Problem-Solving in Prevention of Type 2 Diabetes Mellitus in Older People
By Ana Veiga and Cristina Vaz de Almeida
In recent years, we have seen increased incidence and prevalence of Type 2 diabetes mellitus. This condition affects 415 million people worldwide, with a projected increase of 642 million by 2040 (Observatório Nacional da Diabetes [OND], 2015). In Portugal, more than 1 million people suffer from this disease, with a 23% increase in prevalence (Direção-Geral da Saúde [DGS], 2017) in people ages 65–74.
Health literacy plays a key role in the management, control, and prevention of disease in general. However, it is of particular importance in diabetes, due to both the disease’s chronicity and its effect on quality of life (DGS, 2016). Effectively, health literacy levels directly influence overall quality of life, especially in the elderly population (Panagioti et al., 2018).
Given that about 50% of the European population has low levels of health literacy (Sorensen et al., 2012) and therefore has difficulty accessing, understanding, and using health information (Nutbeam, 1998), and also given that 25% to 40% of the population has low levels of activation (Hibbard & Gilburt, 2014), trust in health task management and knowledge can be paralleled with the concept of active and inactive audiences (Grunig & Hunt, 1984).
There is a two-way relationship between health literacy and cognitive disability in older people (Oliveira, Bosco, & di Lorito, 2019). Health literacy is mediated through an individual’s education, culture, and language. Equally important are the communication and assessment skills of health professionals with whom individuals interact, as well as the ability of the media, the market, and the government to provide health information appropriately to their target audiences (World Health Organization, 2017).
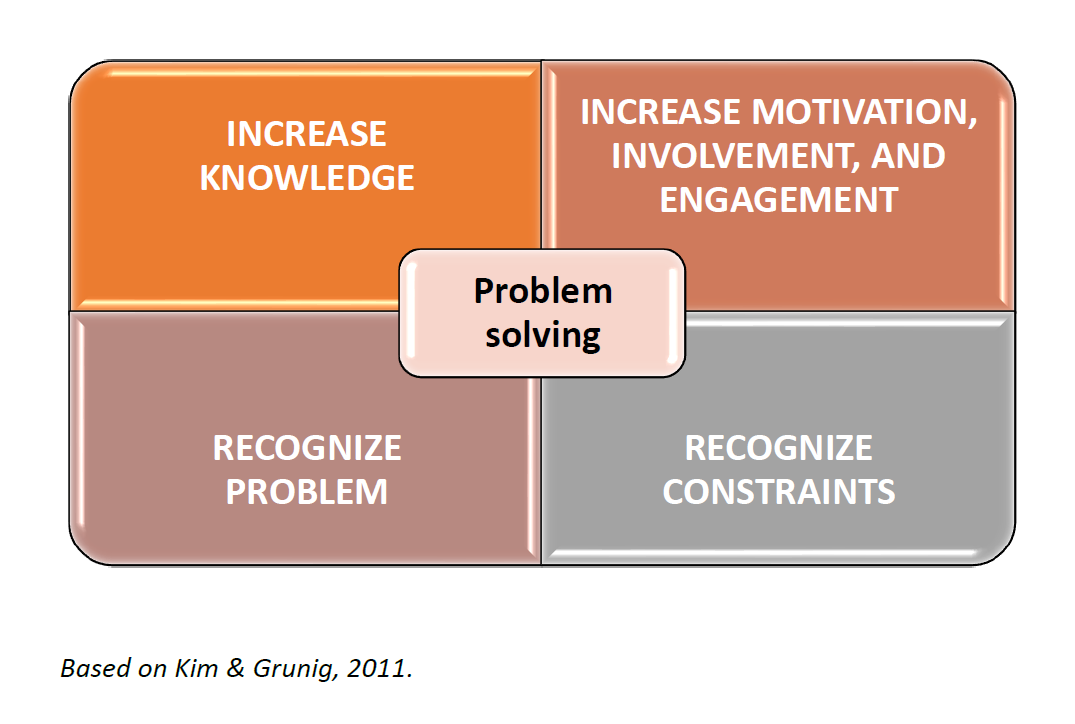
Communication is the structural basis for health literacy (Almeida, 2019). Under the situational theory of audiences (Grunig, 1997), although patient constraints exist—especially related to poor health literacy—recognition of the problem allows one to identify situations that need to be addressed.
Grunig and Hunt (1984) identified three important variables in human behavior that can be associated with the health profile, in particular the behaviors of patients and health professionals: 1) the level of involvement with the organization’s action; 2) the recognition of the problem, which includes the search for information and its processing; and 3) the recognition of existing constraints.
Grunig (1997) stated that people become systematic when they see that information can solve their problems, selectively investing their cognitive and communicative resources in a problem when they see that their effort is necessary and relevant (Kim & Grunig, 2011). We have two elements to consider here: the problem and its resolution (Kim & Grunig, 2011). In this sense, the elderly population—which fits into a low health literacy profile, with high constraints (beliefs, attitudes, and behaviors)—being stimulated/motivated with more knowledge and involvement (Kim & Grunig, 2011) allows for change behavior to be more effective (Bandura, 1993).
Methodology
This is a descriptive study with a convenience sample. The European Health Literacy Survey (HLS-EU-PT) questionnaire was translated and validated for Portugal. Data were collected after informed consent from the elderly and authorization from their organization for study and evaluation purposes.
Descriptive and inferential statistics techniques were employed using the IBM SPSS Statistics software, version 25.
Sample characterization
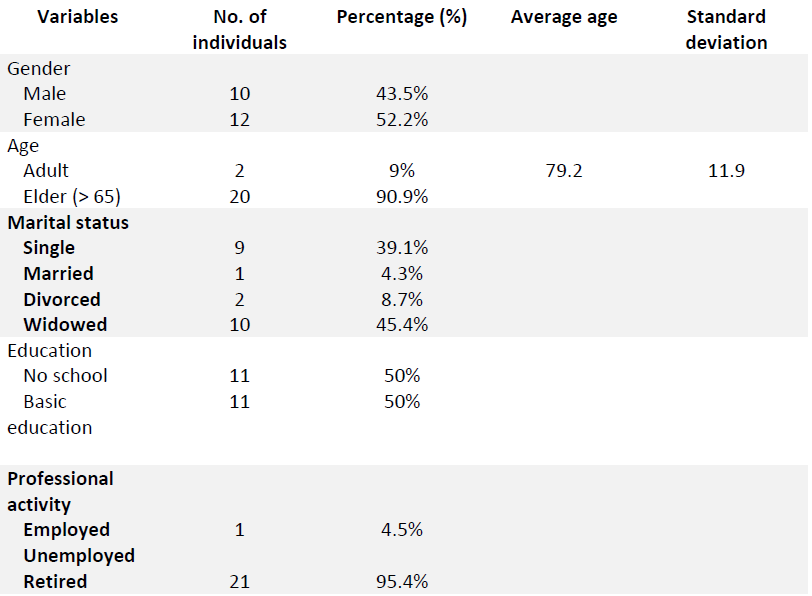
This study counted on the participation of 22 mostly female (52.2%) seniors from the Angel Day Center. Ages range from 52 to 99, with an average of 79.2. Regarding marital status and professional activity, most are widowers (45.4%) and retired (95.4%). Regarding literacy, 50% of the sample have no schooling, and another 50% have basic education, as shown in Table 1.
In addition to the financial situation, we drew our attention to the fact that the majority (86%) live alone and 45% are widowed. Regarding the type of housing, a very significant percentage (77%) stated that they live in a single room, which is an aspect that could contribute to the change in eating behaviors, quality of life, and well being.
Table 1: Sociodemographic Characteristics of Elderly Patients at Lisbon Angel Day Center
Regarding health literacy, 18.2% were at a problematic level and 63.6% were at an inadequate level. Most participants were at the inadequate level on the different dimensions of the scale, particularly healthcare, disease prevention, and health promotion.
Age, education, and lifestyles affect older people’s knowledge and action on their health
Some doctors state that the elderly do not obey medical indications and that “the lack of reading and writing skills often leads to errors in medication dosing,” attributing responsibility to issues of education, knowledge, age, and isolation (Benavente et al., 1996). Nearly two decades later, Sorensen et al. (2012) found that poor health literacy generates adverse effects on care in this field and motivates more hospitalizations, more frequent use of emergency services, and a lower prevalence of preventive individual and family attitudes.
The results show a sample of mostly elderly female (52%), with an average age of over 65 years (91%). This population is more highly predisposed to developing Type 2 diabetes (OND, 2015; American Diabetes Association, 2019). Regarding literacy in general, 50% of the sample basic education (fourth grade), 5% can only read and write, and 14% are illiterate. Regarding health literacy specifically, 28.6% of the elderly are at a problem level, while 61.9% have an inadequate level of health literacy. This study corroborates the outcome profile of national health literacy studies (Nunes, 2014; Espanha et al., 2016; Pedro et al., 2016).
We found in this study that there are dietary patterns that do not follow the National Directorate of Health (DGS 2004) guidelines regarding having a national plan for the elderly (2004). In fact, we note several factors that influence eating behavior: genetic, psychological, sociocultural, and environmental (Pender, 1996).
Among factors that impact behavior change or maintenance of healthy behavior, psychosocial factors (loss of spouse, social isolation, poverty) play a larger role (Campos et al., 2000). The presence of economic difficulties means less purchasing power and, consequently, less ability to purchase nutritious foods (DGS, 2004).
If there is no mechanism to get a patient motivated to solve a problem, the patient’s passive attitude in the acquisition, selection, and transmission of information will be maintained (Kim & Grunig, 2011). Health professionals want these “latent” patients to recognize the problem, get involved (Kim & Grunig, 2011), and become active patients.
Professional-patient communication is an interpersonal, critical caregiving process (Kreps, 1988) that occurs within a specific cultural framework (Wonca, 2002). Health communication at the interpersonal, group, and societal level allows the transmission of verbal and nonverbal messages and can promote healthy behaviors (Almeida, 2019).
In the literature, we find models focused on communication skills of health professionals and approaches emphasizing a humanized relationship that accounts for cultural factors and psychosocial assumptions, thus making the communication more effective.
Following Kim and Grunig (2011), the public wants the recognition and organization of people in the face of a particular problem and the existence of a way to solve it. Thus, if a person realizes that there is a problem, understands what it is, and finds few obstacles in relation to investigating it, the person will probably be able to do some research and provide information about the problem (Kim & Grunig, 2011). But this does not always happen, particularly among those who have the most difficulty accessing, understanding, and using health information (Sorensen et al., 2012).
Also, even when patients are activated to make shared decisions, they often voluntarily delegate those health decisions, such as gaining knowledge about the subject, to professionals (Levinson, Kao, & Thisted, 2005).
Grunig and Hunt (1984) identified three important variables in the manifestation of the behavior of various audiences, in particular patients and health professionals: 1) level of involvement with the organization’s action; 2) recognition of the problem, which includes the search for information and its processing; and 3) recognition of existing constraints. These three variables allow for the segmentation of audiences into assets and liabilities. Active audiences show interest in the organization and activity they are trying to influence, and are close to the profile of patients with adequate or high health literacy. Therefore, they are participative, from the perspective of Hallahan (2000).
In parallel with the profile of active, latent, and passive audiences, Hibbard and Gilburt (2014) highlight four activation levels that individuals may possess. Individuals at level 1 tend to be passive and feel overwhelmed in managing their own health; they may not understand their role in the care process (Hunt & Grunig, 1994). These inactive audiences are distinguished from active audiences by their low level of knowledge, low involvement, and constraints in their actions, and may be associated with a patient profile that indicates low education, low socioeconomic status, elderly age, or being a migrant with difficulty understanding Portuguese Espanha, Avila, & Mendes, 2016). Such individuals are likely to have low, inadequate, or problematic health literacy (Sorensen et al., 2012). Passive audiences show no interest in either organization or activity (Hunt & Grunig, 1994). Thus, it is possible to include in this category those individuals who, despite resorting several times a year to health services (low health literacy), do not obtain optimal health results due to lack of adherence and do not make good health decisions (Sorensen et al., 2012).
At level 2, individuals may lack the knowledge and confidence to manage their health (Hibbard and Gilburt, 2014). Individuals at level 3 act, but may not yet have the confidence and competence to support their behaviors. Grunig and Repper (1992) identified latent audiences, which only become active when stimulated (e.g., through communication from a health professional). In this profile, low-literacy patient (Sorensen et al., 2012) and individuals at levels 2 and 3 are described by PAM (Hibbard and Gilburt, 2014). In levels 2 and 3, we can also integrate Hallahan’s (2000) intermediate audiences. Hallahan (2000) distinguishes between conscientious audiences, with high knowledge and low involvement in their actions (since they are not directly affected by them), and stimulated audiences, with high involvement but little knowledge. By association, the latter can even include people with a high degree of general literacy (Doak, Doak, & Root, 1996) but without a high degree of health literacy, such as medical terms or related knowledge.
And finally, level 4 individuals, in parallel with active audiences, have adopted many of the behaviors necessary to support their health but may not be able to cope with life’s stress (Hibbard & Gilburt, 2014).
Audiences (patients) invest in information and communicative action to solve problems and therefore tend to act when effort is perceived as necessary to meet a biological, psychological, or social need (Grunig, 1997; Kim & Grunig, 2011).
A person who intends to solve a problem will only Increase his or her communicative activity (Street, 2007) when obtaining information is perceived as useful (Littlejohn, 1982). Enabling these inactive audiences assumes a combination of greater knowledge and engagement (Kim & Grunig, 2011) along with motivation (Sorensen, 2012).
The recognition of constraints (beliefs, barriers) discourages the individual, who perceives the existence of obstacles (Grunig, 1997), or, in Bandura’s (1986) terminology, the lack of self-efficacy. For patients’ self-efficacy to be verified, they must be able to exercise control over the events that affect their life (Bandura, 1993). Without motivation to solve their problem (which can be prompted through the attitude and behavior of health professionals), passivity can manifest itself in the acquisition, selection, and transmission of information (Kim & Grunig, 2011) concerning that problem (Grunig & Hunt, 1984).
The solution? Increase knowledge, lower constraints, and improve lifestyles knowledge
Low health literacy is directly related to insufficient knowledge in the field of chronic diseases. Since lifestyles relate directly to the development of chronic diseases, it is essential to ensure interventions tailored to the promotion of literacy and directed to the needs of the elderly population (Davey et al., 2015). Indeed, community intervention through a structured health literacy program that encourages increased physical activity and healthy eating has significant health effects on diabetes risk factors (Jenum et al., 2006).
Programs should include strategies to raise awareness, improve knowledge, and change attitudes towards physical activity and healthy eating through training actions, information leaflets, informal meetings, the media, etc. (Borman et al., 2003).
Figure 1: Situational theory of problem solving
References
Almeida, C. V. (2019). Modelo de comunicação em saúde ACP: As competências de comunicação no cerne de uma literacia em saúde transversal, holística e prática. In C. Lopes & C. V. Almeida (Coords.), Literacia em saúde na prática (pp. 43–52) [Ebook]. Edições ISPA.
American Diabetes Association. (2019). Standards of medical care in diabetes—2019. Diabetes Care, 42(Suppl. 1), S1–S2. https://doi.org/10.2337/dc19-Sint01
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavior change. Psychological Review, 84(2), 191–215. https://doi.org/10.1037/0033-295X.84.2.191
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs: Prentice-Hall.
Bandura, A. (1993). Perceived self-efficacy in cognitive development and functioning. Educational Psychology, 28, 117-148.
Bandura, A. (Ed.). (1999). Self-efficacy in changing societies. Cambridge University Press.
Belim, C., & Vaz de Almeida, C. (2017). Healthy thanks to communication: A model of communication competences to optimize health literacy: Assertiveness, clear language, and positivity. In V. E. Papalois & M. Theodospoulous (Eds.), Optimizing health literacy for improved clinical practices (pp. 124–152). IGI Global.
Benavente, A., Costa, A. F., Rosa, A., & Ávila, P. (1996). A literacia em Portugal: Resultados de uma pesquisa extensiva e monográfica. Fundação Calouste Gulbenkian.
Borman. W.C., Ilgen, D.R., & Klimoski, R.J. Vol. Eds.). (2003). Handbook of Pshychology, Hoboken, N.J: Wiley.
Campos, M., Monteiro, J., & Ornelas, A. (2000). Fatores que afetam o consumo alimentar e a nutrição do idoso. Revista Nutrição, 13(3), 157–165. https://doi.org/10.1590/S1415-52732000000300002
Davey, J., Holden, C. A., & Smith, B. J. (2015). The correlates of chronic disease-related health literacy and its components among men: a systematic review. BMC Public Health, 15(589). https://doi.org/10.1186/s12889-015-1900-5
DGS. (2004). Programa nacional para a saúde das pessoas idosas. Lisboa. Direção-Geral da saúde.
Direção-Geral da Saúde. (2016). A saúde dos portugueses. Lisboa. Direção-geral da saúde.
Direção-Geral da Saúde. (2017). Programa Nacional para a Diabetes 2017. Lisboa. Direção-geral da saúde.
Doak, C. C., Doak, L. G., Friedell, G. H., & Meade, C. D. (1998). Improving comprehension for cancer patients with low literacy skills: Strategies for clinicians. Ca: A Cancer Journal for Clinicians, 48(3), 151–162.
Doak, C. C., Doak, L., G., & Root, J. H. (1996). Teaching patients with low literacy. J. B. Lippincott Company.
Espanha, R., & Ávila, P. (2016). Health Literacy Survey Portugal: A contribution for the knowledge on health and communications. Procedia Computer Science, 100, 1033–1041. https://doi.org/10.1016/j.procs.2016.09.277
Grunig, J. E., & Hunt, T. (1984). Managing public relations. Rinehart and Winston.
Grunig, J. E. (1993). Implications of public relations for other domains of communication. Journal of Communication, 43(3), 164–173. https://doi.org/10.1111/j.1460-2466.1993.tb01289.x
Grunig, J. E. (1997). A situational theory of publics: Conceptual history, recent challenges and new research. In D. Moss, T. MacManus, & D. Vercic (Eds.), Public relations research: An international perspective (pp. 3–48). International Thomson Business Press.
Grunig, J. E., & Repper, F. C. (1992). Strategic management, publics and issues. In J. E. Grunig (Ed.), Excellence in public relations and communication management (pp. 117-157). New Jersey: Lawrence Erlbaum.
Hallahan, K. (2000). Inactive publics: The forgotten publics in public relations. Public Relations Review, 26(4), 499–515.
Hibbard, J., & Gilburt, H. (2014). Supporting people to manage their health. An introduction to patient activation. King’s Fund. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/supporting-people-manage-health-patient-activation-may14.pdf
Huizinga, M. M., Carlisle, A. J., Cavanaugh, K. L., Davis, D. L., Gregory, R. P., Schlundt, D. G., & Rothman, R. L. (2009). Literacy, numeracy, and portion-size estimation skills. American Journal of Preventive Medicine, 36(4), 324–328. https://doi.org/10.1016/j.amepre.2008.11.012
Hunt, T., & Grunig, J. E. (1994). Public relations techniques. Fort Worth: Harcourt Brace College Publishers.
Jenum, A. K., Anderssen, S. A., Birkeland, K. I., Holme, I., Graff-Iversen, S., Lorentzen, C., Ommundsen, Y., Raastad, T., Ødegaard, A. K., & Bahr, R. (2006). Promoting physical activity in a low-income multiethnic district: Effects of a community intervention study to reduce risk factors for type 2 diabetes and cardiovascular disease. Diabetes Care, 29(7), 1605–1612. https://doi.org/10.2337/dc05-1587
Levinson, W., Kao, A., Kuby, A., & Thisted, R. A. (2005). Not all patients want to participate in decision making. A national study of public preferences. Journal of General Internal Medicine, 20, 531-535.
Littlejohn, S. W. (1982). Fundamentos teóricos da comunicação humana. Zahar Editores.
Lopes, C. A., & Almeida, C. V. (2019). Introdução. In C. Lopes & C. V. Almeida (Coords.), Literacia em saúde na prática (pp. 17-23) [Ebook]. Edições ISPA.
Kim, J.-N., & Grunig, J. E. (2011). Problem solving and communicative action: A situational theory of problem solving. Journal of Communication, 61(1), 120–149. https://doi.org/10.1111/j.1460-2466.2010.01529.x
Kreps, G. L. (1988). Relational communication in health care. Southern Speech Communication Journal, 53, 344-359.
Nunes, L. S. (2014). Literacia para a saúde e a conscientização da cidadania positiva. Revista de Enfermagem Referência, Série III(11 Supl.), 94–99.
Nutbeam, D. (1998). Health promotion glossary, Health Promotion International, 13, 349-364.
Observatório Nacional da Diabetes (2015). Diabetes: factos e números 2015. Relatório Anual do Observatório Nacional da Diabetes. SNS.
Oliveira, D., Bosco, A., & di Lorito, C. ( 2019). Is poor health literacy a risk factor for dementia in older adults? Systematic literature review of prospective cohort studies. Maturitas ( IF 3.654 ) DOI: 10.1016/j.maturitas.2019.03.010
Panagioti, M., Skevington, S. M., Hann, M., Howells, K., Blakemore, A., Reeves, D., & Bower, P. (2018). Effect of health literacy on the quality of life of older patients with long-term conditions: A large cohort study in UK general practice. Quality of Life Research, 27, 1257–1268. https://doi.org/10.1007/s11136-017-1775-2
Pender, N. J. (1996). Health promotion in nursing practice (3rd ed.). Stanford, CT: Appleton and Lange.
Pedro, A. R., Amaral, O., & Escoval, A. (2016). Literacia em saúde, dos dados à ação: Tradução, validação e aplicação do European Health Literacy Survey em Portugal. Revista Portuguesa de Saúde Publica, 34(3), 259–275. https://doi.org/10.1016/j.rpsp.2016.07.002
Sorensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., Brand, H., & (HLS-EU) Consortium Health Literacy Project European. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12(80). https://doi.org/10.1186/1471-2458-12-80
Street, R.L. (2007). Aiding medical decision making: a communication perspective. Medical Decision Making, 550-553.
WONCA. Definição Europeia de Medicina Geral e familiar (Clinica Geral/Medicina Familiar). Europa: WONCA, 2002.
World Health Organization (2017). Who strategic communications framework. Geneva: World Health Organization Department of Communications.
