Point-of-Care Medication Error Preventio: Best Practices in Action
May / June 2007
Point-of-Care Medication Error Prevention
Best Practices in Action

![]()
Photo Courtesy of IntelliDOT
Since the industry-wide wake-up call prompted by the Institute of Medicine’s landmark report To Err Is Human (2000) and the follow-up report Preventing Medication Errors (2006), patient safety has become one of the foremost concerns in healthcare, with the prevention of medication errors in acute care settings as a key priority. The reports estimate that at least 1.5 million preventable medication errors occur each year in the United States, many of which result in adverse drug events (ADEs).
In seeking solutions for medication errors, experts in the healthcare field such as David Bates, MD, PhD, recommend healthcare professionals focus their efforts in certain key areas. In a recent presentation, Dr. Bates listed four specific modalities as key components in medication error prevention: computerized physician order entry (CPOE), IV administration “smart pumps,” computerized adverse drug event monitoring (CADM), and barcode point of care (BPOC) medication safety systems.
While CPOE is often mentioned as the top priority in preventing medication errors, many hospitals have found it difficult to adopt. This has been due to several factors including the lack of support for change from physicians, complexity of the systems both to install and to use, and multiple other infrastructure enablers necessary to make CPOE work. Nonetheless, hospital adoption of CPOE is increasing. Cain Brothers’ summary research report released following the 2007 Health Information Management System Society (HIMSS) meeting in New Orleans in March estimated that 27% of hospitals now have a computer order-entry system in operation for medication orders.
Smart pumps are also becoming more prevalent as older IV pump systems are replaced. CADM, in a limited form, has been a feature in most hospital pharmacy information systems for years; however, this functionality is now moving beyond pharmacy as a standard offering in CPOE and electronic health record (EHR) systems.
![]()
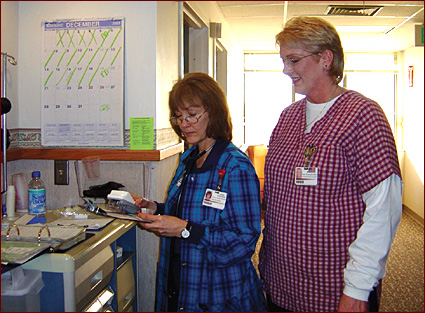
Stillwater Medical Center implemented a BPOC system with hardware that was custom-designed for a nurse’s use. The system has improved communication between nursing and pharmacy, and enhanced the level of patient care.
Photo Courtesy of IntelliDOT
BPOC Adoption
Adoption rates of BPOC systems are also increasing, but not all installations have been successful. According to the Cain Brothers research (2007), 14% of hospitals now have BPOC systems fully implemented, compared to just 5% three years ago. However, Cain Brothers also reports that an additional 12% of hospitals have attempted installations that failed or remain incomplete. Nurses and pharmacists in these facilities provide some insight into the reasons why. Nurses often report that traditional BPOC systems based on off-the-shelf wireless PDAs or a computer on wheels (COWs) are difficult to use.
Sherlyn Hailstone, RN and CEO of St. Joseph’s Hospital in St. Louis, Missouri, tells of her experience purchasing a BPOC system: “After we bought the software from our HIS company, I asked about hardware. The reply was, ‘You can use any hardware you want.’ This illustrates the usability problems with current first generation systems. For the nurse, the hardware user interface is what makes the system either work or not work — the hardware selection is as important as the software design.”
Bonnie Peterson, vice president of patient services at Stillwater Medical Center in Stillwater, Oklahoma, stated, “We looked at BPOC systems based on the COW model, and immediately knew this was not the right choice for our nurses. Nurses working at the bedside need something made for them, something custom-designed to be used at the bedside.”
Pharmacy often has challenges with BPOC implementation as well. The typical hospital stocks approximately 3,000 to 4,000 different pharmaceuticals. In a BPOC environment, all of these medications must have a barcode applied to each unit dose, ready to be scanned by the nurse at the bedside. Thanks to the FDA rule passed in April 2006, all pharmaceuticals sold to hospitals must print a barcode on the smallest unit of measure — the size dispensed to the patient. Despite the ruling, pharmacists still report that 30% or more of their drug stock requires supplemental barcoding.
Marc Rafferty, pharmacy manager at Jane Phillips Medical Center, a 144-bed hospital in Bartlesville, Oklahoma, stated, “Preparation for a BPOC System requires careful planning. Systems must be put in place not only to barcode those medications that lack a manufacturer barcode, but to capture new barcodes that enter our inventory supply in the daily deliveries from our distributors. BPOC systems must have the capability to allow the pharmacy to efficiently keep up with inventory changes and additions, without hours of database updates.”
As these challenges are coming into focus, the evolution of BPOC systems appears to be on the verge of a renaissance of sorts. Through gatherings such as The UnSummit, (www.unsummit.com), an annual symposium specifically focused on barcode point of care technologies and implementation, pharmacists, nurses, and information technologists gather to share their experiences, both good and bad, and spend focused time learning how to make these systems work. UnSummit workshops allow those with successful BPOC implementations to share best practices regarding managing a barcoding program in the pharmacy, formulary management, and many other topics related to operating these essential technologies.
Changes are also occurring on the hardware side, with a new generation of technology that addresses the unique needs of caregivers at the bedside. This technology is coming in the form of hardware designed specifically to meet the workflow and ergonomic needs of nurses, so the devices are intuitive and easy to use, simplifying and improving the human-system interaction. The technology can offer options for both barcode and RFID tag recognition, assuring both accuracy and the greatest comfort for patients. Information can be seamlessly integrated with pharmacy systems, electronic medication administration records (eMAR), and hospital information systems, using an industry standard HL7 interface. Moreover, the clinician’s workflow process can actually be streamlined, despite the added step of verifying medication at the point of care.
Finding the Champion for Change
In any hospital setting, a successful implementation of a patient safety technology at the point of care or BPOC, requires a champion for the technology within the organization. Typically, the champion is serving a role in nursing or pharmacy management, but generally these individuals are characterized by their passion for patient safety and their dedication to both patients and hospital staff.
Nurse managers are often the first to appreciate the ramifications of improved safety measures at the bedside, and are the first to recommend point-of-care technology for medication administration. If nursing finds a system with a device that they find effective and easy to use while allowing for more time with patients, they will become one of the most vocal champions for implementation.
Eileen Dennis, chief nursing officer at Parkview Medical Center in Pueblo, Colorado, said, “We first looked at a patient safety solution, not because we thought we had a problem per se, but out of a desire to give the very best care to patients in our community. Bringing the medication error rate to near zero has been one way to do this.”
 |
|
| Nurses at Jane Phillips Medical Center use a handheld BPOC system to verify medication administration at the patient’s bedside. In addition to confirming the “Five Rights,” this system streamlines workflow by organizing the necessary tasks at the bedside and automating end-of-day charting requirements. Photo Courtesy of IntelliDOT |
However, in order to gain advocates on a hospital-wide basis, Dennis found she needed to engage her entire nursing staff, work closely with the hospital pharmacy staff to accommodate their needs, and build enthusiasm for increasing the use of technology to enhance patient care and reduce costs caused by ADEs. A system that is difficult to use and does not have buy-in from the nursing staff may cause workarounds and will eventually be discontinued. No one will trust the information generated and therefore go to the trouble to keep the system up to date and working. This does not refer to just the computer hardware, but to the human interaction with the system, which makes the system dynamic and viable.
“You have to have everyone fully committed to the use of the technology,” added Dennis, “from nurses who are slow to accept this change, to pharmacy personnel, to senior management, who will appreciate the increased safety along with the ROI these tools produce.”
Champions for medication administration are often found in hospital pharmacy as well. “Hospital pharmacists should have a lead role in medication management issues,” said Rafferty. “That’s our expertise and our responsibility to patients in our care. The more we can do to work with nursing to assure accuracy in the delivery of medication, the better it is for our patients.”
Rafferty’s team deployed a wireless barcode patient safety technology. According to Rafferty, “In the first three weeks after going live, we prevented a number of possible medication errors.” In one instance, a nurse picked up a patient’s medications, only to have the handheld device alert her at the patient’s bedside that the blood pressure (BP) medication was incorrect. In the brief period of time between obtaining the medication to entering the room, the doctor had written the order to stop the medication, the order was sent to the pharmacy, and the pharmacist had entered it into the system. As the nurse prepared to administer the medication, the wireless handheld device alerted her that the BP medicine was no longer prescribed for that patient.
Needs in Nursing
Certainly, nursing staff are passionate about the safety of their patients. Yet, in order to create buy-in and enthusiasm for patient safety technologies at the point of care, hospital executives must take into consideration the daily routine and needs of clinicians using the tool. If the tool adds more work and fails to streamline processes, it will likely be met with resistance. This is particularly true in today’s overworked nursing environment.
The next generation of BPOC systems needs to be designed with recognition of the vast workload that nurses encounter in an average day and integrate easily into the nurse’s workflow from the beginning, decreasing the amount of time nurses spend on paperwork while improving safety at the bedside. There should not be difficult or complicated software to learn; screens should be intuitive and in plain English.
The use of a BPOC solution should create improvements in workflow and streamline ways for nurses to document medication administration, including the ability to create an eMAR that is seamlessly integrated into a pharmacy system, and automation of end-of-day charting requirements for medications delivered during the day.
In research from HIMSS Analytics (2006), nurses noted the importance of providing “a 1:1 ratio of devices to clinicians per shift to ensure information access and remove wait times.” In the case of Parkview Medical Center, for example, as nurses arrive they “check out” their handheld device. They then tell the system which patients they are caring for during their shift. This configuration sets the stage for a host of clinical functions, including personalized reminders assuring documentation to hospital standards, in line with JCAHO requirements.
During medication administration, the handheld technology should guide the nurse through the process, receiving prompts and warnings as configured by the hospital’s pharmacy. If the system is intended to make the workflow easier for nurses, it should document information at the bedside, preferably using just one hand. The handheld devices also should allow nurses to capture and document vital sign information. Likewise, nurse verification of pharmacy order entry allows nurses to double-check medication orders that were computer-entered by a hospital pharmacy.
Under these best practices in point-of-care technology, nurses get more accomplished than just completing medication error checks, confirming the “Five Rights.” They are also able to better organize their work while at the bedside.

![]()
Nurses frequently become strong advocates for BPOC technology once experiencing a “near-miss” error that was caught by the system.
Photo Courtesy of IntelliDOT
However, even armed with all of the benefits that a point-of-care system provides to prevent medication errors, some hospitals will still face resistance from nurses. Installing a system of this nature presents a fundamental change to how the nurse works every day — no matter how easy the transition may be — and this must be addressed. This requires commitment and leadership from the hospital management.
Dennis recently spearheaded a team at Parkview Medical Center in the implementation of a system, and acknowledged that not all nurses want to change. However, once nurses using the system has a “near-miss moment,” where the advantage of the system is made clear, they become passionate advocates for the technology.
“Once nurses experience the value of having such a tool at the bedside,” said Dennis, “the objections disappear.”
In this new era where technology is available to hospitals to prevent many medication errors from occurring, it is not enough to create a tool or system that simply prevents errors. Dennis said, “I can only engage my nurses if I institute a system and device that are reasonable to use. This has to be something that is practical to introduce into the nurse’s everyday work.” Part of the success of these second-generation solutions is that they offer tools easy enough to use that a hospital can hold nurses responsible for using it and following procedure.
The best practices in second-generation point-of-care technology turn over a new leaf for hospital management. There are major implications for how nurse managers are able to supervise their staff, including increased reporting capabilities and visibility into nursing metrics where there was little before, such as: Are medications being given on time? What types of errors is the point-of-care system catching? What are the workload statistics by nurse? What should productivity expectations be? The second-generation technology is able to provide these metrics and usher in a new era of accountability, as well as the ability to document every step in medication administration and more generally in nurse workflow. The data available to hospital management from such a system provides useful information on the 24/7 operation of a hospital unit that has been unavailable to date without extreme monitoring and collection measures. This information on operational variability among units and various shifts can be used to determine and proliferate best practices, thus improving operations in areas beyond medication administration.
Furthermore, if the tool improves patient care and patient safety while actually streamlining the nurse’s workflow, it becomes dramatically easier to demonstrate the advantage of the tool to nurses and paves the way for high levels of compliance. This is also significant for training nurses on the system, which becomes more straightforward and less time-consuming with a tool that is simple to use.
Needs in Pharmacy
Many first-generation systems have also hit roadblocks in adoption because they have not addressed the intricate relationships between teams in the hospital. Nurses are on the front lines of care at the bedside, and they certainly comprise an influential portion of users. However, pharmacy plays an equally vital role in the care process, and the pharmacy’s concerns and questions about how the system will affect their department must be carefully considered. The complexities of pharmacy order entry are a crucial part of enabling nurses to perform their tasks at the bedside.
Pharmacists are understandably anxious about what instituting a new system will mean for their work. Often the pharmacy will ask, “How will the system affect computer order entry of medication orders? How do we assure that all formulary line items are barcoded? How do we get generic replacement and new medications that arrive entered into the database?”
When installing a point-of-care system in a hospital, it is likely that 50% to 60% of the initial work will fall on the pharmacy. For example, once a system is installed, every single medication that a nurse administers to a patient must be labeled and tracked with a barcode. This alone is a daunting task for the pharmacy. Despite the 2006 FDA ruling requiring barcodes on the smallest unit of measure, pharmacists still report that as many as 20% or more of drug stock requires supplemental barcoding.
Pharmacists not only must label each of these medications, but also streamline and revise their computer order entry of medications to be compatible with the new system. Because when a nurse identifies the patient at the bedside, the computer needs to be able to identify the medication, even if it is one of several generic equivalents stocked in the pharmacy.
However, hospital pharmacists can gain numerous efficiencies. Medications and IV orders entered by pharmacists can be sent real-time to nurses carrying a wireless handheld device. Each nurse’s handheld receives the orders, along with configurable warnings and other clinical information. Medications administered prior to pharmacy screening are checked for allergy and drug interactions using industry standard databases.
Rafferty reports improved documentation for hospital pharmacists, as their BPOC documents complex medication administration information, including near-miss data configurable by patient, time, user, and medication.
Additionally, specialized reports reconcile medications administered prior to pharmacy review and order entry with subsequently received medication orders. Pharmacists also gain added confidence in that the handheld device carries caregiver-specific reminders for required tasks and prompts for required documentation.
Team Dynamics: Building Relationships Between Pharmacy and Nursing
Providing care for hundreds of patients daily is truly a team effort. First-generation BPOC systems do not have an emphasis on synchronicity between teams, particularly nursing and pharmacy, which is vital in the hospital. The best practices in second-generation technology not only recognize the needs of each team to allow them to work efficiently, but also provide for built-in dialogue between nursing and pharmacy, to get each team in sync and allow them to work more closely.
For example, a hospital pharmacist may enter a patient’s aspirin order for twice a day, and arrange for it to be administered at 9 a.m. and 5 p.m. However, the nurse may not agree, in that the patient may like to have the aspirin on the same schedule he or she adheres to at home, yet the nurse does not have a way to change the order. That is why Rafferty appreciates the nurse verification of pharmacy order entry feature on his hospital’s BPOC system.
“Now, nurses must verify medication orders prior to administering the medication, rather than just receiving one-sided communication from the pharmacy,” said Rafferty. “If the nurse doesn’t agree with the timing of a medication, or has another concern, the nurse can quarantine the order, send it back to the pharmacy with notes, and have it changed. This feature practically eliminates transcription errors that occur in the pharmacy.”
Bonnie Peterson at Stillwater Medical Center said, “The use of our BPOC has really supported our efforts to improve the relationship between nursing and pharmacy. We thought we had the same set of dosing schedules, but through this learned the two departments had different procedures and standards. Now communications have really improved.”
This built-in tool for dialogue is so important when it comes to reducing medication errors, because both teams have distinct and critical roles when it comes to patient care and safety. The aspirin example, while relatively harmless, is representative of the countless decisions that are made throughout the day in the hospital that jointly involve pharmacy and nursing.
Like hospital pharmacists, physicians appreciate the improved documentation that comes from second-generation BPOC systems, including a summary of medications in an eMAR right from the handheld device. This in turn supports the hospital’s needs in complying with JCAHO requirements, such as documenting pain scale after pain medication is administered, or blood pressure readings after administration of a blood pressure medication.
Conclusion
The healthcare industry is filled with skilled, dedicated, and compassionate professionals, all of whom are deeply committed to the safety of their patients. But hospitals are fast-paced, hectic environments. Without point-of-care technology as an aid, medication errors can and do occur.
Fortunately, as listed by David Bates, there are specific technologies that can be implemented to address these errors. For BPOC, second-generation technology prevents medication errors while being highly usable for the clinician. Where the first generation saw low rates of adoption, the second generation, representing improved technology for human-system interfaces, has seen momentum and acceptance by the healthcare industry.
Medication errors are not a new phenomenon in healthcare, but they can now be effectively addressed and largely resolved through the use of available technology that can meet healthcare’s demand for integrated, practical, and efficient solutions.
Dave Swenson has an extensive background in hospital pharmacy, having spent more than 15 years working in acute care settings, including the Swedish Hospital Medical Center in Seattle. Swenson’s interest in improving patient safety motivated him to join Pyxis Corporation in 1990, where he shared responsibility for the launch of innovative medication and inventory management systems. He is co-founder and COO of IntelliDOT Corporation, which is leading efforts in healthcare to facilitate the adoption of handheld, wireless, BPOC technologies, in order to prevent medication errors at the bedside, as well as improve workflow for nurses. Mr. Swenson is an acknowledged industry expert in the area of pharmacy automation. He can be reached at dswenson@intellidot.net.
References
Cain Brothers. (2007, March 5). “Post-HIMSS HCIT Recap” teleconference with Raymond Falci.
HIMSS Analytics. (2006). Focus group by Jack Price.
Institute of Medicine (IOM). (2000). To err is human: Building a safer health system. Washington, DC: National Academy Press.
Institute of Medicine (IOM). (2006). Preventing medication errors: Quality chasm series. Washington, DC: National Academy Press.
