Quality Initiative Focuses on Cellulitis and the Problem of Diagnostic Error
By Patricia Gogniat, MLS; Art Papier, MD; Sandra Schneider, MD, FACEP
Cellulitis is a common infection that affects the skin and subcutaneous tissues and results in significant morbidity and associated healthcare costs. In fact, more than $3.7 billion were spent on 240,000 inpatient admissions for cellulitis in the United States in 2004 (Solucient, 2006). In addition to these costs, more than 14.5 million individuals were treated in offices, hospital outpatient clinics, and emergency departments for skin infections in 2005 (Hersh, Chambers, Maselli, & Gonzales, 2008). Cellulitis is common in other countries; for example, more than 400,000 bed stays were reported per year in 2009–2010 in the English National Health Service, with an associated cost of £96 million (over $125 million) (Levell, Wingfield, & Garioch, 2011). Importantly, cellulitis as a primary diagnosis increased more than 25% annually from 1999 to 2005 in the United States (Klein, Smith, & Laxminarayan, 2007), indicating that skin and soft tissue infections are growing rapidly.
Cellulitis is a clinical diagnosis, as no currently available tests or imaging results specifically confirm or refute a diagnosis of cellulitis. While red skin and inflammation of the skin are signs of cellulitis, these symptoms are present in many other non-bacterial disease processes. The differential diagnosis of cellulitis is broad, ranging from common inflammatory skin processes such as stasis and contact dermatitis to rare life-threatening presentations such as necrotizing fasciitis (Hirschmann, 2012). There is a paucity of clinical aids for clinicians to differentiate cellulitis from other conditions. There are no accepted evidence-based clinical guidelines (David et al., 2011). The misdiagnosis of cellulitis (“false negatives”) can lead to worsening infection, serious complications, and potentially even sepsis. Incorrect diagnosis of this problem (“false positives”) can result in costly hospitalizations and overuse of intravenous antibiotics. Exposure to antibiotics puts these patients at risk for adverse drug reactions and contributes to antibiotic-resistant organisms (Roujeau et al., 1995; Hällgren, Tengvall-Linder, Persson, & Wahlgren, 2003). Furthermore, hospitalization subjects patients to iatrogenic disease, hospital-borne infections (such as Clostridium difficile), and adverse reactions to medications. Indeed, nosocomial infection with methicillin-resistant Staphylococcus aureus (MRSA) or C. difficile is a considerable problem for these admitted patients.
The United States Centers for Disease Control and Prevention (CDC) estimates that 1.7 million hospital-acquired infections occur each year in the United States, indicating that approximately 1 of every 20 inpatients will acquire such an infection (CDC; http://www.cdc.gov/hai/burden.html). Furthermore, nearly 100,000 deaths result directly from these infections each year (Klevens et al., 2007), and not surprisingly, the majority of these deaths are likely caused by infections with highly resistant bacteria. Awareness of this problem is prevalent, and the United States Department of Health and Human Services (HHS) has listed prevention and reduction of healthcare-associated infections as a top priority. For all of these reasons, it is important that patients who do not require hospitalization for treatment are treated as outpatients.
Recent studies have highlighted the magnitude of the problem around accurate diagnosis of cellulitis. In one study, diagnostic error occurred in 28% in patients hospitalized for cellulitis (David et al., 2011). In another study conducted in the United Kingdom, 33% of 635 cases of cellulitis were misdiagnosed (Levell et al., 2011). Even using a conservative 20% error rate, an estimated 114,000 of the 557,000 inpatient admissions for cellulitis in the United States each year may be preventable, with a potentially avoidable cost of $1,368,000,000 per year in the United States.
Many strategies have been tried to improve diagnostic accuracy and quality of care. These range from evidence-based guidelines to staff education and checklists. Peter Pronovost has demonstrated remarkable decreases in catheter-related bloodstream infections in the ICU through the implementation of five multifaceted interventions to ensure adherence with evidence-based infection control guidelines (Berenholtz et al., 2004). These simple and inexpensive interventions included education of staff, creation of a catheter insertion cart, daily inquisition of providers as to whether catheters could be removed, implementation of a checklist to ensure adherence, and empowerment of nurses to stop catheter insertion if a violation of the guidelines was observed. Using this method, central line infections were reduced 70% in the intervention group (Marsteller et al., 2012). Although no one variable has been shown to be responsible for the documented improvement in infection control, simple tactics including reliance on a checklist are likely to contribute to this success. Thus, we have developed a quality initiative that blends an online protocol with problem-oriented clinical decision support to improve diagnostic accuracy for cellulitis.
Quality Initiative to Improve Diagnostic Accuracy
We chose the diagnostic area of cellulitis as a focus for our efforts to reduce diagnostic error primarily because the diagnosis of cellulitis is essentially clinical, and cognitive errors in diagnosis and management are central to the problem area. We developed a multipronged strategy to improve the diagnosis of cellulitis in an effort to reduce diagnostic errors and ultimately to decrease hospital admissions, improve patient care, reduce medical costs associated with treatment, prevent unnecessary administration of antibiotics, and free up scarce hospital beds. This quality improvement (QI) initiative works in concert with the current community effort to reduce C. difficile infections in hospitals and with the recent New York State hospital requirements (New York State Department of Health, 2013) for the diagnosis and appropriate early treatment of sepsis. The expected outcome of this initiative is to reduce the number of false-positive cellulitis diagnoses that result in unnecessary hospital admissions.
As a first step, it was essential to develop collaboration among regional hospitals, including Rochester General, Strong Memorial, Highland Hospital, and Unity Health along with additional regional and rural hospitals in New York, Excellus Blue Cross Blue Shield, and Logical Images, the company that developed the visual diagnostic clinical decision support system to be used in the initiative. This collaboration initially took place at the leadership level (the project is funded jointly by the four regional hospitals and Excellus BC/BS), but once that group was in agreement, it was necessary to extend our efforts to the emergency physicians at those hospitals. Emergency physicians are responsible for 44% of all inpatient admissions (Gonzalez Morganti et al., 2013) and frequently evaluate patients with cellulitis. We involved an emergency physician who was well known in the community as well as nationally to aid us in understanding the culture of these physicians. This physician helped us understand that emergency physicians may be very conservative with their treatment because they often cannot rely on timely outpatient followup. Therefore, we included in our program next-day access to a dermatologist who would confirm the diagnosis and alter treatment as necessary.
The program now has four components: 1) a physician educational intervention with associated continuing medical education (CME) credit available to both primary care physicians as well as emergency physicians, 2) a care protocol that involves point-of-care clinical decision support using a computerized visual diagnostic clinical decision support system available online at each of the institutions and by smartphone, 3) a system to ensure that discharged patients can be seen and reevaluated within 24 hours by a dermatologist if there is concern, and 4) a community-wide communications program directed at patients and providers in the problem area. An important component of this communication program was having a “champion” at each site to answer questions and encourage use of the program.
Keys to our successful implementation of the QI initiative are the partnership between the hospitals, care providers, and insurance provider; incorporating representatives of the provider groups involved to develop strategies that work best for each group; and utilizing local champions who know the local culture and workflow (essential) and can encourage the use of the QI tool.
CME Physician Training
The first component of the initiative involves CME physician training in the problem area of cellulitis and skin and soft tissue infection. The CME is an online video and interactive program covering the differential diagnosis of presentation with a red leg and clinical teaching on the differential diagnosis. The program is delivered in person at emergency department staff meetings and is available online. It is important to note that online education may be the best way to reach emergency physicians, as it is impossible to get the entire staff together at the same time given their 24/7 shift work. Additional training in use of clinical decision support is available. The decision support can be linked from the electronic medical records. The CME training is accredited by the medical liability insurer Coverys. This company is particularly interested in decreasing diagnostic error and encourages the use of diagnostic criteria to decrease such error.
Training includes cellulitis diagnosis and management as well as differential diagnosis of stasis dermatitis, since stasis dermatitis is most commonly misdiagnosed as cellulitis. In a study of suspected cellulitis cases conducted at the University of Rochester and UCLA, the most common alternate diagnosis subsequently provided by the dermatologist or infectious disease physician was stasis dermatitis, and this diagnosis was found in 37% of the suspected cellulitis cases (David et al., 2011). Because treatment strategies are quite different for cellulitis and stasis dermatitis, differentiation of these two diagnoses is important to minimize the error rate and improve patient care. Thus, training emphasis will be placed on the differential diagnosis of stasis dermatitis and cellulitis. To evaluate the impact of this physician training, the educational training methods will be assessed by user survey and will include metrics of both user satisfaction and impact on knowledge and practice approach.
An iterative approach will define the best educational methods.
Care Protocol
The second component of this QI initiative involves the development of a straightforward care protocol to complement training and to augment the diagnostic process of suspected soft tissue infections (Figure 1). It is important to busy primary care and emergency physicians that this protocol is easily accessed, simplistic and can be used rapidly. Three cognitive pathways comprise the protocol. The first pathway is defined as “probable cellulitis” and includes patients presenting with unilateral redness, history of skin injury preceding the redness, fever, increased leukocyte count, or lymphangitic spread. The second pathway is defined as “Consider Broad Differential Diagnosis” and includes patients with signs of chronicity or recurrence, scaling skin, or reports of itch greater than pain. The third pathway, which is defined as “Unlikely Cellulitis,” includes patients with bilateral redness and chronicity or recurring processes. This protocol will be enhanced with handheld and online visual diagnostic clinical decision support. Beginning with a presentation of red skin in the clinic or emergency department, the provider can then consider other symptoms before reaching a diagnosis and prescribing appropriate laboratory tests, observation, and/or therapeutic interventions. This triage protocol facilitates discrimination between true cellulitis and other similar diagnoses quickly and efficiently. Cognitive studies have shown that inclusion of the correct diagnosis in the differential diagnosis within the first 6 minutes of cognitive processing increases the likelihood of giving the correct diagnosis (Norman, 2009). In the event that the clinical presentation suggests a diagnosis other than cellulitis, such as stasis dermatitis, the provider can then consider a broad differential diagnosis.
Triage Protocol for Red Skin (Suspected Cellulitis)
Refer to this workflow for patients with red skin of the leg.
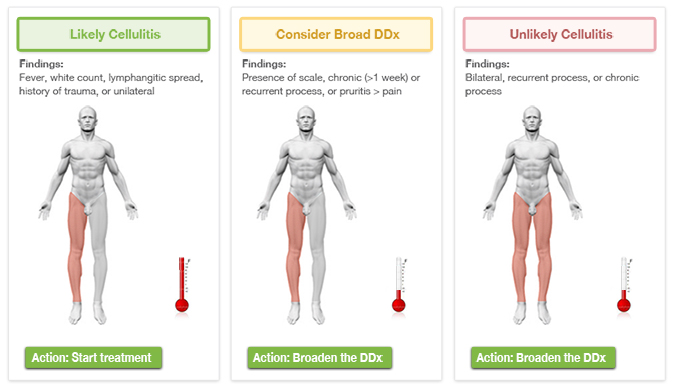
Figure 1. Triage Protocol
Such a differential diagnosis is facilitated by the use of a visually based, computerized clinical decision support system for diagnosis at the point of care (see www.visualdx.com). This web-based clinical decision support system links the benefits of conventional clinical decision support with a visually guided, problem-oriented search methodology to generate a differential at the point of care. The specialized tool broadens the differential diagnosis when provided with information regarding a patient with erythema and edema of the skin or with presumed cellulitis. The ability to generate a robust differential diagnosis within seconds replete with immediate display of variant images for each condition as well as additional textual information about the conditions is advantageous for accurate diagnosis. With this system a visual differential diagnosis is displayed in fewer than 5 seconds, and in the case of suspected cellulitis, the results are narrowed from 70 possible diagnoses and 1,157 disease images including images of both light and dark skin. In a previous study of the diagnostic accuracy of cellulitis, this system was shown to include the correct diagnosis in the differential diagnosis more frequently than diagnosis by the admitting team (64% vs. 14%; David et al., 2011).
Importantly, this visual differential diagnosis system captures the variation in the disease, a quality that makes diagnosis of cellulitis difficult. Cellulitis can occur on almost any body location, although the majority of cases involve the foot and leg or hand and arm. One benefit to this clinical decision support system is the inclusion of 867 images of cellulitis presentation on various body sites and at various stages of disease as well as in patients of different genders, races, and ages. Indeed, serious infections of the skin (as well as noninfectious diseases of the skin) are included for each body location within the differential diagnosis. In order to fully take advantage of this system, this point-of-care clinical decision support will be supported by physician training and will be monitored for use and search strategies.
Timely Access to Specialty Care
Conversations with the end user (the emergency physicians) identified a common barrier to discharging patients with a questionable diagnosis of cellulitis. These physicians felt they would be more likely to discharge a patient if they were assured the patient could receive care promptly. Working with community resources, we were able to ensure access for these patients. This provided incentive for emergency physicians to use the program.
Medical Community Communication
The final component of this QI involves communication within the medical community around the issue of cellulitis. Nurse and mid-level training and triage are crucial elements in this initiative. Similar to the previous studies aimed at decreasing bloodstream infections in central line recipients (e.g., Berenholtz et al., 2004; Marsteller et al., 2012), this initiative relies on the active engagement of nurses and mid-level providers in the problem workflow. The developed protocol is integrated with current guidelines for emergency room triage protocols in order to be incorporated into the workflow. Additionally, ongoing reference materials and learning guides will be offered to propel the initiative. Project participants will receive quarterly updates on the number of hospital admissions for cellulitis at their institution and the other institutions in the community. Sharing of the cellulitis hospital admission rate through a “dashboard” will allow the participants to see how their community “competitors” are doing and will serve to encourage each participating institution to be even more engaged.
Evaluation
The hospitals will also provide de-identified admissions data for assessment and monitoring. From this community-wide data, the impact of the program on the number of admissions for cellulitis will be assessed. Blue Cross Blue Shield will provide de-identified data on admissions and on costs associated with the misdiagnosis of cellulitis and other soft tissue infections.
Broad Implications of Quality Initiatives Focused on Diagnostic Accuracy
This four-pronged approach to improve the diagnostic accuracy of physicians incorporates physician training, guidance by a concrete care protocol, use of a proven computerized visual diagnostic clinical decision support system, engagement of the end users with attention to their perceived barriers, and ongoing communication with patients and providers. Ultimately, we expect to observe a reduction in the number of false positives and a concomitant decrease in hospital admissions based on the incorrect diagnosis of cellulitis. A significant increase in correct diagnosis will decrease the number of hospital admissions, prevent overuse of antibiotics, expose fewer people to nosocomial infections, and save considerable healthcare costs. As mentioned earlier, current estimates indicate that healthcare expenses of $1,368,000,000 are incurred annually in the United States due to the misdiagnosis of cellulitis. In a climate of economic tightening and healthcare reform, a QI initiative that is aimed at decreasing this figure significantly and improving patient care and patient outcome is essential. Furthermore, this QI initiative includes an innovative approach to medicine and facilitates the discovery of new methods in clinician education and care, thereby paving the way for more comprehensive health services research in this problem-solving area.
In its current iteration, this initiative is focused on a specific diagnostic problem, that of cellulitis, but successful development of the prototype will allow expansion to a wide variety of diagnostic problems in the areas of infectious disease and dermatology as well as across other medical fields. Following successful implementation of this initiative, the investigators will combine the protocol with an innovative management algorithm to decrease extended inpatient hospital stays. This algorithm may involve home monitoring, home antibiotic infusion, or observation and may include direct consumer-nurse interaction or visiting nurse teleconsultation. In the future, telemedical consult intervention may be a logical additional step to the protocol in cases where the admitting physician is not completely confident in the diagnosis after using the visual clinical decision support system. The attending physician could send images and case details to an on-call dermatologist through a mobile telemedical interface. This consulting expert could then provide diagnostic confidence and learning links via the clinical decision support system. Thus, the success of this initiative will serve as the basis for widespread expansion of the QI initiative and concomitant global reduction of misdiagnosis, which, in turn, helps everyone: the patient, the provider, and the payor.
Patricia Gogniat is a medical information specialist for Logical Images, Inc. She obtained her bachelor’s degree from the University of Rochester in Rochester, New York, and a master’s degree in library and information science from the State University of New York at Buffalo. Her research interests include diagnostic error, standardized terminology, and EHR integration of point-of-care resources. Gogniat may be contacted at pgogniat@logicalimages.com.
Art Papier is co-founder and CEO of Logical Images, Inc., and an associate professor of dermatology and medical informatics at the University of Rochester School of Medicine and Dentistry in Rochester, New York. Papier developed VisualDx, a widely used point of care diagnostic clinical decision support system. He also conducts research in diagnostic errors with particular interest in the misdiagnosis and inappropriate therapy around soft tissue infections. Papier received his MD from the University of Vermont College of Medicine and completed his graduate medical training in dermatology at the University of Rochester Medical Center. He serves on the board of the Society to Improve Diagnosis in Medicine and may be contacted at apapier@logicalimages.com.
Sandra Schneider is professor and chair of the Department of Emergency Medicine at the University of Rochester, emergency physician-in-chief at Strong Memorial Hospital, and attending physician at Highland Hospital, all in Rochester, New York. She is also immediate past chair of the Emergency Medicine Foundation and past chair of the Society of Academic Emergency Medicine. Schneider received her MD from the University of Pittsburgh School of Medicine and completed her residency in internal medicine at the University of Pittsburgh.
References
Berenholtz, S. M., Pronovost, P. J., Lipsett, P. A., Hobson, D., Earsing, K., Farley, J. E., Milanovich, S., Garrett-Mayer, E., Winters, B. D., Rubin, H. R., Dorman, T., & Perl, T. M. (2004). Eliminating catheter-related bloodstream infections in the intensive care unit. Critical Care Medicine, 32(10), 2014-2020.
Cabana, M. D., Rand, C. S., Powe, N. R., Wu, A. W., Wilson, M. H., Abboud, P. A., & Rubin, H. R. (1999). Why don’t physicians follow clinical practice guidelines? A framework for improvement. The Journal of the American Medical Association, 282(15):1458–1465.
Centers for Disease Control and Prevention. (2010, December 13). Healthcare-associated infections. Retrieved from http://www.cdc.gov/hai/burden.html
David, C. V., Chira, S., Eells, S. J., Ladrigan, M., Papier, A., Miller, L. G., & Craft, N. (2011). Diagnostic accuracy in patients admitted to hospitals with cellulitis. Dermatology Online Journal, 17(3):1.
Gonzalez Morganti, K., Bauhoff, S., Blanchard, J. C., Abir, M., Iyer, N., Smith, A., Vesely, J. V., Okeke, E.N., & Kellermann, A. L. (2013). The Evolving Role of Emergency Departments in the United States. Santa Monica, CA: RAND Corporation. Retrieved from http://www.rand.org/pubs/research_reports/RR280.html
Graber, M. (2005). Diagnostic errors in medicine: A case of neglect. Joint Commission Journal on Quality and Patient Safety, 31(2), 106-113.
Groopman, J. (2007). How Doctors Think. New York, NY: Houghton Mifflin Company.
Hällgren, J., Tengvall-Linder, M., Persson, M., & Wahlgren, C. F. (2003). Stevens-Johnson syndrome associated with ciprofloxacin: A review of adverse cutaneous events reported in Sweden as associated with this drug. Journal of the American Academy of Dermatology, 49(5 Suppl), S267-S269.
Hersh, A. L., Chambers H. F., Maselli, J. H., & Gonzales, R. (2008). National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Archives Internal Medicine, 68(14), 1585-1591.
Hirschmann, J. V. & Ragi, G. J. (2012). Lower limb cellulitis and its mimics. Journal of The American Academy of Dermatology, 67(2), 163-184.
Klein, E., Smith, D. L., & Laxminarayan, R. (2007). Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus. United States, 1999-2005. Emerging Infectious Diseases, 13(12), 1840-1846.
Klevens, R. M., Edwards, J. R., Richards, C. L. Jr., Horan, T. C., Gaynes, R. P., Pollock, D. A., Cardo, D. M. (2007). Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports, 122(2), 160-166.
Kohn, L. T., Corrigan, J. M., Donaldson, M. S. (Institute of Medicine) (2000). To Err is human: Building a safer health system. Washington, DC: National Academy Press.
Levell, N. J., Wingfield, C. G., & Garioch, J. J. (2011). Severe lower limb cellulitis is best diagnosed by dermatologists and managed with shared care between primary and secondary care. British Journal of Dermatology, 164(6), 1326-1328.
Marsteller, J. A., Sexton, J. B., Hsu, Y., Hsiao, C., Holzmueller, C. G., Pronovost, P. J., & Thompson, D. A. (2012). A multicenter, phased, cluster-randomized controlled trial to reduce central line-associated bloodstream infections in intensive care units. Critical Care Medicine, 40(11), 2933-2939.
Newman-Toker, D. E., & Pronovost, P. J. (2009). Diagnostic errors–the next frontier for patient safety. The Journal of the American Medical Association, 301(10), 1060-1062.
New York State Department of Health (February 7, 2013). Amendment of Sections 405.2 and 405.4 of Title 10 NYCRR (Hospital Sepsis Protocols). Retrieved from http://www.health.ny.gov/facilities/public_health_and_health_planning_council/meetings/2013-02-07/docs/13-01.pdf
Norman, G., (2009). Dual processing and diagnostic errors. Advances in Health Science Education Theory and Practice, 14(Supplement 1), 37-49.
Roujeau, J., Kelly, J. P., Naldi, L., Rzany, B., Stern, R. S., Anderson, T., Auquier, A., Bastuji-Garin, S., Correia, O., Locati, F., Mockenhaupt, M., Paoletti, C., Shapiro, S., Shear, N., Schöpf, E., & Kaufman, D. W. (1995). Medication use and the risk of Stevens–Johnson syndrome or toxic epidermal necrolysis. New England Journal of Medicine, 333(24), 1600-1607.
Saber Tehrani, A. S., Lee, H., Mathews, S. C., Shore, A., Makary, M. A., Pronovost, P. J., & Newman-Toker, D. E. (2013). 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: An analysis from the National Practitioner Data Bank. BMJ Quality and Safety, doi:10.1136/bmjqs-2012-001550.
Solucient (2006). The DRG handbook comparative clinical and financial benchmarks. Evanston,IL: Solucient.
