Self-service Registration: Leading the Way to Safer, More Effective Care
November / December 2005
Self-service Registration
Leading the Way to Safer, More Effective Care
When it comes to improving the quality and safety of healthcare, few organizations classify the patient registration process as a top priority. But with the introduction of patient self-service technology that automates the check-in process, the flaws of traditional paper-based methods are becoming increasingly clear, including patient misidentification and the errors resulting from the duplicate manual entry of patient data.
By using self-service technology to streamline and improve the patient check-in process, healthcare organizations can eliminate these inherent challenges and improve the delivery of patient care. From electronically capturing consent documents to gathering vital medical history information, self-service technology facilitates a more effective registration process that ensures accurate patient identification and minimizes the potential for errors throughout the continuum of care.
The key to a successful self-service strategy lies in the integration with existing IT infrastructures — such as practice management systems, clinical data repositories and electronic medical records systems — so healthcare organizations can expand this strategy throughout the enterprise to achieve true clinical excellence. Whether identifying patients at check-in or improving provider access to patient information, a successful self-service technology will ultimately impact every step of the care process.
Authenticating Patient Identity at Check-In
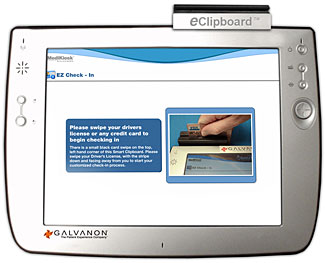
An automated patient registration process ensures more accurate patient identification at check-in by using the swipe of a driver’s license, credit card, or membership card to authenticate the patient’s identity (Figure 1). A second personal identifier, such as a birth date, is entered by the patient into the self-service device, providing the second level of authentication that HIPAA requires and helping to minimize the risks associated with patient misidentification.
| Figure 1. Patients swipe a driver’s license, credit card, or membership card to authenticate their identity. |
 |
|
| Courtesy of Galvanon |
When combined with biometric solutions, such as fingerprint imaging or smart card technology, self-service technologies further improve an organization’s ability to verify a patient’s identity, even those who may be unconscious or impaired. At Santa Barbara Cottage Hospital, patients have the option of providing a thumbprint or swiping a driver’s license to begin the registration process. Using biometric imaging not only enables the hospital to instantly identify patients but it also makes it easier for staff members to locate patients within the organization’s database, helping to reduce the likelihood of duplicate patient records.
Once patients are identified, they can begin checking in for the scheduled office visit, lab test, or hospital stay, where they will be asked to enter or verify demographic, insurance, and medical history information. This automated approach to patient check-in not only helps to ensure more accurate patient identification, but it also dramatically improves the overall quality of an organization’s access services. These services form the foundation for high-quality healthcare and ultimately determine if the appropriate patient information is gathered, how accurate the information is, and how quickly it is available to providers.
Preventing Data Entry Errors
All of the information captured during the automated patient check-in process, including medical history data, is automatically stored in an organization’s clinical data repository or electronic medical records (EMR) system, eliminating the need for staff to manually re-enter data and reducing the risk of clerical errors. This capability also gives providers quick and easy access to the information they need to effectively treat patients. For example, when patients are routinely asked to update their allergies and medications at each visit, their providers know which treatments or medications to avoid, such as those that may result in dangerous drug interactions.
Without the need to manually enter data from patient forms into the organization’s information systems, overall efficiency also increases, giving staff members more time to devote to patient-related questions and concerns. This enhances an organization’s ability to properly educate patients about conditions, medications, treatments, and surgeries — helping to make patients more active participants in their own care.
Many healthcare organizations also use self-service technology to ensure that the proper consent forms have been signed and that patient communications conform to HIPAA guidelines. Once signed, these forms can be passed along to an EMR or other electronic imaging and storage system, helping to reduce liability and the costs associated with managing a paper-based consent process.
Together, these self-service capabilities not only improve the way patients are registered and admitted, but they also enhance service to patients, boost satisfaction levels, and minimize wait times. As a result, patients can register for appointments quickly and easily, without the hassle of filling out redundant patient registration forms at each visit.
Vital Information at the Point of Care
Self-service technology can also be used to facilitate adaptive clinical screenings that have the ability to generate additional questions based on previous responses. This functionality provides many benefits over traditional pencil and paper screening methods, including enhanced patient privacy, increased accuracy, and reduced administrative costs. All of the data gathered during these screenings is then used to improve the delivery of preventive care services and support a more effective triage and treatment process.
At Ohio’s Columbus Children’s Hospital, eight pediatric-based primary care clinics have implemented self-service technology to automate a self-report adolescent screening program for at-risk behavior. Upon arrival at the facility, patients use the touch screen interface on the self-service device to complete a health risk assessment questionnaire concerning their use of alcohol and drugs, symptoms, and impairments for co-morbid mental disorders and other at-risk behaviors such as suicide ideation and depression.
Within seconds of survey completion, the self-reported results are summarized, scored using pre-defined algorithms, stored in the patient’s lab result, and made available to physicians during the same-day office visit. Having access to this personalized assessment information allows physicians to provide tailored advice and conduct interventions that are more likely to change patient behavior.
This automated approach also enables staff at Columbus Children’s Hospital to coordinate further research and follow-up activities, such as continued telephone support services that are consistent with the treatment regimen. As a result, providers have the tools they need to strengthen relationships with patients and establish an ongoing dialogue that promotes compliance with the prescribed plan of care.
Weighing the Options
Today’s self-service registration technologies are available in a variety of forms, including wireless tablet PCs, desktop kiosks, and freestanding kiosks. This range of hardware options gives healthcare organizations the flexibility they need to deploy self-service technology in a way that complements existing workflow, promotes efficiency, and enhances quality of care. For example, tablet PCs were the ideal choice for Columbus Children’s Hospital because its administration wanted to create a private screening process that patients could complete from their seats in the waiting area.
Once a hardware selection is made, the next step is to focus on the software, particularly on how it will dictate the patient’s experience with the technology. This step is especially important because providers will not be able to reap the safety and quality benefits of self-service technology unless they first drive user acceptance. That’s why it is crucial to carefully plan and evaluate all of the ways patients will interact with the technology to ensure the end result is both intuitive and easy-to-use.
Lastly, healthcare organizations should examine their existing IT infrastructure to determine how to best leverage self-service technology in combination with the current technology framework. A successful self-service strategy will include an interface with the facility’s administrative and clinical systems, including scheduling, ADT, and electronic medical records systems, to effectively eliminate duplicate data entry and simplify the management of patient information.
Looking Toward the Future
As the healthcare industry continues to look for new and innovative ways to reduce costs and improve quality, patient self-service technology presents a viable option for minimizing errors and increasing access to patient information at the point of care. From patient registration and triage to treatment and beyond, the use of self-service technology allows healthcare organizations to improve safety and quality at every step within the care process, resulting in a safer, more efficient healthcare system for patients and staff alike.
Raj Toleti (rtoleti@galvanon.com) is co-founder and CEO of Galvanon, a provider of kiosks, Web self-service applications, and technology that automates the patient registration process, streamlines everyday patient interactions, and improves patient flow through the healthcare process. Previously, Toleti was a founding member of the Microsoft Consulting Services (Healthcare) practice, where he was awarded the Excellence Award for Consulting from Microsoft.
