No Hidden Patient: Facility Design for Safety
September / October 2006
No Hidden Patient: Facility Design for Safety
![]()

![]()
Designing a new hospital or medical center around patient safety principles is the most important challenge facing facility planners and architects today. A facility’s layout, equipment, and furnishings strongly influence the effectiveness of care, safety, and satisfaction of patients and caregivers.
Traditionally, the best inpatient care centers have been designed to look like hotels, not like medical centers. But the number-one rule of architectural design, “function precedes form,” dictates that safety-enhancing features should precede hotel-like amenities. Hotels are designed for customer satisfaction, including the customer’s desire for peace, quiet, and privacy. In the hotel setting, peace and quiet are enhanced by placing the bathrooms and closets close to the room entry, near the corridor, insulating the bedroom from corridor traffic and noise as much as possible. In this layout, the bathroom and closet are referred to as being “inboard.”
In hospitals, patient safety concerns must precede privacy. When the patient is visible and accessible, the caregiver’s ability to observe and act quickly is improved. When planners choose patient privacy over safety, they are in essence choosing form over function.
Following hotel design, most medical/surgical patient care centers are designed with “inboard” bathrooms that make it difficult for nurses to see patients. In most cases, nurses must travel down the corridor, enter a doorway, walk around an inboard bathroom, and fully enter the room to see the patient. This layout is inconvenient for caregivers and potentially hazardous for patients. It gives priority to privacy and convenience of the housekeeping staff over patient safety functions.

![]()
Many medical center planners get around this visibility problem by creating “nurse observation-and-work alcoves” between patient rooms, with small glass windows for viewing the patient. The “alcoved” nurse stands or sits in isolation while watching one or two patients through little windows into the room. There are at least two problems with this setup: it’s still corridor-based, and the alcoves restrict communication among clinical nursing, professional, and medical staff. It takes nurses away from the central workstation where patient care-planning conferences can be held with other clinical, medical, and professional staff, and there is a false and risky assumption that a nurse will be sitting at that alcove at all times.
Both of these traditional designs — nursing alcoves and rooms with inboard bathrooms arranged on long corridors — pose risks to patients. I now advise my clients to use what I call the “No Hidden Patient” care center design.
The concept of No Hidden Patient came to me after reading a news story about a tragic event in a hospital in my hometown. It was reported that a floor nurse on a medical/surgical unit had been notified by the monitor tech in the intensive care unit of a disturbance shown on a patient’s monitor. The nurse walked down the long corridor to the patient’s room, turned into the room around the inboard bathroom, and saw that the patient was not in bed. The nurse assumed the patient was in the bathroom and left. Seven minutes later, the patient was discovered lying on the floor on the other side of his bed, as it turned out, too late to save his life.
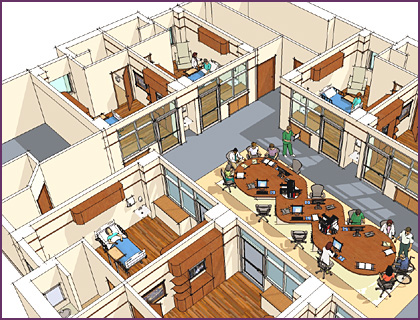
From that point on, “No Hidden Patient” became my mantra for all patient care centers, not just the intensive care unit. The No Hidden Patient design includes outboard bathrooms and glass inboard walls for unimpeded visibility. Privacy can be provided, via curtains or window-blinds, at the discretion of the patient’s physician and clinical nursing staff. This high-visibility plan is often used in intensive care units (ICUs), but I believe it should be incorporated in all inpatient areas including emergency, observation, trauma, surgical, and invasive diagnostics prep and hold, among others.

![]()
Similarly, to maximize safety for patients and caregivers, I recommend that hospitals redesign the traditional workstation, which isolates nurses behind high counters and tends not to provide an environment conducive to meaningful communication among caregivers. Clinicians often leave the traditional, outward-facing, counter-style nursing station in search of a quiet place to work. Physicians and visitors standing at the counter block the nurses’ view of patients in their rooms. The congestion at the counter-style workstation also creates cross-traffic problems when clinical nursing staff need to reach their patients in a hurry.
Another design — nursing worktables — can be adapted from ICUs to replace traditional nursing workstations and enhance safety in all areas of the hospital. (See sidebar.) Nursing worktables are reminiscent of traditional dining room tables in the way they function, lending themselves naturally to formal and informal face-to-face meetings among clinical, medical, professional, and administrative staff. It’s easy to pull up a chair to work at a computer or to join a meeting, and just as easy to get up to attend to a patient.
The worktable design can be modified for the needs of different departments. In the emergency department, I recommend that the worktable be higher, with bar-style chairs or stools, so that the oft-harried physicians and nurses may use computers, telephones, records, and other technologies while standing, sitting, or just leaning against the furniture before dashing off to see another patient.
![]()
To assure patient safety in the layout of a patient care center also requires that the planners consider “caregiver safety” as well. It is a known fact that clinical nurses are getting older (average age in USA: 42), and many are now presenting with foot, knee, and hip ailments from all the walking necessary during a single shift on a traditional single- or double-corridor “racetrack” patient care unit. Yet with sicker patients in today’s hospitals, we need clinical nursing staff that can leap up without a thought to assist a patient in need. How can they do that if they are sore and tired? The No Hidden Patient hospital is patient-focused and nursing-focused.
When patients wake up feeling disoriented or uncomfortable, you don’t want them also to feel isolated. If on opening their eyes, they see another person, their fears are immediately assuaged. And if the person they see happens to be a nurse who may easily enter the room to touch the patients in word or deed, then care becomes synonymous with the innate promise of the hospital that says, “You’re in good hands.” With No Hidden Patient design, the hospital says, “You’re in good eyes” too!
- Genesis of the Clinical Nursing Worktable
Jeff Hardy is an operations planner and new facility designer. He is president of Healthcare Enterprise Development Services in Novato, California. For further information, call 800/233-5313, email jhardy@jhardy.com, or visit www.jhardy.com.
