Opioids: What Do Healthcare Professionals Want and Need to Know?
The availability of, and access to effective and safe treatments for pain remain serious problems in the United States (Institute of Medicine, 2011). Opioid medications are important for addressing short-term and chronic pain management. Given the benefits that they provide, usage of opioids has become widespread over the past decade. However, opioid medications also carry substantial risk, and their increased usage has introduced a host of unintended consequences across the care continuum. Given this, opioids have significant implications for patient safety. The National Patient Safety Foundation (NPSF) conducted a convenience flash poll survey to obtain a snapshot of opioid-related patient safety concerns, learning needs, and familiarity with existing seminal publications among healthcare professionals.
The number of prescribed and dispensed opioids doubled between 1999 and 2010, according to the U.S. Department of Health and Human Services (HHS) as quoted in the National Action Plan for Adverse Drug Event Prevention (HHS ODPHP, 2014). In inpatient settings, a 2012 research database of 1,665,418 hospitalized patients showed that 72% of patients treated with IV analgesia received IV opioid monotherapy.1 In ambulatory care settings, research indicates that as many as 20% of patients with pain-related diagnoses or non-cancer pain symptoms (including chronic and acute pain) presenting to physician offices receive a prescription for an opioid medication (Daubresse et al., 2013). Further, a Joint Commission Sentinel Event Alert reports that “[o]f the opioid-related adverse drug events, including deaths, that occurred in hospitals and were reported to The Joint Commission’s Sentinel Event database (2004–2011), 47% were wrong-dose medication errors, 29% were related to improper monitoring of the patient, and 11% were related to other factors, including excessive dosing, medication interactions, and adverse drug reactions” (Joint Commission, 2012).
Postoperative respiratory depression is a particular concern for inpatients. “Opioids can sedate the part of the brain that controls breathing, causing the lungs to slow and ultimately stop” (Association for the Advancement of Medical Instrumentation, 2015). Research indicates that this condition may impact as many as one in 200 hospitalized postoperative surgical patients (Frederickson et al., 2015; Dahan, Aarts, & Smith, 2010). Other opioid-related adverse drug events include over-sedation; gastrointestinal intestinal events (e.g., nausea, constipation, vomiting); pruritus; opioid-induced hyperalgesia; and immunological and hormonal dysfunction (HHS ODPHP, 2014).
In ambulatory settings, opioid pain medication use presents the potential for opioid use disorder (also known as abuse, dependence, or addiction) and overdose. The 2013 National Survey on Drug Use and Health conducted for the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) found that as many as 1.9 million people abused or were dependent on prescription pain relievers, including opioids (HHS SAMHSA, 2014). Separately, the number of prescription opioid overdose deaths increased annually between 1999 and 2010, reaching 16,651 deaths in 2010—a number that surpasses the total of heroin and cocaine overdose deaths combined (HHS ODPHP, 2014; ECRI Institute, 2015). Given the inherent risks of opioid medications and their potentially serious impact on patients, opioid management is a patient safety issue.
Survey
NPSF conducted a flash poll survey of 18,070 healthcare professionals to better understand opioid-related patient safety concerns, learning needs, and familiarity with existing seminal publications.
Results
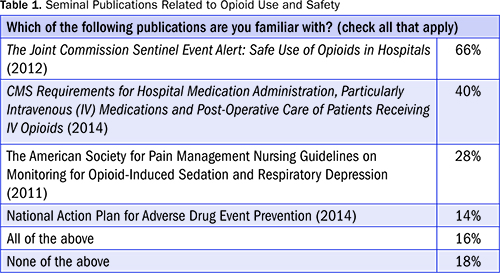
While the flash poll survey response rate was low (3%), the findings warrant consideration. One of the more illuminating results is a lack of familiarity with key publications related to opioid use and safety (Table 1). Nearly 20% of respondents indicated that they were not familiar with any of the seminal publications issued by governmental agencies, regulators, and professional societies. While 66% of survey participants indicate being familiar with one publication, The Joint Commission Sentinel Event Alert, 49: Safe Use of Opioids in Hospitals, this finding is also concerning given that nearly 21,000 inpatient and ambulatory healthcare organizations and programs in the United States are currently accredited by The Joint Commission, including 77% of hospitals (Joint Commission, n.d.a., n.d.b.). Even fewer respondents (40%) reported being familiar with the CMS Requirements for Hospital Medication Administration; these requirements emphasize the need for postoperative monitoring of patients receiving IV opioid medications, and the lack of familiarity with them is eye-opening given that most U.S. hospitals participate in Medicare and are required to comply with its directives.
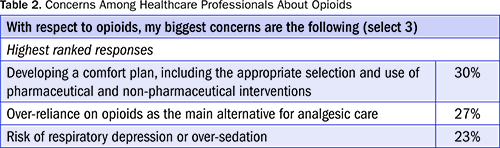
In addition, the results show a concern among respondents that over-reliance is placed on opioids in patient care. In the survey, respondents rank-ordered their concerns related to opioids, as shown in Table 2.
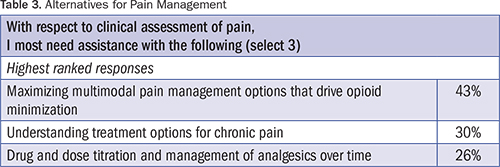
Results also indicate that there is broad interest in learning more about alternatives for pain management (Table 3).
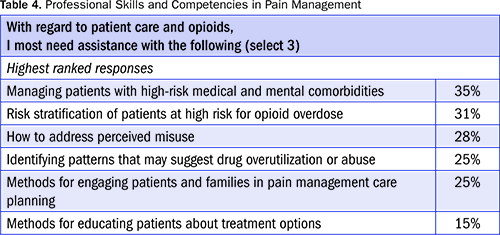
Finally, results show strong interest and desire among respondents to acquire additional skills and competencies in gauging patient comfort and developing multimodal pain management plans, as well as patient engagement strategies (Table 4).
Conclusion
Although they confer important pain-reducing benefits, opioid medications carry substantial risk and have significant implications for patient safety. NPSF conducted this survey to better understand healthcare professionals’ concerns, learning needs, and familiarity with existing seminal publications related to opioids.
While survey respondents indicate a surprising lack of familiarity with existing publications, they report interest in more education. In addition, respondents voice concern that over-reliance may be placed on opioids in patient care and express interest in learning about alternatives for pain management, as well as acquiring additional skills and competencies in gauging patient comfort, developing multimodal pain management plans, and engaging patients.
When a sizable number of professionals indicate that they need help developing a skill set, we have a clear call to action. In sum, the results indicate that greater clinician education is needed to ensure opioid medications are used appropriately and only after multimodal treatment options have been attempted. By strengthening this foundational understanding, professionals may be better able to establish and manage appropriate options for pain management and reduce the risk of patient harm. Considerable effort is spent discussing the problems created from opioid use, but in addition to discussing how to address the medications’ inherent risks, the focus should begin with how to better evaluate patients and employ multimodal pain treatment options. The latter discussion could result in less use of opioids and less risk for patients.
NPSF recommends the following:
- Educate all members of healthcare teams regarding key publications on opioid safety
- Ensure that all professionals involved in prescribing and/or providing opioids demonstrate competencies in assessing pain, creating multimodal comfort plans, and adapting plans in a timely manner based on the changing conditions of patients
- Conduct additional research to prioritize and address all educational needs of healthcare professionals with respect to pain management and opioids
Limitations
The survey has various limitations that should be considered when interpreting the results. We used a flash poll survey to collect feedback, which by design allowed for only a limited number of questions. Hence, no single area is examined in depth. In addition, given that responses draw from a convenience sample, there is a potential for bias. Finally, the relatively low response rate and the likelihood that the majority of respondents have a safety-related interest preclude our ability to generalize our findings to the broader community.
Acknowledgments
NPSF gratefully acknowledges Roy Soto, MD, professor and residency program director in the department of anesthesiology, Oakland University William Beaumont School of Medicine, and Chris Pasero, pain management educator and clinical consultant, for their expert subject-matter guidance; Shiella Radel, Northeast regional business director, hospital division, Mallinckrodt Pharmaceuticals, for assistance with the flash poll survey development; and Paula Griswold, executive director, Massachusetts Coalition for the Prevention of Medical Errors, for assistance disseminating the survey.
The authors work for the National Patient Safety Foundation.
Patricia McGaffigan is chief operating officer and senior vice president of programs.
Caitlin Lorincz is senior program director and may be contacted at clorincz@npsf.org.
Tejal Gandhi is president and CEO.
References
Association for the Advancement of Medical Instrumentation. (2015). Opioid safety & patient monitoring conference compendium. Retrieved from http://s3.amazonaws.com/rdcms-aami/files/production/public/FileDownloads/HTSI/Opioids/2015_Opioid_Compendium.pdf
Dahan, A., Aarts, L., & Smith, T. W. (2010). Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology, 112, 226–238. Retrieved from http://anesthesiology.pubs.asahq.org/article.aspx?articleid=1932606
Daubresse, M., Chang, H. Y., Yu, Y., Viswanathan, S., Shah, N. D., Stafford, R. S., … Alexander, G. C. (2013). Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010. Medical Care, 51, 870–878. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24025657
ECRI Institute. (2015, April). Top 10 patient safety concerns for healthcare organizations. Retrieved from https://www.ecri.org/Pages/Top-10-Patient-Safety-Concerns.aspx
Frederickson, T. W., Gordon, D. B., De Pinto, M., Kral, L. A., Furnish, T., Gupta, R., & Austin, P. A. (2015). Reducing adverse drug events related to opioids implementation guide. Society of Hospital Medicine Center for Hospital Innovation & Improvement. Retrieved from http://tools.hospitalmedicine.org/resource_rooms/imp_guides/radeo/radeo_implementation_guide.pdf
Institute of Medicine. (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press.
Joint Commission. (n.d.a.). About The Joint Commission. Retrieved from http://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx
Joint Commission. (n.d.b.). Facts about hospital accreditation. Retrieved from http://www.jointcommission.org/facts_about_hospital_accreditation/
Joint Commission. (2012, August 8). Safe use of opioids in hospitals. The Joint Commission Sentinel Event Alert, 49. Retrieved from http://www.jointcommission.org/assets/1/18/SEA_49_opioids_8_2_12_final.pdf
U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. (2014, September). Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. (2014). National action plan for adverse drug event prevention. Retrieved from http://health.gov/hcq/pdfs/ade-action-plan.pdf
