Pain Relief vs. Addiction and Overdose: Four Steps to Maintain an Appropriate Equilibrium
By Justina Igwe
Opioids have been one of the world’s most effective pain relievers since Friedrich Sertürner of Germany extracted an opioid analgesic from opium in 1803. Extracted from the opium poppy (Papaver somniferum), a species of flowering plant originating in Asia Minor but now grown in all temperate regions of the world, opioids are widely used in healthcare facilities to relieve both acute and chronic pain.
However, as we well know, opioids have become a substance of concern due to their propensity to spark misuse and addiction. Tragically, the Centers for Disease Control and Prevention (CDC) estimates that there have been about 1 million drug overdose deaths since 1999, of which 82.3% involved a synthetic opioid.
As expected, it is a major public health challenge to balance the need for pain relief and the imperative of reducing opioid addiction and overdose deaths. Below are four steps that healthcare systems can take to achieve that balance.
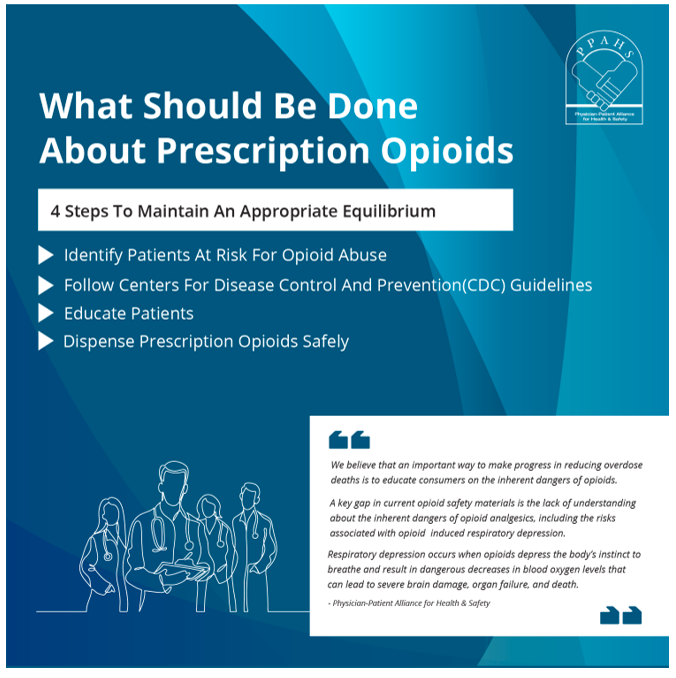
Step 1: Identify patients at risk for opioid misuse
Clinicians must be cautious when taking care of patients who fall under this category, including:
- Patients recently released from prison. It is estimated that 85% of people in prison have an active substance use disorder or were incarcerated for a crime involving drugs or drug use. Prison inmates with an opioid use disorder may experience lowered opioid tolerance, putting them at greater risk for overdose upon release from prison if clinicians do not provide appropriate treatment.
- Patients who obtain prescription opioids from multiple pharmacies. Research has shown that patients who obtain drugs from multiple pharmacies, whether concurrently or sequentially, have a higher chance of non-adherence.
- Patients who obtain prescription opioids alongside other medications. Patients who don’t receive adequate education on opioids’ euphoric properties may be more likely to misuse them even while adhering to treatment regimens of other prescribed medications.
Providing counseling and conducting urine drug testing (UDT) should come before administering opioids. Patient safety should be the top priority of every opioid prescriber.
Step 2: Follow CDC guidelines
To ensure patients’ safety, clinicians should administer opioids only in accordance with CDC guidelines. The goal of these guidelines, according to Lynn R. Webster, MD, FACPM, FASAM, is “to reduce the number of overdose deaths.” These guidelines have three main focus areas:
- Preferred treatment for chronic pain. Treatment should begin with non-pharmacological approaches such as physical therapy, psychotherapy, and relaxation therapy. If pharmacological therapy is indicated, try non-opioid options such as NSAIDs. Finally, establish realistic treatment goals with the patient if an opioid prescription is necessary—that is, if the benefits outweigh the risks.
- Opioid selection, dosage, duration, follow-up, and discontinuation. The decision to use short-acting or long-acting opioids should depend on the individual patient. However, the CDC advises beginning with short-acting opioids because they are associated with fewer adverse effects. Begin with the lowest effective dosage and only increase it after reassessing the patient’s need. The CDC notes that most patients need not remain on opioids for long; for many, three days is enough, and it should be rare for a patient to stay on opioids for more than seven days. Discontinue opioids gradually when it is obvious that their risk outweighs their benefits.
- Assessing risks and addressing the harm of opioid use. Avoid prescribing opioids and benzodiazepines concurrently; they have synergistic effects and can cause oversedation and respiratory depression, heightening the risk of overdose or death. Conduct UDT to rule out patients’ use of controlled substances and illicit drugs. (Read the CDC guideline for UDT by clicking here.) Finally, provide counseling before discharging patients. Enlighten them on why they should never use opioids without a doctor’s prescription and on the adverse effects that result from misuse. Warn them about how opioids can induce respiratory depression and how to address it. Make use of the CDC checklist to ensure that nothing is left out.
Step 3: Educate patients
In 2012, The Joint Commission issued Sentinel Event Alert #49, “Safe use of opioids in hospitals.” This alert stated:
While opioid use is generally safe for most patients, opioid analgesics may be associated with adverse effects, the most serious effect being respiratory depression, which is generally preceded by sedation.
In a recent letter to the FDA, several physician societies call for greater educational efforts on opioid safety:
We believe that an important way to make progress in reducing overdose deaths is to educate consumers on the inherent dangers of opioids. A key gap in current opioid safety materials is the lack of understanding about the inherent dangers of opioid analgesics, including the risks associated with opioid-induced respiratory depression. Respiratory depression occurs when opioids depress the body’s natural instinct to breathe, and results in dangerous decreases in blood oxygen levels that can lead to severe brain damage, organ failure and death.
Step 4: Dispense prescription opioids safely
When opioids are indicated, here are some key points to keep in mind:
- Take the time to speak with patients about their prescription. This allows for proper counseling on the prevention of opioid misuse.
- Refuse to dispense prescription opioids directly to patients.
- Evaluate prescription orders for forgery and alteration.
- Evaluate new prescription orders with concurrent treatments.
- Determine whether medication has been mistakenly or improperly prescribed.
- Validate a prescriber’s Drug Enforcement Administration registration and patient identification.
- Check the prescription drug monitoring program as well as patients’ records. Consult the prescriber for any concerns.
Justina Igwe is a nursing student at the University of Nigeria Enugu Campus.
