Quality Metric – Proceedings from the Quality Colloquium: Implementing Evidence-Based Guidelines and Reporting Results Through a Quality Metric
March / April 2005
Quality Metric
Proceedings from the Quality Colloquium: Implementing Evidence-Based Guidelines and Reporting Results Through a Quality Metric
![]()
Although it is generally acknowledged that evidence-based medicine (EBM) reflects expert consensus about the standard of care in specific disease processes, implementing guidelines that incorporate EBM meets with a great deal of resistance. Therefore, the challenge facing healthcare organizations is not in establishing the value of EBM, which has been widely recognized for years and by many experts, but in how to change habituated practice, physician reluctance, and an unsupportive hospital culture so that guidelines are more readily embraced. Data are compelling and persuasive to administrators and physicians, especially comparative data that target specific patient populations and that illustrate improved patient safety and successful outcomes.
Leadership’s acceptance of the value of EBM as a tool to improve operational performance and clinical outcome is crucial for success. The national safety movement specifically identified an organization’s leadership as critical to promoting changed practices. For EBM to become operationalized, the CEO has to promote support by establishing explicit policies and procedures. The Medical Board must also endorse and approve EBM as the community standard of care. Accreditation agencies set standards of care and recommend guideline use to ensure uniformity of practice across the continuum. However, because the medical staff is voluntary and thus not integrated into the hospital organization, encouraging compliance with guideline use requires appealing to their good will. To implement EBM at the bedside for the healthcare team, education and communication are central.
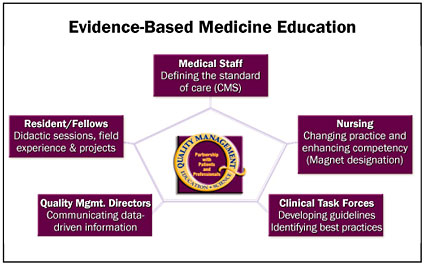
To develop techniques that will bridge the disconnect between actual practice and what are known to be best practices and highest-quality standards, the North Shore-LIJ Health System (NS-LIJHS)ãcomprised of 15 hospitals, including community, tertiary hospitals, and spanning diverse services, such as long-term care facilities, rehabilitation, and behavioral health facilitiesãhas promoted the development and use of guidelines. The CEO encourages education of our 32,000 employees through the Center for Learning and Innovation and through the new employee orientation program, known as Foundations. Quality is a key element of the teaching. As of today, 480 managers, 5,757 orientees, and approximately 2,000 nurses have received this education. A quality management rotation for nurses and fellows has been implemented as well (Figure 1).
![]()
The Quality Management Department encouraged the Plan Do Check Act (PCDA) methodology for performance improvement through prioritization, brainstorming, team meetings, evaluation, and implementation of clinical pathways. These activities helped to change the hospital culture by involving clinicians firsthand in the hospital organization and operation. Through multidisciplinary task forces, the healthcare team takes greater responsibility for supporting evidence-based practice guidelines and describes successful outcomes. Task forces optimize patient care; standardizing measurements for that care helps to identify gaps and best practices. Communication among disciplines is enhanced as is patient education. These efforts are reinforced to both the clinical and administrative staff through data that define changed processes.
Administrators need to be educated about how guideline use promotes efficiency of resource utilization as well, more than other approaches that have proved unproductive. The HMOs encouraged reducing length of stay (LOS) for increasing efficiency, but applying such a simplistic notion to such a complex phenomenon as illness wasn’t successful. Again, using data to focus attention on the relationship among quality of care, standardizing care with guidelines, cost, and efficient resource utilization helps administrators understand the value of incorporating EBM into practice.
The Centers for Medicare and Medicaid Services (CMS) formulated an approach to encourage compliance with EBM guidelines by offering financial incentives for those organizations that successfully meet their recommendations. By establishing safety guidelines, such as the importance of hand washing in reducing infection, the National Patient Safety Program acknowledges that the source of errors lies in the hospital culture and common practices. Again, clinicians express skepticism about the relevance of guidelines to their specific practices, suggesting that they don’t need to be told how to perform. However, the recent MRSA outbreak in England suggests that although the admonition regarding hand washing has been in place for decades, people are still dying because of non-compliance with this most elementary EBM of hygiene.
With the support of leadership, through system quality management, quality indicators and databases are consistently analyzed to meet the vision of delivering quality care to all patients, regardless of where they interact with the diverse system. Fundamental to this vision, implementing EBM is accomplished through promoting clinical pathways that integrate CMS measures, focusing on improving processes, and educating medical and nursing professionals on quality principles and the importance of data and measurements.
Most important, to change practice at the bedside, a formal methodology is required that increases collaboration and efficiency and strengthens accountability by linking assessment and intervention strategies with patient outcomes. The over 170 clinical pathways used in the NS-LIJHS provides this methodology, while data revealing variation from the treatment outlined in the clinical pathway provide information regarding compliance with the standard of care. For example, when variance analysis revealed that heart failure patients were discharged without adequate instructions and education for care, the identification of this problem enabled caregivers to improve their discharge instructions, especially regarding the importance of complying with medication administration. Clinical pathways also provide patients with accessible information so that they can be active participants in their own care. They are informed about their disease process, the treatment goals, the function of medication and tests, the importance of diet and activity, and particulars about their at-home care.
Variance analysis measures the distance between guidelines and actual practice. Data are collected and analyzed in order for caregivers to have information about compliance with specified interventions and to understand what impact interventions have on patient outcomes. CMS measures are collected and aggregated for system hospitals; data on compliance with these measures are reported out monthly to identify areas of improvement and best practices. Compliance with these measures increases accountability because this objective standard is available for public scrutiny.
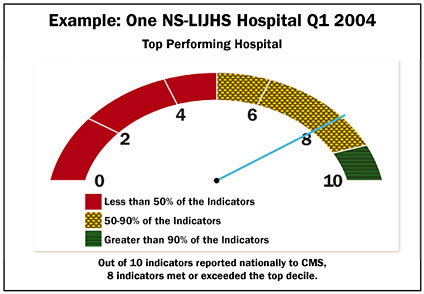
If physicians claim that the data aren’t relevant to their patients because their patients are special and their care is appropriate, then the data can provide a profile for them to evaluate how far they are, in their practice, from meeting the goal of the evidence. Further data show that their patients are, in fact, similar to others in the data set. Only their performance accounts for the difference. The intent of the data analysis is to promote compliance with the guidelines by the physician. For example, all patients presenting to an emergency department with a myocardial infarct who can benefit from the administration of aspirin and/or beta-blockers, should receive that care. A clear graphic representation using colors (red representing 50 percentile or less compliance, yellow 50-90 percentile, and green, the top decile, based on national performance) illustrates the rate of compliance. In order to move from the lowest level, the red zone, to the highest, the green, physician participation and leadership commitment are essential. (Through these measures, a benchmark is established; much as the finance departments develop a predictive projection of future expenditure, based on past performance, benchmarks of quality care also can be used to gauge performance Figure 2, page 42).
![]()
When EBM is standardized throughout the organization, clinicians and administrators see the benefits. For example, pneumonia patients on clinical pathways can be tracked for appropriate and timely interventions that result in appropriate and timely discharge. The clinical pathway alerts the caregiving team that Day 3 is the optimum time to switch the method of antibiotic delivery (from IV to PO), a switch that, when medically appropriate, triggers the implementation of the discharge plan. When clinicians and administrators track LOS they are able to monitor underuse and overuse of resources. Through these aggregated data, care is improved, utilization is monitored for improvement, and LOS is decreased. Patient care is seamless; interventions are implemented in a timely way; communication among the team is maximized because everyone knows what is expected, and whether those expectations were met. Arguments about the validity of EBM are overcome by monitoring patient outcomes post-discharge through tracking and trending such measures as readmission and infection rates.
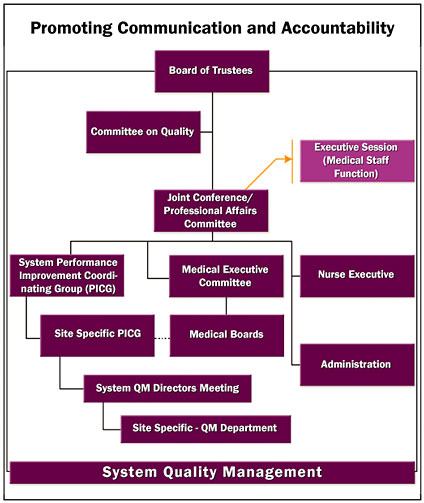
Improvements, guidelines, measures, and analyses all need to be shared vertically, from the bedside to the Board of Trustees, and horizontally across the many services and departments that oversee patient care. The quality management committee structure maintains communication and accountability through multidisciplinary committees that are organized to oversee different areas: acute, behavioral, rehabilitation, nursing home, home care, safety, and ambulatory (Figure 3). Databases for quality form the building blocks of a process that internalizes EMB into daily patient care.
![]()
Andrea Restifo, vice president of quality management for the North Shore-LIJ Health System, is responsible for the operations of the system quality management department, and serves as the corporate liaison to the JCAHO. She is responsible for communicating information related to regulatory preparation, best practices, lessons learned from incidents, and the establishment of system quality initiatives to the quality management staff throughout the system. Restifo is Dlugacz’s co-author on The Quality Handbook for Health Care Organizations: A Manager’s Guide to Tools and Programs.
Karen Nelson, RN, assistant vice president of quality management for the North Shore-LIJ Health System, oversees the utilization management program, continuum of care planning, and the JCAHO’s and Centers for Medicare and Medicaid Services core measures process. She serves as faculty for the Center for Learning and Innovation and has taught quality management to hospital executives at Beijing International MBA Program at Peking University, Beijing, China. Most recently, Nelson received the 2004 IPRO Excellence In Quality Improvement Award in recognition of championing clinical pathway and core measures implementation and motivating physician, nursing, and quality leaders to ensure consistent quality of care.
