Patient Identification: Producing a Better Barcoded Wristband
May / June 2008
![]()
Patient Identification: Producing a Better Barcoded Wristband
![]()
Patient identification is the cornerstone of patient safety. In fact, virtually all patient safety initiatives call for patient identification as a critical step in a larger workflow, such as verifying the “five rights” of medication administration or matching the correct blood product with the right patient prior to a transfusion. Despite its fundamental nature, however, no standard exists for ensuring positive patient identification at hospitals nationwide.
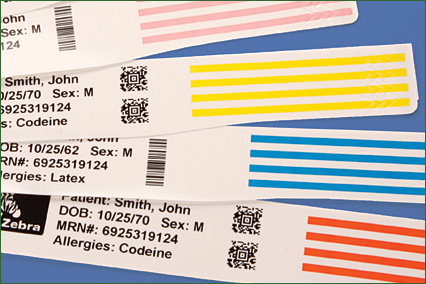
The use of barcode technology for patient identification is a growing trend at many healthcare organizations. It offers a convenient, efficient way to ensure patient information is available at the point of care and also supports compliance with the Joint Commission guidelines. In 2008, “improving the accuracy of patient identification” tops the Joint Commission’s National Patient Safety Goals. The goal requires the use of two or more patient identifiers when administering medications and blood products or taking blood samples; a barcoded wristband that includes two or more patient specific identifiers complies with this requirement.
With barcoding, as any technology implementation, the key to success lies in helping nurses and clinicians confirm patient identification with the greatest possible ease and reliability. In terms of impact on medication error rates or other patient safety goals, these two factors are closely intertwined with the need for accuracy.
Healthcare providers pursue initiatives based on patient identification for safety and error prevention. Whether the application is medication administration, specimen collection, or blood administration, a facility’s approach to patient identification can both support objectives and streamline workflow for clinicians.
One Hospital’s Experience
As a health system based in Bennington, Vermont, Southwestern Vermont Health Care (SVHC) serves southern Vermont and parts of New York and Massachusetts. In addition to its 99-bed flagship facility, SVHC offers rehabilitation, long-term care, hospice and home care, advanced cancer treatment, and primary care services. An early adopter of healthcare IT, SVHC implemented its core hospital information system in 1991. More recently, in late 2007 and early 2008, SVHC introduced barcoding for bedside medication verification. As a part of that initiative, we gave careful consideration to our patient identification methodology.
SVHC received funding support for this project through the Agency for Healthcare Research and Quality (AHRQ) with an implementation grant designed to demonstrate improvements in patient safety through information technology. Our specific project aims to decrease medication transcription and administration errors through the use of barcoding and eMAR technologies.
We evaluated both barcoding and radio-frequency identification (RFID) as possible options, but we ultimately determined that RFID was still too new and costly for a hospital such as ours. With this decision behind us, we moved on to exploring barcode symbologies and print options in light of the needs of our patients, clinicians, and the hospital’s mission.
Creating a Lasting Image
Before implementing our bedside medication verification solution, we had been using laser printers to produce our barcoded patient identification wristbands. The laser-generated labels were not only difficult to separate from the backing sheets, but the resulting bands were also easily damaged and fell apart quickly.
To overcome these challenges, we implemented direct thermal wristband printers. Thermal printers are designed specifically for barcoding and produce lasting, durable barcodes that can be easily scanned at the point of care. In fact, our current bands survive a week of wear, 24 hours under water, or temperatures up to 130 degrees Fahrenheit. In addition, thermal printers allow users to create only the wristbands they need while laser printers must print full or half sheets of wristbands or labels. The laser method wastes costly wristbands and labels that must be thrown away or destroyed by staff for HIPAA compliance.
When compared to laser printers, there is not a significant cost difference between laser and thermal printers, and thermal printers may even save money because direct thermal printers do not use ink, toner, or ribbons. They are also very easy for nurses to load and require little maintenance, making them ideal for networked use anywhere in the organization. In addition to implementing wristband printers in the patient admissions area, we placed five printers on the floors so that nurses can also produce replacement bands when needed.
Another point of interest is the relative ease of printing two-dimensional (2-D) codes. It is not more difficult than generating linear codes because the intelligence for creating the 2-D images resides in the printer, not the application software.
Selecting the Right Symbology
When evaluating barcode symbologies, our first step was to determine a preference for either linear or 2-D barcodes. Linear barcode formats, such as Code 128, encode data by simply alternating black and white spaces in one direction. The actual data is represented by the white spaces between the lines. Laser scanners, the most common type of decoding device, read the code by illuminating the printed media and measuring the reflected light.
Two-dimensional barcodes are more complex. These code formats usually consist of a matrix or grid pattern, with height and width, that encodes characters in two directions. Aztec Code and Data Matrix are examples. Two-dimensional symbologies are more advanced in the sense that they can encode much more data in a much smaller space, are readable at any orientation, and offer error correction.
For three primary reasons, we chose the 2-D Data Matrix format for both bedside medication verification and medication labeling in the pharmacy:
• Ease of use while scanning. Any difficulties encountered when scanning a barcode may lead to workarounds, which can jeopardize the overall safety of the patient. The orientation of the barcode on the wristband can also hinder ease of scanning and result in workarounds. Due to the length of many linear symbologies, the curvature of the patient’s wristband actually distorts the spacing of the barcode and makes it difficult to scan, particularly for pediatric or infant patients. Difficulty may arise when linear codes are printed perpendicularly to the length of the wristband because the required reduction in size of the symbol presents scanning challenges.
In organizations that still use linear codes, it is not uncommon for nurses to insert a finger underneath the wristband to straighten it out and get a successful scan of the symbol. Of course, that takes time. It also increases the potential for infection.
With smaller, 2-D symbols that can be read from any direction, getting a successful scan typically requires less effort. These barcodes can be repeated around the length of the wristband. At SVHC, we repeat the Data Matrix code 15 times. In many cases, there is no need to disturb a sleeping patient to get a positive scan. For example, if a nurse is administering an IV drug late at night, he or she can scan any spot on the wristband, from any angle, and get a positive patient identification.
• Reading accuracy and data capacity. Two-dimensional barcodes offer much greater accuracy than traditional, linear barcodes. While “best case” error rates are one per 37 million with Code 128, the error correction built into formats such as Data Matrix and PDF417 create symbols that fail only once per 612 million scans.
Of course, the differences in these hypothetical error rates are probably undetectable during everyday use. These numbers also reflect optimum scanning conditions, which are rarely present in hospitals. The advantage does come into play when wristbands are somehow wrinkled or deformed. Even when partially damaged, Data Matrix codes can often still be read.
Perhaps more importantly for forward-looking organizations, 2-D formats can encode or represent more information in a smaller space. Beyond simply representing a simple sequence of numbers, say a patient account number, 2-D codes can carry thousands of alphanumeric characters.
Even in the space of three square millimeters, Data Matrix can encode about 50 alphanumeric characters. That is roughly the number of characters in this paragraph. For this reason, our future barcodes may include patients’ names, blood type, date of birth, or other details.
• Equipment requirements. The main advantage of Code 128 and other linear symbologies arises from the fact they have been around for decades. Virtually any barcode scanner will read Code 128, UPC, and Code 39. Older, laser-based readers were designed before 2-D symbols were developed, so they are not compatible. To reap the benefits of 2-D, hospitals must invest in newer scanners with CCD sensors. Fortunately for health systems such as SVHC, reliable scanners are available for several hundred dollars rather than several thousand dollars.
On the topic of compatibility, we should add that we do use both linear and 2-D codes on our wristbands. Unfortunately, our legacy blood glucose monitoring system requires the linear format, which we print perpendicular to the length of the band without complication. As technology progresses and our budget for new equipment allows, SVHC will inevitably move away from linear barcodes and expand the types of data we encode.
Results
As of February 2008, bedside medication verification was live in the ICU and in both the east and west wings of SVHC. In the first two weeks of February, we administered 10,000 medications with a 93% scan rate. That figure is a conservative estimate; factoring in patient transfers to units not yet live with bedside medication scanning, the actual rate is higher.
The system is certainly preventing errors. Our clinical staff must now systematically verify the five rights — right patient, drug, dose, route, and time. But with a slightly more advanced symbology and a nearly indestructible barcode image, we are improving caregivers’ chances of doing the job right and enhancing patient outcomes.
In the near future, we’ll move on to implement barcode-based systems for specimen collection and blood transfusion management. The lessons learned here will also apply for applications down the road. As our experience illustrates, the choices an organization makes about its approach to patient identification directly impact productivity, the risk of workarounds, and medical error rates plus provide a strong foundation upon which additional safety applications can be introduced.
Edward Lanoue is an informatics pharmacist at SVHC. He has developed, implemented, and upgraded information systems and automation technology since 1996. He may be contacted at etl@phin.org.
Charles Still is senior systems analyst at SVHC. Previously, he was director of information systems at Albany Medical Center and systems manager for an automotive manufacturing company. He writes frequently about barcode systems and Web-based workflow automation. He may be contacted at stich@phin.org.
