Quality Reporting Through a Data Warehouse
January / February 2009
![]()
Population Decision Support
Quality Reporting Through a Data Warehouse
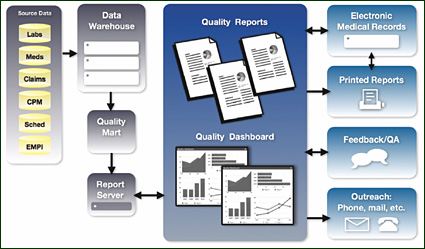
Developing a clinical data warehouse is a key first step toward improving quality reporting functionality, which supports the entire care enterprise. While patient data resides in numerous disparate locations, it is only when the information is brought together for analysis that a more complete picture of the population — and its individual members — can begin to emerge.
Quality reporting made possible by data warehousing provides benefits across the enterprise, enabling initiatives such as: proactive treatment programs that result in improved compliance with evidence-based guidelines; chronic disease monitoring that improves patient satisfaction and outcomes; and the development of population decision support systems, which provide greater visibility into performance at the organizational and population levels and enable daily workflow tools that ease the burden of managing large patient populations.
Proactive Treatment Programs
Much like an auto dealership sends out reminder postcards to its clientele for regular maintenance activities based on a pre-determined schedule, healthcare providers can deliver health maintenance reminders to their patients, based on evidence-based guidelines. The logic to support such a proactive healthcare program is far more sophisticated than the auto maintenance example, but the data is available to harvest within clinical applications and billing systems, and the goals are the same: to improve outcomes and reduce costs through preventative treatment.
A proactive outreach program increases patient participation, satisfaction, and outcomes by reminding patients (or their caregivers) of upcoming or overdue tests, immunizations, or follow-up visits. For those hospitals and networks without EHR decision support systems, system ticklers, or other outreach mechanisms that remind physicians about needed services, a data warehousing and quality reporting system increases the rate of patients receiving care based on evidence based measures — and, thus, quality of care.
Looking at an example like childhood immunizations, the complexity of providing proactive care starts to become apparent. Pediatric practices face unique preventative care challenges based on the specific needs of their young populations, including managing immunization schedules and scheduling of well child visits for thousands of patients. While EHR decision support systems — where available — can alert the doctor of needed immunizations during an office visit, such a reminder serves no purpose if the parent does not first make a visit.
A data warehouse and complementary reporting system can simplify the management of immunization schedules, with status reports highlighting patients who need to be scheduled for visits printed by or automatically sent to clinicians and their support staff. While this may seem simple enough to accomplish, the process is convoluted by the need to access and join together data from multiple data sources, including patient contact and demographic information, vaccination history, and a scheduling system, while accurately mapping providers to patients and providers to clinics to understand performance and accountability. Additionally, the logic contained in the warehouse must be intelligent enough to translate up-to-date CDC guidelines to properly identify which immunizations are recommended for each patient and to factor changing combination vaccinations such as Pediarix®. All of these factors can be supported through a data warehouse solution that includes the data, the logic, and the reporting utilities to support clinical workflows to improve quality, without the tedious manual effort currently required to accomplish this task.
![]()
Chronic Disease Monitoring
When facing a more complex challenge like managing and reporting on chronic disease panels, the need for sophisticated quality reporting is more evident and more likely to impact both long term costs and patient outcomes. For the purposes of illustration, this article primarily focuses on diabetes, but the challenges discussed are typical for other chronic diseases, as well, such as coronary artery disease, congestive heart failure, and asthma.
For many providers diabetes has been one of the first areas where data management efforts have been applied to improve quality of care in chronic diseases. This is because the diabetic population is among the largest and fastest growing and also faces high risk with many preventable long term, high cost complications. Also, it is possible to both identify the patients at risk and take actions to reduce it. Key indicators have been established for providing high performance diabetes care based on a strong outcomes based measure, HbA1c levels, as well as a number of process measures like periodic lab testing for HbA1c, micro-albumin, LDL, foot and eye exams. Because many of the process areas are measurable in claims data, commercial payors and CMS offer P4P incentives through HEDIS measures to improve diabetes care.
As a result, diabetes represents not only a quality opportunity but also one tied directly to revenue. But for many provider organizations the lack of an effective data management and reporting infrastructure to track diabetic populations and establish initiatives to improve care is a significant challenge.
Without a data warehousing system, there is no way to generate accurate quality reports on a timely basis. Accurate and timely reporting is critical to proactively impact diabetic patients — who require an enhanced level of care — and achieve high performance on measures. In the absence of a proactive treatment program, care providers are typically only alerted to the gaps in their patients’ care during office visits. This leads to worsening performance as the passive patients who do not follow provider guidance — the patients measures generally track for quality — fall through the cracks.
Institutional and managerial visibility into performance related to diabetic panels is also hindered and, as a result, otherwise addressable issues like insufficient evidence of foot exams across a practice put P4P numbers — and associated income — at risk.
Logic built into the reporting system can analyze data from disparate sources and identify at-risk patients and populations before high-cost episodes occur. Management reports can also allow medical directors to compare physicians within their practice (e.g. tracking average HbA1c levels by provider) to identify and engage with the providers that are lagging behind their peers, as well as to recognize the top performers. And the availability of timely and accurate quality reports can help administrators identify operational issues across an enterprise to determine where additional resources may be needed.
Population-Based Decision Support Systems and Workflows
Data warehousing and quality reporting provide the elements needed to build population decision support systems that allow understanding of performance at all levels, as well as to enable tools that support daily or monthly workflows for care teams to better manage their busy patient calendars. These workflow tools are effective in alerting team members to patients who should be contacted to schedule key services and to ensure that needed testing is optimized during visits by orchestrating tests prior to the busy visit encounter.
At an operational and oversight level, decision support systems can identify quality of care issues based on evidence-based guidelines, which, if left uncorrected, can lead to diminished P4P numbers, exposure to lawsuits, and poor public perception of a facility or network. Quality reporting via a data warehouse arms administrators with the information they need to intervene with practices and providers, boosting quality metrics before a problem is exposed to a broader audience.
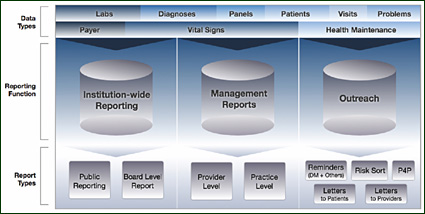
Quality Reporting Serves Multiple Viewpoints
Diabetes, like other chronic conditions, requires quality reporting from three different perspectives: institution-wide reporting, management reporting, and outreach opportunities.
Institution-wide Reporting
Institutional visibility into data is critical to monitoring how the hospital or network is performing. Such reporting is essential for identifying areas of weakness so that quality improvement is executed with top level management support and visibility into the impact of initiatives. Positive results avoid negative publicity for publicly reported measures, and improve financials by achieving favorable contracts with insurers.
Hospital administrators are also tasked with reporting to key stakeholders such as board members. Whereas these reports can be burdensome to compile, a quality data warehousing system eases the creation process and eliminates the need to cut and paste data from disparate spreadsheets.
Furthermore, administrators can gain insights into which departments or focus areas of the hospital or network may require additional resources.
Management Reporting
At the managerial level, medical directors can identify gaps in care and work with practices and providers to make specific improvements local to their groups. Physicians and practices can also be compared to each other to identify the stronger and weaker performers and initiate steps to share best practices and bring the less effective providers in line with their peers.
Outreach Opportunities
Outreach reporting provides the capabilities to directly impact care at an individual patient level and, therefore, entails direct interaction with many constituencies, including the patients themselves. It can also be the most complex to execute but also the most effective because it provides individual prioritized opportunities for improvement. For patients with diabetes, the patient and the care provider both can be alerted to areas of concern like missing or overdue exams and HbA1c levels that are not in control.
Outreach reporting can also support proactive efforts to prevent new health conditions. By identifying the highest risk diabetics through algorithms that look across the full set of diabetes evidence-based care guidelines, clinic administrators can prioritize their limited time by using risk ranking reports to identify and schedule visits with the patients within the population who will benefit most from the outreach.
Additional outreach reports focused on more statistical calculations of metrics used in P4P or PQRI (Physician’s Quality Reporting Incentive) allow providers to understand how they are performing against measures and how that matches with organizational goals and objectives. They can then work with their team to change practice workflows or campaigns to improve the performance before a measurement period is complete.
The new concepts being developed around the medical home will include a more comprehensive outlook on care that will drive a greater accountability between the clinic and the patient rather than a single provider and a patient. Quality reporting driven from data warehouses will be needed to support the medical home because tracking care and outreach across providers will require a more sophisticated view not possible without detailed data and rules to measure teams and their delivery of care to populations.
The effectiveness of each type of report — whether for institutional, managerial, or outreach purposes — is directly affected by the capabilities of the data warehousing and quality reporting system. A system that can not interpret evidence-based guidelines, for example, will produce insufficient or inaccurate reports, resulting in poor performance or — more troublesome — issues with patient safety.
![]()
Benefits of Data Warehousing and Quality Reporting
The benefits of establishing a quality data warehouse and reporting system are wide ranging, but the key improvements include:
Rapid and on-demand access to large sets of data across domains.
Instantaneous access to quality data offers value across an enterprise’s constituency: care management teams can easily run daily or weekly patient summaries that alert providers to needed actions for specific patients; and administrators can readily monitor providers’ and practices’ compliance with evidence-based guidelines for P4P analysis and overall quality improvement.
Establishing workflows to identify and fix quality issues in populations of patients.
Timely data, like notices about recalled medications or administering catch-up vaccinations due to temporary vaccine shortages, can be incorporated into one-time workflows to improve the safety of patient populations. Automating these processes significantly reduces the manual effort currently required to manage these situations.
Improvements in pay-for-reporting and pay-for-performance activities.
Hospitals and provider systems can achieve more success toward meeting pay-for-reporting and pay-for-performance goals, and can subsequently negotiate contracts with higher compensations based on their superior performance.
Identification of issues relating to disparities of care.
Tracking key measures for P4P purposes typically only applies to the members of large payors’ health plans. By focusing only on patients of commercial payor plans (generally higher income patients), disparities of care can result as less time is spent on patients who are not affiliated with a major insurer.
Data warehousing and reports at provider sites that focus on entire populations through EHR data allow potential disparities to be identified and improvements to be executed in a fair manner. This benefits the patient and organization alike, as high-cost episodes often provided as uncompensated or care delivered at reduced compensation rates can be avoided through the same proactive programs delivered to meet P4P objectives.
Reduced risk/liability; visibility into areas of risk.
Administrators can gain visibility into their organizations’ exposure to risk due to gaps in care. For example lab orders for colonoscopies that are incomplete may create a liability issue if the patient is later found to have colon cancer that would have been detected by the colonoscopy, had it occurred. By incorporating controls into the analysis of patient data, organizations can help their member providers and practices improve their patients’ outcomes, while reducing the hospital’s liability exposure.

![]()
Challenges
While the benefits of building a quality data warehouse and reporting system are many, doing so is a multi-faceted and complex proposition. Specific challenges involved with such an endeavor include:
Ensuring data privacy and security.
HIPAA violations, lawsuits, and negative public image are just a few of the consequences that can result from improperly protected patient data. Therefore, the data warehouse must incorporate role- and practice-level controls to prevent unauthorized access to patient information, as well as auditing and logging functionality for retrospective activity reporting. Effective data stewardship also must avoid issues at the outset (e.g., quality data being used for research purposes without IRB approval).
Creating relevance for providers.
There is plenty of potential for variability when measuring a specific aspect of a patient’s health, like hypertension, pain scores, or disease progression. A report or measure that rolls-up this information into summaries is a gauge and any gauge introduces additional variation due to the variation of the gauge itself. With the combination of the measure of the patient’s health and variation in how the population gets measured, it is easy to get to the point where noise and imperfections in the measurements lead to useless reporting. So it is critical (and difficult) to minimize the variability and imperfections in the way that measures are constructed and rolled-up.
Many providers and practices are skeptical when it comes to the accuracy of performance reports because of the difficulty of reliably matching patients and provider panels. A quality report that erroneously includes patient data from outside one’s practice undermines the provider’s confidence in the report and may lead to the provider ignoring useful information presented about their actual patients. Even if the provider reports the error, the new (subsequent) report’s findings will likely still be met with skepticism. To avoid this, a quality reporting team must focus a large effort in obtaining the necessary management support, data sets, and resources to get provider panels right.
Complexity in properly reporting against clinical data.
Clinical data is nuanced and, as such, can create challenges when reporting patient care and outcomes. For example, evidence-based guidelines for coronary artery disease (CAD) call for the use of beta blockers, but some CAD patients are allergic to those medications. The logic and available data built into the data warehousing and reporting system, consequently, must account for these detailed pieces of information so that providers and practices are not measured negatively for doing the right thing.
The system should also be able to accommodate updates to evidence-based guidelines in a timely manner so that the latest knowledge about specific conditions is considered. Without such flexibility, there is a risk of demonstrating non-compliance with evidence-based medicine.
Quality is a problem distributed among all members of the team.
Without an incentive, there is little motivation for practices to focus on improving outcomes across patient populations, especially given the day-to-day operational demands they face. Although there have been pilot programs that have proven successful in identifying and improving the health of specific at-risk populations, funding and resources to support such programs are limited and a quality reporting system is often seen as a cost that can be eliminated or limited. Often it takes an enlightened senior management team focused on quality over financial issues within the mission of the organization to allocate adequate resources to quality data warehousing and reporting.
Billing and clinical data sets are flawed and provide different views.
Quality reports are used by different constituencies for different purposes. Similarly, billing and clinical data sets offer different views of the same patient encounter. The data warehousing system must be able to capture and analyze these differing data elements and present the information to the end-user in an actionable format.
Billing and clinical data points each have inherent flaws, which lead to inconsistent or incomplete records: billing data is only useful for patients who are billed and not, for example, for indigent or traveling patients. It also doesn’t contain critical detailed information like the value of a test or measurement. Clinical data is often input hurriedly or primarily for the purpose of documenting the result of a visit, resulting in inaccurate and incomplete records, with the bulk of content stored in clinical notes rather than structured formats. This results in inconsistent records across populations. But imperfect data is not a good enough reason not to measure and improve quality.
Key Success Factors
A healthcare enterprise must consider several key factors to ensure success when implementing a quality data warehousing and reporting system, including:
Achieve adequate sponsorship and governance.
A bottoms-up approach to a data warehouse or a quality reporting application is unlikely to succeed in the long run. The breadth of issues that will ultimately need to be solved requires sponsorship from senior leaders like the CMIO, CEO, and quality committees to overcome roadblocks like data access, commitment to use quality reports for interventions, and improvement of data quality to make accurate measurements. This does not mean that projects must boil the ocean. Even a small quality reporting initiative focused on a specific area is worth executing as long as the technical initiatives are matched with overall commitments to making changes that result in quality improvements. Starting small to prove success with senior sponsorship in a particular area is often the best place to start.
Integrate reporting and proactive outreach tools with the clinical team’s workflow.
When integrated with the care staff’s regular activities, patient reports and reminders can be very effective in improving outcomes and patient satisfaction, as well as helping to prevent costly episodes. Given the demands of busy patient-centric calendars, however, a practice manager or medical assistant is less likely to access such information if it means breaking from the normal routine.
Present quality reports in the correct context.
Quality reports serve multiple purposes, depending on the needs of the end user. Therefore, the reporting system must be able to present data to many different constituencies in a format that is useful for each.
Align with financial incentives but avoid
disparities of care.
Pay-for-performance programs are effective in improving outcomes for targeted patients covered by major insurance plans, but other populations with similar conditions can suffer as a result. to ensure true success in improving patient outcomes, regardless of whether they are affiliated with a major payor, quality reports should consider all patients.
Conclusions
The proactive outreach, chronic disease monitoring, and population decision support that quality data warehousing makes possible benefit all key stakeholders and result in a more effective and efficient enterprise. Quality reporting and enhanced workflows allow clinicians to more actively monitor and provide proactive care to at-risk populations, while medical directors and other administrators can more accurately predict revenue streams and identify areas of concern before greater issues arise. While the development and implementation of a quality data warehousing and reporting system is a complex process that requires an investment of time and resources, the potential for improved quality of care, patient outcomes, and revenues make the effort worthwhile.
|
Dan Housman is a managing director at Recombinant Data Corp., a firm that provides data warehousing and clinical intelligence solutions to healthcare providers and academic medical centers. Housman has delivered web-based analytical applications for healthcare providers including quality dashboards, disease management reports, compensation incentive metrics, and analysis of publicly reported measures. He earned a bachelor of science degree in chemistry and biology from MIT in 1995 and is an active member of HDWA (Healthcare Data Warehousing Association) and AMIA (American Medical Informatics Association). Housman may be contacted at DHousman@recomdata.com.
