Second Victim Support: Implications for Patient Safety Attitudes and Perceptions
By Susan D. Scott, PhD, RN, CPPS
Although recent publications have enhanced our understanding of the second victim phenomenon, many questions remain unanswered. In an effort to explain this possible career-ending circumstance, the vast majority of the literature focuses on describing the second victim experience. An area that needs further investigation is the influence that second victim support might have on the overall patient safety culture in the context of the clinical work environment. This gap in knowledge provides an opportunity to discover the impact of clinician support on long-term patient safety perceptions and attitudes.
This study was designed to explore the impact of second victimization and provision of a formal clinician support infrastructure at a Midwestern academic healthcare system. The study was framed around the research question, “Over time, is there a difference in clinician perceptions relating to patient safety among three groups of survey respondents (non-victims, second victims with support, and second victims without support)?” The study represents a first quantitative link between second victim support and its influence on the overall culture of patient safety at both the departmental/unit and organizational levels.
Background
The Institute of Medicine’s (IOM) seminal report, To Err Is Human: Building a Safer Health System, advocated for healthcare organizations to develop a culture of patient care that focused on improving the safety of that care (Kohn, Corrigan, & Donaldson, 2000). Since the release of that report, significant efforts have been made to influence the safety culture within hospitals; however, much work is still needed (Wachter, 2012). In 2007, The Joint Commission required accredited hospitals to conduct staff surveys specific to patient safety to assess and advance organizational patient safety cultures (Pronovost & Sexton, 2005).
Patient safety culture surveys, administered on a regular basis, track changes in patient safety perceptions and evaluate the impact of various interventions. The self-report surveys were designed to obtain perceptions of the working environment from all staff, from frontline to administrative personnel (Colla, Bracken, Kinney, & Weeks, 2005). Assessment of the safety culture at departmental and facility levels helps organizational leaders identify areas that are in need of improvement in general patient safety concepts (Singla, Kitch, Weissman, & Campbell, 2006).
To address increasing regulatory and consumer expectations for enhancing patient safety considerations, a team was selected to oversee transformation of the University of Missouri Health Care (MUHC) patient safety culture. The team’s work included the development and implementation of an electronic adverse event reporting system, coordination of safety event investigations, and management of root cause analyses for the healthcare system (Kivlahan et al., 2002). As the event investigation process matured, this team identified that clinicians were frequently experiencing significant personal and professional emotional distress in the aftermath of unanticipated patient safety events (Scott, Hirschinger, & Cox, 2008). The team soon recognized that they were observing effects of the second victim phenomenon (Wu, 2000).
As MUHC patient safety researchers prepared to conduct an initial baseline assessment of the patient safety culture, they recognized a golden opportunity to identify second victim incidence within the organization. To quantify the prevalence of the second victim experience, a question was created using the second victim definition and added to the Agency for Healthcare Research and Quality Hospital Survey on Patient Safety (AHRQ-HSOPS) instrument.
The 2007 baseline assessment revealed that approximately one of every seven MUHC staff members reported having experienced a patient safety event that caused personal duress within the past year. Approximately one-third of the individuals received institutional support to assist with their emotional recovery (Scott et al., 2009). These findings led to a research trajectory designed to increase understanding of the second victim experience and to design supportive tactics for clinicians suffering as second victims (Scott et al., 2010; Scott et al., 2009; Scott, Hirschinger, & Cox, 2008).
The second victim experience
The second victim phenomenon is potentially a dangerous consequence for any individual working in a healthcare provider’s role. Historically, a vast majority of the healthcare workforce has suffered from career-related stress and anxiety as a result of unanticipated adverse clinical events (Wolf, Serembus, Smetzer, Cohen, & Cohen, 2000). The second victim phenomenon is fairly common; estimates project approximately half of all healthcare providers will experience its impact at least once during their professional career (Seys et al., 2013).
If not addressed, second victims can face long-term career sequelae such as changing roles or leaving the chosen profession prematurely. Most healthcare professionals are unsure where to turn for support and guidance (DeWit, Marks, Natterman, & Wu, 2013). Some fear that seeking emotional support is a stigma representing personal or professional weakness (Dekker, 2013). As a result, many suffer in silence. It is becoming evident that formalized tactics to address the suffering of second victims should be prioritized at every healthcare facility (Carr, 2009). Healthcare institutions should proactively anticipate needs of second victims and design interventions to sustain a healthy recovery (White, Waterman, McCotter, Boyle, & Gallagher, 2008).
Provision of emotional support for healthcare clinicians who may be suffering as second victims is critical for their psychosocial recovery after an unanticipated clinical event (Dekker, 2013). A few models of emotional support that allow healthcare organizations to meet the unique needs of healthcare providers after adverse clinical events have emerged in recent years (Seys et al., 2012; Conway et al., 2011; Scott et al., 2010). Important elements of these interventional models include an educational program to ensure providers are proactively aware of post-event practices, policies, or guidelines to govern the handling of adverse clinical events, and the existence as well as the expectation of a support system for individuals and teams of clinicians (Hall & Scott, 2012).
Intervention: MUHC’s forYOU Team
After several years of studying the second victim phenomenon, MUHC deployed a second victim emotional support infrastructure in 2009. This infrastructure, known as the forYOU Team, is a first-of-its-kind evidence-based second victim intervention that offers immediate emotional and social support (Scott et al., 2011). Introduction of the
forYOU Team to provide clinician support following an unanticipated clinical event was one of several interventional strategies chosen to enhance MUHC’s culture of patient safety. The forYOU Team was specifically designed to address the diverse needs of clinicians suffering as second victims (Scott et al., 2010). The team’s guiding principle is the understanding that each clinical event represents a unique experience, with each clinician requiring an individualized type and intensity of emotional support to facilitate second victim recovery.
The forYOU Team model allows for interventional support, from basic emotional first aid at the unit/department level to comprehensive, professional counseling services based on the individual needs of each clinician. Members of the forYOU Team provide emotional support using a three-tiered interventional methodology (Scott et al., 2010); each tier uses increasing institutional resources to help ensure that the emotional needs of the clinician are met. While some clinicians may only need the resources available from one tier of support, others might need resources from all three tiers to help promote professional and personal recovery (Hirschinger et al., 2015).
Research method
The purpose of this study was to investigate the impact of the second victim experience on patient safety attitudes and perceptions using the AHRQ-HSOPS survey instrument during four survey periods over approximately six years. Upon approval from the University of Missouri-Columbia Health Sciences Institutional Review Board, a cross-sectional analysis of existing MUHC Patient Safety Culture Survey findings was conducted. This study was designed to monitor for group differences among three clinician types (non-victims, second victims with support, and second victims without support). Three MUHC healthcare facilities (University Hospital, Women’s and Children’s Hospital, and Missouri Rehabilitation Center) participated in each of the four surveys. The study sample included MUHC clinicians who voluntarily completed the AHRQ-HSOPS survey and identified that they worked in one of the three MUHC facilities.
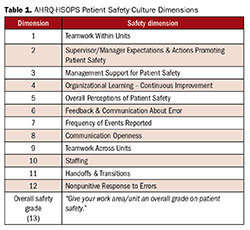
The AHRQ-HSOPS instrument—one of the most popular tools for assessing patient safety culture within a healthcare setting (Wachter, 2012)—was used to collect MUHC data over time. The tool assesses healthcare clinician opinions, attitudes, and perceptions about patient safety issues, medical error event reporting, and institutional responses to adverse events (AHRQ, 2013). It has been deemed psychometrically sound in evaluating the various identified dimensions within the context of patient safety and has been used in large populations of frontline healthcare providers (Sorra & Dyer, 2010). The tool has 44 questions and uses a five-point Likert scale. The survey requests clinicians to rate the safety culture within their respective units, as well as the overall organization. The survey contains an outcome variable, not included in any of the dimensions, that asks respondents to provide an overall safety grade for their local department or work unit. Table 1 provides a listing of the 12 specific dimensions and the overall safety grade question.
To assess prevalence of the second victim phenomenon at MUHC, two questions were added to MUHC’s AHRQ-HSOPS survey instrument. The primary question was, “In the last 12 months, were there any patient safety events that caused you personal problems such as anxiety, depression or concerns about your ability to do your job?” If the clinician responded “yes” to this question, then a subsequent question was asked: “Did you receive support from anyone within the MUHC system?” These questions were used to monitor MUHC second victim prevalence and associated perceptions of clinician support over time, and both have been incorporated as standard survey items for every MUHC culture survey.
The AHRQ-HSOPS survey has been administered to MUHC healthcare clinicians four times (prior to implementation of MUHC forYOU Team intervention, five months post-forYOU team deployment, three years post-forYOU Team deployment, and four years post-forYOU Team deployment). Surveys were administered in 2007, 2009, 2012, and 2013.
MUHC Patient Safety Culture Survey results were analyzed to assess influence of the second victim experience (with support and without support) on clinicians’ overall perceptions of patient safety. The dependent or outcomes variables included the 12 specific safety dimensions and the overall patient safety grade. Independent variables for this study were the three clinician groups (non-victims, second victim with support, and second victim without support).
Baseline patient safety culture data prior to implementation of the forYOU Team, five months after team deployment, and at two additional post-deployment assessment points were evaluated to determine if there were differences in the individual 12 patient safety dimensions or the overall patient safety grade across the three clinician groups.
The MUHC Patient Safety Culture Survey results for the four respective years were reviewed. Sample size was 1,054, 1,203, 758, and 1,213 respectively. A total of 4,228 participants were included in this study. MUHC’s AHRQ-HSPOS data were stratified by year, facility, professional type, and second victim exposure (non-victims, second victims with support, and second victims without support). Descriptive statistics using simple count and proportions were used to characterize the data elements. Mean group scores for each of the 12 safety dimensions and overall safety grade were calculated for each of the three second victim groups. A chi-square analysis was performed to determine rates that were compared across facilities and across time. Comparisons between groups were performed using logistic regression. For dimension scores, groups were compared using analysis of variance.
Since the research questions involved 13 variables (12 survey dimensions and the overall safety grade), a large number of statistical tests was required. Given the relatively large amount of data, it was possible to detect relatively small but statistically significant differences between groups. Because of this consideration, the threshold of p < .001 was established. To assist in determining the practical or clinical relevance or meaningfulness of this large data set, a mean score difference of > 0.40 was established a priori. A University of Missouri-Columbia biostatistician performed data analysis.
Results
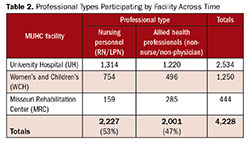
A total of 4,228 clinicians participated in the four surveys within the three hospital settings. Clinicians participating in the study were divided into two professional types: nursing personnel (registered nurses and licensed practical nurses) and allied health professionals (respiratory therapists, pharmacists, paramedics, etc.). Nursing personnel accounted for 2,227 (53%) of the total respondents, with allied health professionals making up 2,001 (47%). A breakdown of professional type by facility is included in Table 2. Across time, approximately one-fourth of the respondents (n = 1,040) self-identified as second victims by answering favorably to MUHC’s second victim primary screening question.
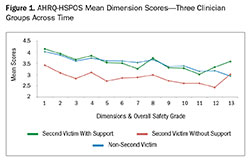
Analysis of the 12 patient safety dimensions and overall safety grade across time for the three clinician groups was conducted (Table 3). For individual dimensions, the supported second victim (SV+) mean scores are quite similar to non-victims; however, a striking difference is observed between supported second victim (SV+) and non-supported second victim (SV-) mean scores. In all 13 dimensions, the unsupported second victim (SV-) scores were lower than the supported victim (SV+) scores. Twelve of the 13 dimensions revealed highly statistically significant (p < .0001) differences between the second victims with support (SV+) and second victims without support (SV-). Clinical or practical meaningfulness was also attained in the same 12 dimensions. The mean score for MUHC second victims with support (SV+) was also noted to be higher than the AHRQ national benchmark mean in all 12 dimensions, with lower scores attained for the overall safety grade. When comparing the MUHC second victims without support (SV-) mean scores to the AHRQ national benchmark, MUHC scores were lower than the national mean in 10 of the 12 dimensions as well as the overall patient safety score.
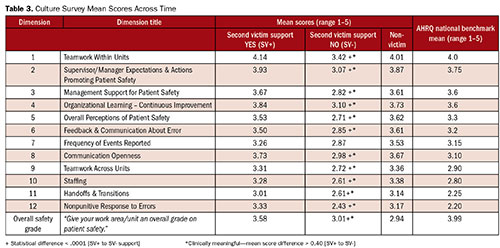
Supported second victims respond in meaningfully different ways from non-supported second victims. The information is readily obvious as captured in Figure 1, depicting responses from the three facilities across time. The x-axis represents the 12 safety dimensions plus the overall patient safety grade (#13). The y-axis represents mean score values. The relatively similar responses among the second victims with support and the non-victims in this depiction are apparent. However, there is a prominent difference in the mean scores among the non-supported second victims (red line).
Individuals identified as second victims without support were statistically different than their counterparts in the other two groups. This group had much lower overall mean scores than the national average in 10 of the 13 dimension scores. These lower scores contribute negatively to the overall patient safety environment. Individual department/units with high levels of support scored much higher on overall patient safety scores. As a result, for those clinical areas striving to increase their patient safety scores, proactively developing a second victim support strategy would be a wise investment.
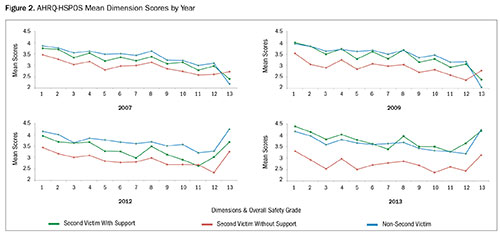
Data was also analyzed by year. The two baseline years (2007 and 2009) were relatively similar. As time progressed, and the forYOU Team efforts matured with increased awareness of second victims and increasing peer support presence, the differences in the unsupported second victim group (red line) became increasingly obvious (Figure 2).
Discussion
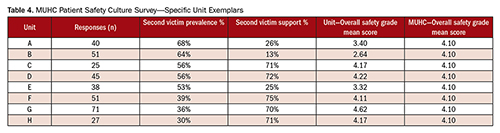
This longitudinal study highlights the importance of clinician support as well as the impact that this support affords future patient safety perceptions and attitudes. It also showcases the impact that unsupported clinicians have on their respective unit safety culture perceptions as well as facilitywide. To demonstrate the impact that support (or lack thereof) can have on individual unit safety scores, a table representing eight MUHC participating units was developed (Table 4). This table reflects the influence of second victim prevalence and perceived levels of support on the unit’s overall patient safety grade. It appears that supported second victims help raise the overall patient safety grade within units and facilities that have higher levels of perceived support. Conversely, unsupported second victims can significantly lower the overall patient safety scores.
Conclusion
This study reports on findings from an analysis of second victimization and perceived social support in three different hospitals in an academic health setting over a period of approximately six years. The knowledge gained from this research exemplifies the importance of second victim support within the context of the healthcare work environment.
The impact of MUHC’s interventional strategy to support second victims is captured in this longitudinal study. Patient safety researchers have come to appreciate the fact that the second victim phenomenon is potentially a serious consequence for every role within a healthcare setting. However, this study reveals that the impact of the second victim experience and the provision of support (or lack thereof) to individual clinicians may extend beyond the clinicians themselves, penetrating the working environment at both the unit and overall facility levels.
The study underscores the importance of clinician support in the aftermath of unanticipated clinical events. An organizational understanding and awareness of the second victim phenomenon, together with peer and supervisory surveillance in the aftermath of high-risk clinical events, provides a unique opportunity to enable second victims to receive the emotional support that many desperately desire. These findings introduce the argument that healthcare organizations now have an obligation to ensure emotional support strategies are designed to mitigate second victim suffering and optimize the existing patient safety culture. Clinician support interventions should be designed to address second victim responses of varying severities, ranging from simple peer interactions to prolonged professional support in more severe clinical safety events that involve a protracted litigation process.
Susan D. Scott is manager of patient safety/risk management at at University of Missouri Health System in Columbia, Missouri. Her research includes understanding the second victim phenomenon in an attempt to develop effective institutional supportive interventions. She is coordinator of MUHC’s forYOU team and may be contacted at scotts@health.missouri.edu.
References:
AHRQ survey on patient safety culture. (2013). Retrieved from http://www.mocps.org/culturesurvey/.
Carr, S. (2009). Disclosure and apology: What’s missing? Advancing programs that support clinicians (Issue Brief). Boston, MA: Medically Induced Trauma Support Services.
Conway, J., Federico, F., Stewart, K., & Campbell, M. (2011, March 1). Respectful management of serious clinical adverse events (White Paper—IHI Innovation Series). Retrieved from Institute for Healthcare Improvement: www.ihi.org/IHI/WhitePapers/.
DeWit, M. E., Marks, C. M., Natterman, J. P., & Wu, A. W. (2013). Supporting second victims of patient safety events: Shouldn’t these communications be covered by legal privilege? Journal of Law, Medicine, & Ethics, 852-858.
Dekker, S. (2013). Second victim: Error, guilt, trauma and resilience. Boca Raton, FL: CRC Press.
Hall, L. W., & Scott, S. D. (2012). The second victim of adverse health care events. Nursing Clinics of North America, 47(3), 383-393. doi:10.1016/j.cnur.2012.05.008.
Hirschinger, L. E., Scott, S. D., & Hahn-Cover, K. (2015). Clinician support: Five years of lessons learned. Patient Safety & Quality Healthcare, 12(2), 26-31.
Kivlahan, C., Sangster, W., Nelson, K., Buddenbaum, J., & Lobenstein, K. (2002). Developing a comprehensive electronic adverse event reporting system in an academic health center. Journal on Quality Improvement, 28(11), 583-594.
Kohn, L. T., Corrigan, J. M., & Donaldson, M. S. (Eds.). (2000). To err is human: Building a safer health system. Washington, DC: National Academies Press.
Pronovost, P., & Sexton, B. (2005). Assessing safety culture: Guidelines and recommendations. Quality and Safety in Health Care, 14, 231-233. doi:10.1136/qshc.2005.015180.
Scott, S. D., Hirschinger, L. E., & Cox, K. R. (2008). Sharing the load: Rescuing the healer after trauma. RN, 71, 38-43.
Scott, S. D., Hirschinger, L. E., Cox, K. R., McCoig, M. M., Brandt, J., & Hall, L. W. (2009). The natural history of recovery for the healthcare provider second victim after adverse patient events. Journal of Quality and Safety in Health Care, 18, 325-330.
Scott, S. D., Hirschinger, L. E., Cox, K. R., McCoig, M. M., Hahn-Cover, K., Epperly, K. M., … Hall, L. W. (2010). Caring for our own: Deploying a systemwide second victim rapid response team. The Joint Commission Journal on Quality and Patient Safety, 36(5), 233-240.
Scott, S. D., Hirschinger, L. E., McCoig, M. M., Cox, K. R., Hahn-Cover, K., & Hall, L. W. (2011). The second victim. In M. A. DeVita, K. Hillman, & R. Bellomo (Eds.), Textbook of rapid response systems (pp. 321-330). New York, NY: Springer.
Seys, D., Scott, S., Wu, A., Van Gerven, E., Vleugels, A., Euwema, M., … Vanhaecht, K. (2012). Supporting involved health care professionals (second victims) following an adverse health event: A literature review. International Journal of Nursing Studies. doi:10.1016/j.ijnurstu.2012.07.006.
Seys, D., Wu, A. W., Van Gerven, E., Vleugels, A., Euwema, M., Panella, M., … Vanhaecht, K. (2013). Health care professionals as second victims after adverse events: A systematic review. Evaluation & The Health Professions, 36(2), 133-160. doi:10.1177/0163278712458918.
Singla, A. K., Kitch, B. T., Weissman, J. S., & Campbell, E. G. (2006). Assessing patient safety culture: A review and synthesis of the measurement tools. Journal of Patient Safety, 2(3), 105-115.
Sorra, J. S., & Dyer, N. (2010). Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Services Research, 10. Retrieved from http://www.biomedcentral.com/1472-6963/10/199.
Wachter, R. M. (2012). Understanding patient safety (2nd ed.). New York, NY: McGraw Hill Medical.
White, A. A., Waterman, A., McCotter, P., Boyle, D., & Gallagher, T. H. (2008). Supporting health care workers after medical error: Considerations for healthcare leaders. Journal of Clinical Outcomes Management, 15, 240-247.
Wolf, Z. R., Serembus, J. F., Smetzer, J., Cohen, H., & Cohen, M. (2000). Responses and concerns of healthcare providers to medication errors. Clinical Nurse Specialist, 14, 278-287.
Wu, A. (2000). Medical error: The second victim. The doctor who makes the mistake needs help too. British Medical Journal, 320, 726-727.
