Patients: How Safe do Patients Feel?
November / December 2005
Patients
How Safe do Patients Feel?
Ever since publication of the Institute of Medicine’s To Err Is Human (1999), concerns about patient safety have taken a prominent place in debates about American healthcare. The Institute published a second volume, Crossing the Quality Chasm (2001), asserting that patient care should be safe and that errors resulted not only from provider carelessness and unique circumstances, but also from flawed processes and systems; the JCAHO implemented a set of National Patient Safety Goals; and the Leapfrog Group put pressure on hospitals to disclose the extent to which they are following safety guidelines.
Stories of medical errors capture readers’ attention; the news media are attracted to stories that feature a mistake. Twenty years ago it was the Libby Zion case (Robins, 1995). Later high-profile cases include those of Betsy Lehman in 1994 (Conway & Weingart, 2005), Vincent Gargano in 1995 (Fegelman, 1995), Ben Kolb in 1996 (Belkin, 1997), and Jesica Santillan in 2003 (Cohen & Falco, 2003). The late medical writer Lynn Payer (1992) gave some insight into the news media’s contribution to public distrust of medical institutions. She cited journalistic imperatives that press toward simplified, black-and-white accounts, such as the tendency of editors to favor stories that pit good against evil, with little patience for more fully nuanced descriptions. This approach to reporting medical errors magnifies the most dramatic cases and promulgates an image of hospitals as dangerous places.
As a result, polls show that many Americans are sensitized to medical mistakes and perceive the healthcare environment as only “moderately” safe — safer than nuclear power or food handling, but less safe than airline travel or the workplace (National Patient Safety Foundation, 1997).
Consequently, patients, exposed to media accounts of medical errors that occur in hospitals, may begin a hospital visit wary and worried: Will something adverse, even disastrous, happen to me? (Burroughs et al., 2005; Rein, 2004). Hospital personnel may need to counter initial negative feelings of discomfort or lack of safety to increase patient comfort levels while hospitalized. Hospitals must make actual care safer, and personnel must communicate to patients what is being done to assure their safety.
Over the past few years, the patient safety movement has prodded hospitals to improve the safety of their practices. Hospital efforts are ongoing, and there is much more progress to be achieved. Surprisingly, to date, the role of the consumers of care — patients — in the patient safety movement has been minimal (Hatlie, 2004). Yet, it is patients who have the most to gain from increased safety in hospitals. Safety improvements protect patients physically; alleviating anxiety about safety during the hospital stay protects them emotionally.
One way in which the role of patients can be incorporated into the patient safety movement is through the examination of patients’ own perceptions of their personal safety while hospitalized. Patient perceptions can be used to pinpoint the kinds of persons, places, and processes to consider when assessing current practices and designing patient safety initiatives, and they can serve as a sort of reality check for individual hospitals interested in improving their culture of safety.
We will examine the following issues: How do patients perceive the safety and security of an inpatient hospital milieu? Do such perceptions vary in predictable ways? What can be done to increase the degree to which patients believe that their hospital visit will be safe and secure?
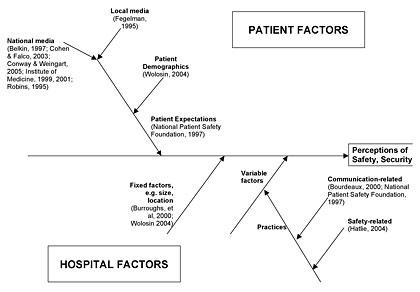
Theoretically, patients’ perceptions of safety and security while hospitalized are an outcome of the interaction of patient-related factors and hospital-related factors. On the patient side, media accounts and patient demographics affect patient expectations; on the hospital side, there are predetermined factors (size, location, etc.) as well as factors within the hospital’s control (e.g., safety practices and communication practices) (Wolosin, 2004). See Figure 1.
Press Ganey Associates, Inc., a patient satisfaction measurement and consulting firm, collects, reports, and warehouses patient satisfaction data on behalf of its clients. In the case of client hospitals, standard, psychometrically valid surveys are sent to patients upon discharge from the hospital; the surveys are returned directly to the company for processing and reporting. Response rates average 25%. In the survey, 49 distinct aspects of the visit (e.g., “Quality of the food”) are rated on a balanced, 5-point Likert-type scale. The scale ranges from 1 (very poor) to 5 (very good). Raw scores are converted to a 100-point scale for reporting purposes. In addition, several background questions (e.g., age, sex) appear on the survey.
In 2004, more than 650 client hospitals used a question regarding perceived safety, in addition to the standard 49 items. Patients were asked to rate “Degree of safety/security felt in hospital.” Surveys with that question that were returned in 2004 from a hospital whose Medicare provider number could be ascertained and, with patient age and sex information, were used as the basis of this report. These conditions yielded a set of over 600,000 surveys from 495 hospitals. The age-sex distribution of survey respondents approximated the latest available national hospital discharge statistics (Hall & Owings, 2002).
Patient Ratings of Safety
Over the entire sample, the average rating for the safety/security question was 87.8, roughly midway between “good” and “very good.” Overall, patients say they felt relatively safe in the hospital.
Demographics
There were notable variations in safety ratings. For one thing, female patients aged 18-34 (most of whom were in the hospital giving birth) felt safer than any other group; interestingly, male patients of the same ages felt the least safe of any group. This finding is probably due, in part, to the tendency of males to have longer hospital stays (on average, close to 5 days) than females (on average, just under 3.5 days). As noted below, perceptions of safety decline as the hospital stay lengthens.
Hospital Size
Hospitals varied from 70 to 100 in the average safety rating given by their patients. Larger hospitals tended to have lower average safety ratings than smaller ones. Large hospitals may seem to be more impersonal and may be exposed to more criticism from local media; thus, it is not surprising that their patient safety ratings are slightly lower than those of smaller facilities.
Type of Experience
On average, patients felt less safe as the length of their hospitalization increased. Moreover, patients who shared rooms rated their stay as less safe/secure than patients in private rooms. Interestingly, when patients were given more information about the potentially sensitive subjects of organ donation, patients’ rights, and life support during the registration process, they rated their stay as safer.
Improvement Strategies
The findings lead directly to practices that would increase perceived safety: shorter lengths of stay and more single-bed rooms. In addition, the more that information is shared — not just during registration, but throughout the patient’s stay — so as to give patients the sense that nothing important will be hidden, the greater will be the patient’s sense of safety and security. Having adequate information about the entire hospital visit has positive effects on feelings of safety and security (Boudreaux, Ary, Mandy, & McCabe, 2000; Louis Harris & Associates, 1997).
Such informational needs are not met routinely. A recent survey found that 41% of people with direct hospital experience reported not receiving answers to their questions about the illness. One-third reported not receiving adequate information about care prior to being released from the hospital. Seventeen percent reported that nurses sometimes, rarely, or never answered questions about the illness, and only 18% reported that nurses provided adequate information about care upon release from the hospital (Kaiser Family Foundation, 2000).
Conclusion
Studies have demonstrated a strong link between safety concerns and patient satisfaction, indicating that hospital personnel should
- counter negative initial impressions, where they exist;
- use available research including the findings of this study to improve patients’ perceptions of safety and security;
- improve their safety practices;
- communicate to patients and families what is being done for safety’s sake; and
- communicate more thoroughly and effectively throughout the patient’s visit (see sidebar).
Robert Wolosin (rwolosin@pressganey.com) is a research product manager in the Research and Development Department of Press Ganey Associates, Inc. Prior to Press Ganey, he worked in a family practice residency as director of Behavioral Science, and he has taught at Indiana University and Notre Dame. Wolosin was educated at the University of Chicago and the University of Michigan and has presented at conferences including The American Society for Healthcare Human Resource Administration, the International Society for Quality in Health Care, and the European Association for Healthcare Education.
Laura Vercleris a knowledge associate in the Knowledge Management Department of Press Ganey. She organizes literature and actively conducts quantitative and qualitative research to highlight best practices in patient, physician, and employee satisfaction. Vercler received her bachelor’s degree from Illinois State University and her master’s degree from Purdue University. She recently earned her CPHQ and is active in a number of organizations including the National Association for Healthcare Quality and the American Society for Quality.
Jessica Matthews is a research assistant in the Research and Development Department of Press Ganey, where she conducts custom analyses and creates special documents for clients. Matthews received her bachelor’s degree in mathematics from Saint Mary’s College in Notre Dame, Indiana. She has presented at the American Academy of Allergy, Asthma, and Immunology.
- Sidebar:

- • Communicating With Patients
References
Belkin, L. (1997, June 15). How can we save the next victim? The New York Times Magazine,33-70.
Boudreaux, E. D., Ary, R. D., Mandy, C. V., & McCabe, B. (2000). Determinants of patient satisfaction in a large, municipal ED: the role of demographic variables, visit characteristics, and patient perceptions. American Journal of Emergency Medicine,18(4), 394-400.
Burroughs, T. E., Waterman, A. D., Gallagher, T. H., Waterman, B., Adams, D., Jeffe, D., et al. (2005). Patient concerns about medical errors in emergency departments. Academic Emergency Medicine,12(1), 57-64.
Clark, C. R. (1997). Creating information messages for reducing patient stress during health care procedures. Patient Education and Counseling,30, 247-255.
Cohen, E., & Falco, M. (2003, February 23, 2003). Victim of botched transplant declared dead. Retrieved June 13, 2005, from http://www.cnn.com/2003/HEALTH/02/22/transplant.error
Conway, J. B., & Weingart, S. N. (2005). Organizational change in the face of highly public errors: I. The Dana-Farber Cancer Institute experience. Retrieved June 16, 2005, from http://webmm.ahrq.gov/perspectives.aspx
Fegelman, A. (1995, June 15). U. of C. cancer patient dies of chemotherapy overdose. Chicago Tribune,p. 2.
Gallagher, T. H., Waterman, A. D., Ebers, A. G., Fraser, V. J., & Levinson, W. (2003). Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA,289(8), 1001-1007.
Hall, M. J., & Owings, M. F. (2002). 2000 National Hospital Discharge Survey. Retrieved April 22, 2005, from http://www.cdc.gov/nchs/data/ad/ad329.pdf
Hatlie, M. J. (2004). Consumers and the patient safety movement: Past and future, here and there. Patient Safety and Quality Healthcare,6-10.
Institute of Medicine. (1999). To err is human: Building a safer health system.Washington, D.C.: National Academies Press.
Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century.Washington, D.C.: National Academy Press.
Kaiser Family Foundation. (2000). National survey on Americans as healthcare consumers: An update on the role of quality information.Rockville, MD: Agency for Healthcare Research and Quality.
Liang, B. A. (2002). A system of medical error disclosure. Quality & Safety in Health Care,11(1), 64-68.
Louis Harris & Associates. (1997). Public opinion of patient safety issues:Research findings: National Patient Safety Foundation at the AMA.
Maicki, H. W. (2001). Communicating bad news. Supportive Voice(Winter).
National Patient Safety Foundation. (1997). Nationwide poll on patient safety: 100 million Americans see medical mistakes directly touching them. Retrieved May 6, 2005, from http://www.npsf.org/html/pressrel/finalgen.htm
Payer, L. (1992). Disease-mongers: How doctors, drug companies, and insurers are making you feel sick.New York: John Wiley & Sons.
Rein, A. (2004). Consumer perspectives: The effect of current nurse staffing levels on patient care.Washington, D.C.: National Consumers League.
Robins, N. (1995). The girl who died twice: Every patient’s nightmare: The Libby Zion case and the hidden hazards of hospitals.New York, NY: Delacorte Press.
Tito, F. (2000, Winter). Communicating with patients about risk and safety.National Patient Safety Foundation’s Focus on Patient Safety, 3, 6,8.
Wolosin, R. J. (2004). Patients’ perceptions of safety in U.S. hospitals, AcademyHealth 2004 Annual Research Meeting.San Diego, CA.
