many patients arrived in the pre-op holding area of the OR without a written antibiotic order. Additionally, antibiotics were often administered either too early or too late, and weight-based dosage was also an issue. Finally, patients undergoing procedures longer than 4 hours (6 hours for vancomycin administration) did not routinely receive an appropriate re-dose of antibiotic.
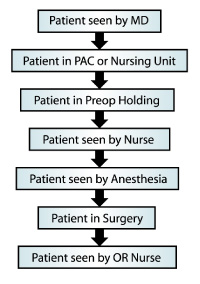
The prophylactic antibiotic process map shown in Figure 3 was created during the Measure phase to illustrate patient flow and contact within the hospital. It reveals multiple opportunities for ensuring the patient receives the right antibiotic and other appropriate interventions.
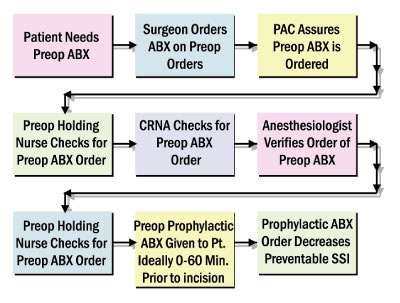
Figure 4 illustrates the ideal process designed to ensure that the antibiotics are administered correctly and at the right time.
Analyze and Improve
In the Analyze and Improve phases, statistical tools such as FMEA (Failure Mode and Effects Analysis) and fishbone diagrams were used to identify critical factors impacting infection rates. Data analysis revealed significant variation among surgeons and anesthesiologists. Processes for each were reviewed to uncover best practices that could be adopted.
Root cause analysis revealed numerous variables. Even if the surgeon ordered the antibiotic early enough, there could still be delays in the operating room preventing timely administration. Although valid data certainly helped to make the case for change, cultural techniques such as stakeholder analysis were also instrumental in creating a shared need.
Applying such techniques helped the team gain acceptance from the staff as they began to develop new procedures and implement the following process improvements:
- Development of database for indicator monitoring reporting.
- Revision of pre-operative order set to include recommended antibiotics and weight-based dosage.
- Education of physician office staff, CRNAs, anesthesiologists, surgeons, residents, and OR staff.
- Development of physician report card.
- Having RN staff and anesthetists prompt the physician for an antibiotic order if the patient arrives in the pre-operative holding area without one or with one that is not recommended.
- Posting appropriate antibiotics and doses for colon and vascular surgeries beside each patient and nurse’s station, in the medication preparation area, and in key locations within the surgical area.
- Using error-proofing techniques to revise the pre-operative physician order form to include recommended antibiotics with proper doses and re-dose times.
In addition, the team developed a “Who-What-When” (WWW) plan containing over 200 separate tasks, and provided staff with a new post-op order set allowing them to quickly check the right boxes instead of writing everything out.
Visual reminders were placed in the operating room prompting the staff when it is time for a re-dose of the antibiotic. The team also created posters, signs, and a puzzle with the indicators written on it. Education and training continue on an ongoing basis„when new residents enter the hospital each year, they are now being educated on processes for reducing the risks of surgical site infections.
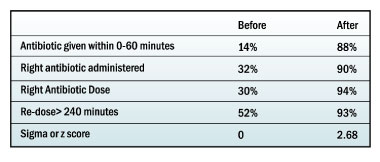
Controlling Results
As a result of interventions and changes in standard operating procedures, data revealed significant improvement in patients receiving the right dose of antibiotics at the right time. While progress and monitoring continue, the process has improved 91% from zero sigma to 2.86, and in addition to improving patient safety, the business case demonstrated annual savings in excess of $1 million.
To sustain the improvements, the team instituted the following measures:
- Prophylactic antibiotics were added to the pre-induction and pre-incision time-out.
- Pre-operative and intra-operative indicators will continue to be monitored by the Surgical Quality Improvement Council. Individual results are sent to surgeons, anesthesiologists, and CRNAs.
- A Six Sigma team is working on the discontinuation of antibiotics within 24 hours.
- The glucose indicators monitor patients with diagnosed and undiagnosed diabetes and will need further work.
- A project binder documenting the entire project was prepared for the administrators and physician champion.
- The results and project process are shared with the Peripheral Vascular Services Collaborative Practice and Surgical Quality Improvement Council.
Summary and Next Steps
In addition to providing obvious benefits for the patient, reducing surgical site infections offers a number of advantages for the hospital as well in conserving valuable resources„money, supplies, time, and labor„that can be applied in other care areas. Without the added length of stay, the hospital can free up capacity and improve bed availability for other patients.
 |
|
| Fig. 6 |
When CMS began monitoring the SSI indicators, Charleston Area Medical Center was ahead of the game. They were already 1 year and 9 months into the project before auditing began, and having this process in place helped them to demonstrate measurable improvement. Responses from the staff have been overwhelmingly positive, since the changes helped to make their jobs easier, rather than adding extra steps or work to the process.
The project to reduce the risks of surgical site infections is just one of many projects successfully completed at Charleston Area Medical Center since the leadership team launched a Six Sigma-based performance improvement initiative several years ago. With this project in the Control phase, the team’s next target will be improving postoperative glucose control and hypothermia.
Bibliography and Resources
Debbie Young is a registered nurse in the perioperative department at Charleston Area Medical Center in West Virginia. She is a certified Green Belt and spends approximately 50 to 60% of her time on Six Sigma projects designed to improve efficiency, quality, and cost management. She may be contacted at debbie.young@camc.org.
