Optimization of Peripherally Inserted Central Catheter Placement Practices
By Kenneth Murphy, MD, FSIR; Kimberly G. Alsbrooks, BSN, RN, RT (R), VA-BC; Kathy Kokotis, RN, BS, MBA; and Kaitlin Carr Heath, MBA
Introduction
Peripherally inserted central catheters (PICC) have been lifelines for countless patients in need of intravenous therapies since their popularization in the 1970s as an alternative to non-tunneled central venous catheters (Hoshal, 1975; Sandrucci & Mussa, 2014). With more than 4 million PICCs placed annually, PICC insertion is one of the most frequently performed procedures in the United States (Girgenti & Moureau, 2013). Antibiotic administration is the most common reason for PICC placement, but indications are wide ranging and include power injection of contrast media, blood draws, delivery of diverse medications (e.g., chemotherapy), and administration of fluids, blood products, and total parenteral nutrition (Cotogni & Pittiruti, 2014).
As PICC placement practices have evolved over time, it has been important to ensure that the procedure is performed safely and efficiently. A variety of healthcare entities, including medical researchers and medical device manufacturers, have developed training curricula for placers—i.e., personnel who place PICC lines—and protocols to standardize each procedure (Chopra et al., 2015). The use of advanced vascular access (VA) technologies such as point-of-care ultrasound guidance (USG) has also flourished in pursuit of this end. In light of the importance of safe and efficient PICC placement, ensuring that hospitals are able to invest in these resources should be a fundamental mission for the larger healthcare community.
Amid a changing PICC clinical and reimbursement landscape, there is a need to identify best practices for PICC placement that promote widely held patient safety goals, clinical efficiency, and hospital financial health. Even small changes in clinical and/or reimbursement practices can have a significant impact given the high-volume nature of PICC procedures. Through literature review and interviews with key clinical and nonclinical stakeholders, this report seeks to illuminate features of the current PICC landscape with an eye toward determining the best practices for preserving a safe and high-functioning clinical system.
A changing landscape: Variability of clinical practice
In its early clinical history, most PICC placement was performed at the bedside by nurses using moderately successful landmark techniques. Introduction of catheter tip visualization technologies, such as fluoroscopy, moved PICC procedures into the hands of interventional radiologists (IR) trained in the use of these procedures. However, it was not long before advancements in VA technologies, such as the modified Seldinger technique (MST), MST with point-of-care USG, and novel tip location/confirmation systems, made bedside insertion safer, more successful, and more accessible to diverse providers (Sandrucci & Mussa, 2014). These developments along with new VA training programs, favorable cost/clinical outcomes analysis, and a more accepting hospital culture eventually shifted the majority of PICC placement back to the bedside and to registered nurses (RN) with specialized VA training. The manpower available for PICC placement also increased exponentially as PICC-specific training programs, geared toward nonphysician providers, expanded the pool of placers and provided mastery of skills needed for bedside insertion and troubleshooting. Per recent Medicare legislation, nonphysician providers, including RNs, certified registered nurse anesthetists, nurse practitioners, physician assistants, radiology assistants (RA), and radiology technologists, may now have supervised or unsupervised PICC insertion within their scope of practice, depending on state regulations or hospital protocols (Medicare Access to Radiology Care Act of 2019, 2019–2020).
Placement at the bedside, as opposed to in the IR suite, also holds several advantages that have maintained and strengthened this historic shift while supporting the adoption of bedside placement as best practice. These advantages can be easily conceptualized as the “3 R’s”: Resource management, Risk reduction, and Radiation avoidance (Figure 1).
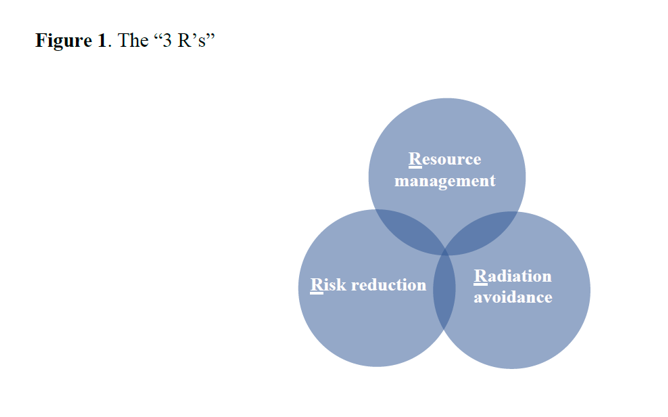
With respect to resource management, bedside PICC placement requires a considerably smaller amount of material resources, personnel, and time for supportive activities (e.g., intra-hospital transport [IHT], waiting for a room). Observational studies measuring average patient transport time to the IR suite, procedural time, and room cleanup time have revealed a 1.5-hour process at minimum (Agrawal et al., 2014; Tomaszewski et al., 2017; Toomay et al., n.d.; Walker & Todd, 2013). An additional hour can be added to the process for lengthy transports and procedures, or patients under isolation precautions due to the need for suite sterilization (Ierardi et al., 2020; Tomaszewski et al., 2017). Bedside placement, by comparison, requires approximately 45 minutes (Tomaszewski et al., 2017).
PICC placement at the bedside also allows for avoidance of the high-cost resources associated with IR suite procedures, including fluoroscopy, patient transporters, room staff, charges for room use, and clinical assistants for the placer. Indeed, the estimated cost for a patient undergoing PICC placement in the IR suite is $1,469.32, compared to $386.33 for bedside placement (Meyer, 2010). Thus, hospitals can observe significant cost savings by providing bedside PICC placement whenever clinically appropriate.
Bedside PICC placement is also advantageous with respect to risk reduction as IHT may carry health risks for patients, mobilized clinical staff, and nonclinical personnel. Critically ill patients, for example, may clinically decompensate or incur harm from equipment malfunction en route to the IR suite (Fanara et al., 2010). For critical and non-acute patients, IHT can result in interrupted oxygen therapy, missed respiratory treatments and blood draws, paused infusions of essential intravenous therapies, and possibly missed evaluations by their rounding healthcare team (Despoina & Brokalaki, 2014). Unnecessary IHT may also place the larger hospital community at an exposure risk when a transported patient is infectious, which is an unfortunate but critical consideration, especially during the COVID-19 era (Pittiruti & Pinelli, 2020).
Lastly, bedside PICC placement with tip location/confirmation technology allows for radiation avoidance by reducing potential exposure of patients, providers, and hospital staff. According to the Organization for Occupational Radiation Safety in Interventional Fluoroscopy (2015), image-guided medical procedures using interventional fluoroscopy are the leading source of occupational ionizing radiation exposure for medical personnel. Patients undergoing a procedure with fluoroscopic guidance are exposed to as much as 250 to 3,500 times more radiation than a single chest x-ray (U.S. Food and Drug Administration, 2010).
Any effort to describe the advantages of bedside PICC placement and support its use as best practice must, however, be coupled with acknowledgment of the IR suite’s criticality to a successful PICC program. The unique capabilities of interventional radiologists and resources of the IR suite are essential for the appropriate care of certain patients, such as those with difficult venous access. The objective of clinical decision-making should be to choose the most appropriate setting and placer based on the unique therapeutic needs of the patient.
A changing landscape: Reimbursement
Review of medical insurance coding and policies in the United States reveals a complex reimbursement system with payments to healthcare facilities and professionals dependent on multiple variables, including patient insurance type (e.g., Medicare, Medicaid, or commercial), hospital admission status (e.g., inpatient or outpatient), and procedural setting (e.g., inpatient bedside, outpatient examination room, or IR suite). A thorough review of any of these variables is beyond the scope of this discussion. But for our purpose, it suffices to note that new trends in coding and value-based payment have altered the reimbursement landscape.
PICC-related reimbursement rates have been declining, with unfavorable changes in both provider (professional fee) and institutional (facility fee) components. In 2019, the Medicare Physician Fee Schedule bundled PICC insertion, imaging guidance, and radiologic interpretation into a single CPT® code, which led to 25% and 36% reductions in the professional fee for PICC placement and replacement, respectively, in the hospital setting (Centers for Medicare & Medicaid Services, 2021; Coffta, 2019). Facility fees for inpatient procedures have also declined as increases in “payment bundling” by insurance providers have pushed healthcare facilities to provide essentially discounted treatment packages (Scamperle, 2013). As these trends intensify, there is a growing need to identify best practices for PICC placement that optimize patient care while supporting clinical efficiency and institutional financial health.
Semi-structured interviews
A targeted review of the literature demonstrated a variable PICC clinical landscape coupled with complex reimbursement practices. To gain a deeper understanding from multiple perspectives, we conducted semi-structured in-depth interviews, using primarily open-ended questions, with a variety of clinical and nonclinical stakeholders. Questions were based on topics in the literature that could benefit from further research and firsthand provider insight, such as institutional PICC practices, their pros and cons, and ways to optimize practices from clinical and reimbursement standpoints. Interviewees were screened for participation based on their self-reported knowledge of clinical and/or reimbursement practices regarding PICC placement.
Two IR physicians, two RNs, and two respondents with a background in hospital billing/coding, collectively representing the Northeast and Western regions of the United States, were ultimately selected for semi-structured interviews based on their self-reported knowledge/experience. Interviewees worked at an assortment of public, private, academic, and non-academic hospitals ranging in size from an acute care hospital of fewer than 200 beds to a nearly 500-bed hospital within a large tertiary health care network. All respondents reported involvement in the care or reimbursement of inpatients and outpatients, and their hospitals’ acceptance of Medicare, Medicaid, and most (not necessarily all) types of commercial insurance.
Findings
Providers & patients
Interviewees’ descriptions of PICC clinical practices at their institutions were consistent with each other and the literature. In brief, respondents noted that PICC lines are typically placed at bedside by a specially trained nurse under a physician’s order but with no requirement for direct physician supervision. USG and electrocardiography (ECG)-based catheter tip location/confirmation systems are used for PICC insertion and tip location verification, respectively; chest x-ray verification is occasionally used for a nonconfirmatory ECG. Patients with historical or presumed difficult vascular access may be scheduled for PICC placement with an IR physician in the IR suite, where fluoroscopy and support staff are available. Despite literature on the diversity of providers with PICC placement in their scope of practice, RAs or radiology technologists were rarely involved in PICC procedures at interviewees’ institutions due to regulations or hospital protocols.
While acknowledging IR’s criticality for challenging cases and benefits of the IR suite, all respondents strongly recommended bedside PICC placement by specially trained nurses for the majority of patients with uncomplicated vascular access. As a first point, all emphasized that a nurse with appropriate PICC training is just as capable as an IR physician of performing the procedure.
As one RN remarked, “There is no reason for a physician to do it. It’s a skill that a nurse with proper training can do, just as a physician would need proper training.”
“Any nurse can be trained to place a PICC,” echoed an IR physician. These views are supported by the literature, with a U.S. single-center study showing a jump from a 69% PICC placement success rate for specially trained nurses using landmark technique at the bedside, to a greater than 90% success rate when these nurses were provided with advanced VA technologies (Croteau et al., 2009). A similar U.S. single-center study, performed after the implementation of a nursing PICC team equipped with USG and micro-introducers, demonstrated a greater than 90% PICC placement success rate at the bedside as compared to an approximately 40% success rate the previous year for specially trained nurses working without these technologies (Hawes, 2007). Success rates for these specialized nursing teams can even approach those of physicians in the IR suite, with one single-center cohort analysis demonstrating a 93.1% insertion success rate for PICC-trained nurses at the bedside as compared to the 100% success for IR/anesthesiology in the IR suite (Walker & Todd, 2013). While respondents did note the benefit of easier PICC troubleshooting in the IR suite, they nevertheless emphasized that proper training of placing providers and increased availability of advanced VA technologies (i.e., point-of-care USG) could obviate most issues at the bedside.
In further support of bedside placement, interviewees did not observe any difference in central line–associated infections or other complications based on placing provider or clinical setting, another view supported by the existing literature. Examination of the nursing PICC team at one institution revealed relatively low rates for multiple complications compared to previously published rates (Bouzad et al., 2016; Chopra et al., 2013; Maki et al., 2006), including catheter-related bloodstream infections (0.6%), catheter-related deep venous thrombosis (1.5%), and requirement of at least one thrombolytic dose for catheter management (11.4%) (McDiarmid et al., 2017). A more recent multicenter retrospective study demonstrated minimal complication rates for catheter-related bloodstream infection (0.6%; 0.37 per 1,000 catheter days) and catheter-related deep venous thrombosis (0.8%; 0.46 per 1,000 catheter days) after each institution implemented a nurse-led PICC service (Ruegg et al., 2020). All interviewees emphasized that appropriate training of placers and adherence to procedural protocols could equate infection risk among clinical settings.
Respondents also highlighted another crucial reason for moving to the bedside: patient satisfaction. In their familiar hospital bed, with the potential for family or friends nearby, patients can have a more comfortable procedural environment conducive to well-being. Survey results from one U.K.-based single-center study of patients undergoing PICC placement found that satisfaction was considerably higher among those who had a member of the PICC nursing team explain the procedure at the bedside instead of a physician in the IR suite (Walker & Todd, 2013). Another U.S.-based study found that patients’ perception of the skill and courtesy of nurses starting their IVs increased by 14% and 7%, respectively, after the hospital’s institution of a nursing PICC team (Hawes, 2007). Simply put, patients’ apparent preference is to stay put and engage with the nurses whose familiar faces fill their day.
Reimbursement and costs
All participants emphasized that procedural cost—while not something that affected their clinical decision-making—was a strong reason for supporting bedside PICC placement, when clinically appropriate, given the importance of financially healthy healthcare institutions. Costs of time, materials, human resources, and room charges with use of the IR suite were noted most often. Current reimbursement rates, for example, do not account for the time occasionally required to transport a patient to the IR suite, prepare the room, assemble room staff, and ultimately prepare the suite for subsequent use. Nor do they account for the additional time required or challenge of PICC placement for a patient with complex vasculature. This time can also represent losses for the larger hospital community. As interviewees noted, use of the IR suite when not clinically necessary may lead to providers and specialized equipment being unavailable to other patients, and a need for increased staffing to prevent delayed or deficient care. Unnecessary utilization of the IR suite may also result in revenue loss for facilities whose IR physicians are working below the top of their licensure. A 2009 study from a U.S. hospital served as a remarkable testament to the time and opportunity costs associated with the use of the IR suite. After introducing a PICC nursing team under the IR service, departmental backlogs and waiting times for PICC placement were eliminated, allowing for reassignment of the IR suites to complex PICCs and higher-revenue procedures. The result was $1.2 million in cost savings for the hospital in the first half of the year alone (Croteau et al., 2009).
Another financial consideration noted by interviewees was the potential impact of reduced reimbursement facility fees on patient care. As mentioned earlier in our discussion, reimbursement of VA procedures has been impacted by Medicare and Medicaid programs’ increased use of “payment bundling” and categorization of these procedures as integral to many treatment regimes. This trend also affects commercial insurance reimbursement rates as most contracts are based on a percentage of fees established by the Centers for Medicare & Medicaid Services. Furthermore, commercial insurance companies have increasingly adopted de facto bundling practices by denying payment for procedures that may be considered integral to managing a patient’s condition. As facility fees for inpatient PICC reimbursement decline, so may facilities’ incentive to adopt more expensive novel or advanced VA technologies (e.g., smaller lumen catheters, all-inclusive PICC kits, point-of-care USG) and providers’ interest in performing the procedure. These changes could, in turn, result in delayed access to PICC placement, diminished patient satisfaction, and worse clinical outcomes.
Recommendations of the participants
While the clinical diversity of patients necessitates variety concerning PICC placers and settings, falling PICC reimbursement rates highlight the importance of selecting and using these resources efficiently. Indeed, increased procedural efficiency can help health facilities improve their financial health, clinical outcomes, and ultimately patient satisfaction. Respondents had several suggestions regarding best practices for improving the clinical efficiency of PICC placement and addressing cost-related concerns.
- Increased availability of PICC-trained nurses
Insufficient numbers and/or availability of PICC-trained nurses for full patient coverage can lead to unnecessary scheduling of PICC procedures in the IR suite. Creation of more PICC training and qualification programs, aggressive recruitment of PICC-trained nurses, and on-call staffing of these nurses to nontraditional hours could prevent much of this unnecessary (and costly) escalation of care.
- Utilization of advanced VA technologies at bedside
Increased availability of point-of-care USG and other VA technologies at the bedside, and more training programs for their operators, would promote procedural safety and efficiency and allow for more PICC placements to occur at the bedside by nurses.
- Increased reimbursement for PICC insertion attempts
Interviewees had two suggestions for addressing cost-related concerns due to current reimbursement practices. First, payers could provide additional reimbursement for placements ultimately completed in the IR suite, following unsuccessful insertion attempts at the bedside. This would deter immediate escalation of care to the IR suite and allow partial recouping of costs associated with bedside attempts. Second, payers could adjust reimbursement rates to compensate for the additional time and resources required for PICC placement in the IR suite for patients with complex vasculature.
Conclusion
While many variables are involved, optimizing PICC placement practices fundamentally rests on patients receiving treatment in the most appropriate clinical setting by well-trained healthcare providers. Our findings from semi-structured interviews combined with the published literature suggest that bedside PICC placement should be considered as the most appropriate setting for most patients. Current clinical and reimbursement practices regarding PICCs represent significant challenges; however, the solutions may be more straightforward than expected since clinical and financial incentives seem to align for stakeholders. Future studies comparing clinical and efficiency outcomes between various PICC placement practices (e.g., personnel, setting, technology) will be able to inform both policy and clinical decision-making.
Kenneth Murphy, MD, FSIR, is medical director of the Mohawk Valley Vascular Center and director of interventional radiology at Faxton-Saint Luke’s Hospital in Utica, New York, both of which belong to the Mohawk Valley Health System. Kimberly G. Alsbrooks, BSN, RN, RT (R), VA-BC, is senior director of clinical programs in medication delivery systems (vascular access devices) at BD, where she works on program research and evidence-based program development, development of vascular access products, and related scientific and marketing publications. Kathy Kokotis, RN, BS, MBA, is director of global clinical development at BD, where she assists in development of marketing and educational programs for international vascular access products. Kaitlin Carr Heath, MBA, is associate director of market access and payment policy for BD, where she develops and leads global market access strategies, enables reimbursement and policy activities, and supports market development for medication delivery solutions.
References
Agrawal, J. P., Gupta, S., Gilani, S., & Lev, S. (2014). Improving the PICC line workflow. Journal of Vascular and Interventional Radiology, 25(3), S61. https://doi.org/10.1016/j.jvir.2013.12.153
Bouzad, C., Duron, S., Bousquet, A., Arnaud, F.-X., Valbousquet, L., Weber-Donat, G., Teriitehau, C., Baccialone, J., & Potet, J. (2016). Peripherally inserted central catheter-related infections in a cohort of hospitalized adult patients. CardioVascular and Interventional Radiology, 39, 385–393. https://doi.org/10.1007/s00270-015-1182-4
Centers for Medicare & Medicaid Services. (2021, July 19). Physician Fee Schedule. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched
Chopra, V., Flanders, S. A., Saint, S., Woller, S. C., O’Grady, N. P., Safdar, N., Trerotola, S. O., Saran, R., Moureau, N., Wiseman, S., Pittiruti, M., Akl, E. A., Lee, A. Y., Courey, A., Swaminathan, L., LeDonne, J., Becker, C., Krein, S. L., & Bernstein, S. J. (2015). The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): Results from a multispecialty panel using the RAND/UCLA appropriateness method. Annals of Internal Medicine, 163(6 Suppl), S1–40. https://doi.org/10.7326/M15-0744
Chopra, V., O’Horo, J. C., Rogers, M., Maki, D. G., & Safdar, N. (2013). The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: A systematic review and meta-analysis. Infection Control & Hospital Epidemiology, 34(9), 908–918. https://doi.org/10.1086/671737
Coffta, S. (2019, April 16). The value of PICC lines for interventional radiologists. HAP Partners Radiology Billing and Coding Blog. https://info.hapusa.com/blog-0/the-value-of-picc-lines-for-interventional-radiologists
Cotogni, P., & Pittiruti, M. (2014). Focus on peripherally inserted central catheters in critically ill patients. World Journal of Critical Care Medicine, 3(4), 80–94. https://doi.org/10.5492/wjccm.v3.i4.80
Croteau, D. L., Coristine, P. M., Sturza, S. G., Hunt, C., Getzen, T. M., Clayton, W. J., Campbell, T. D., & Angus, B. A. (2009). Abstract No. 106: The implementation of an RN bedside PICC team under the interventional radiology umbrella – a patient flow process improvement. Journal of Vascular and Interventional Radiology, 20(2), S42. https://doi.org/10.1016/j.jvir.2008.12.087
Despoina, A. G., & Brokalaki, H. (2014). Intrahospital transport policies: The contribution of the nurse. Health Science Journal, 8(1), 166–178. https://www.hsj.gr/medicine/intrahospital-transport-policies-the-contribution-of-the-nurse.pdf
Fanara, B., Manzon, C., Barbot, O., Desmettre, T., & Capellier, G. (2010). Recommendations for the intra-hospital transport of critically ill patients. Critical Care, 14, R87. https://doi.org/10.1186/cc9018
Girgenti, C., & Moureau, N. L. (2013). The need for comparative data in vascular access: The rationale and design of the PICC registry. Journal of the Association for Vascular Access, 18(4), 219–224. https://doi.org/10.1016/j.java.2013.07.003
Hawes, M. L. (2007). A proactive approach to combating venous depletion in the hospital setting. Journal of Infusion Nursing, 30(1), 33–44. https://doi.org/10.1097/00129804-200701000-00006
Hoshal, V. L. (1975). Total intravenous nutrition with peripherally inserted silicone elastomer central venous catheters. Archives of Surgery, 110(5), 644–646. https://doi.org/10.1001/archsurg.1975.01360110190032
Ierardi, A. M., Wood, B. J., Gaudino, C., Angileri, S. A., Jones, E. C., Hausegger, K., & Carrafiello, G. (2020). How to handle a COVID-19 patient in the angiographic suite. CardioVascular and Interventional Radiology, 43, 820–826. https://doi.org/10.1007/s00270-020-02476-8
Maki, D. G., Kluger, D. M., & Crnich, C. J. (2006). The risk of bloodstream infection in adults with different intravascular devices: A systematic review of 200 published prospective studies. Mayo Clinic Proceedings, 81(9), 1159–1171. https://doi.org/10.4065/81.9.1159
McDiarmid, S., Scrivens, N., Carrier, M., Sabri, E., Toye, B., Huebsch, L., & Fergusson, D. (2017). Outcomes in a nurse-led peripherally inserted central catheter program: A retrospective cohort study. CMAJ Open, 5(3), E535–E539. https://doi.org/10.9778/cmajo.20170010
Medicare Access to Radiology Care Act of 2019, H.R. 1970, 116th Cong. (2019-2020). https://www.congress.gov/bill/116th-congress/house-bill/1970/
Meyer, B. M. (2010). Implementing and maintaining an infusion alliance. Journal of Infusion Nursing, 33(5), 292–303. https://doi.org/10.1097/NAN.0b013e3181ee01f5
Organization for Occupational Radiation Safety in Interventional Fluoroscopy. (2015). Occupational exposure to ionizing radiation in interventional fluoroscopy: Severity of adverse effects of a growing health problem [White paper]. https://orsif.org/wp-content/themes/twentyfourteen-child/download.php?file=posters_download/ORSIF-WhitePaper-Feb-Supplement_V8_WEB.pdf
Pittiruti, M., & Pinelli, F. (2020). Recommendations for the use of vascular access in the COVID-19 patients: An Italian perspective. Critical Care, 24, 269. https://doi.org/10.1186/s13054-020-02997-1
Ruegg, L., Federi, R., & Choong, K. (2020). Peripherally inserted central catheter-associated complications: A retrospective review of a nurse-led peripherally inserted central catheter-insertion service. Vascular Access, 6(1), 16–19. https://search.informit.org/doi/epdf/10.3316/informit.139151047982690
Sandrucci, S., & Mussa, B. (Eds.). (2014). Peripherally inserted central venous catheters. Springer-Verlag Mailand. https://doi.org/10.1007/978-88-470-5665-7
Scamperle, K. (2013). The fee-for-service shift to bundled payments: Financial considerations for hospitals. Journal of Health Care Finance, 39(4), 55–67.
Tomaszewski, K. J., Ferko, N., Hollmann, S. S., Eng, S. C., Richard, H. M., Rowe, L., & Sproule, S. (2017). Time and resources of peripherally inserted central catheter insertion procedures: A comparison between blind insertion/chest x-ray and a real time tip navigation and confirmation system. ClinicoEconomics and Outcomes Research, 9, 115–125. https://doi.org/10.2147/CEOR.S121230
Toomay, S., Vaughan, F., Collins, J., & Eastbrooks, M. (n.d.). Interventional radiology throughput optimization [Unpublished results]. University of Texas Southwestern Medical Center. https://www.iise.org/uploadedFiles/SHSNew/InterventionaRadiologyThroughputOptimization.pdf
U.S. Food and Drug Administration. (2010). Initiative to reduce unnecessary radiation exposure from medical imaging [White paper]. https://www.fda.gov/radiation-emitting-products/initiative-reduce-unnecessary-radiation-exposure-medical-imaging/white-paper-initiative-reduce-unnecessary-radiation-exposure-medical-imaging
Walker, G., & Todd, A. (2013). Nurse-led PICC insertion: Is it cost effective? British Journal of Nursing, 22(19), S9–S15. https://doi.org/10.12968/bjon.2013.22.Sup19.S9
