Mentoring Programs: Essential for Sustaining a Culture of Safety
March/April 2013
![]()
Mentoring Programs: Essential for Sustaining a Culture of Safety
An effective mentoring program can strengthen a healthcare enterprise’s performance in many areas, including quality improvement, risk management, personnel recruitment and retention, staff education, and leadership. By enhancing staff knowledge and team integration, mentoring programs help support an enterprise-wide culture of safety, which, in turn, helps minimize adverse patient occurrences and related financial losses. This article examines the theory and practice of mentoring, focusing on how adult learning strategies and ongoing managerial support can improve mentor-mentee rapport and produce better outcomes for participating individuals and the organization. Sample worksheets are included, to help create and evaluate a mentoring program.
Understanding Mentoring
Mentoring is defined as “an enhancement strategy through which one person [the mentor] facilitates the development of another [for the purposes of this article, the mentee] by sharing known resources, expertise, values, skills, perspectives, and proficiencies” (Triple Creek Associates 2007). The goal is to foster relationships, behaviors, and activities that embody the organization’s core principles and sustain a healthy organizational culture that remains stable and can withstand changes in the operating environment.
Organizations committed to a culture of safety tend to be “learning organizations” (Domrose 2009), dedicated to two-way communication and ongoing staff development. Internal mentoring is a key learning and teaching strategy that allows the organization to retain skills and create continuity, with positive implications for succession planning efforts and long-term sustainability. As mentoring activities proliferate, staff commitment to the program tends to intensify. The information that mentors share with mentees is later shared by mentees with others (Peddy 1998), making mentoring a self-perpetuating process.
Mentoring also can help foster risk awareness, resulting in fewer errors and decreased liability exposure. Properly mentored employees learn through emulation to become leaders in patient safety and quality improvement efforts. When work teams exhibit mentoring behaviors—for example, by pooling knowledge and working together in a flexible and collaborative manner—they are better positioned to identify systemic issues before serious problems occur (AHRQ 2008).
At a time of chronic shortages of nurses and other healthcare workers, mentoring can be a useful tool for bolstering staff retention and recruitment results. In one research study, three-quarters of surveyed organizations reported that mentoring programs were valuable for increasing retention (Barbian 2002). Another study reported a decrease in turnover of 20% associated with mentoring programs (Alleman & Clarke 2000).
Mentorship helps sustain morale by demonstrating that the expertise and experience of veteran staff members are valued. Moreover, such programs personify a spirit dedicated to helping newcomers thrive and grow. Healthcare organizations with a reputation for successful mentoring programs are, therefore, inclined to recruit and retain better- motivated employees, increasing quality of care and reducing exposure.
Mentoring partnerships can flourish only when mentees believe that openness is rewarded and issues can be discussed honestly, without fear of retaliation or impetuous blame. Without these protections, participants become over-cautious and disengaged, the program loses momentum, and the morale of both mentees and mentors may suffer. Successful mentorship is about more than one-on-one relationships; it involves an organization-wide commitment to personal accountability, communication, and trust. Mentorship also may exhibit multiple mentoring models, such as mentoring circles and peer and team mentoring (Ambrose 2003).
Working with Adult Learners
Mentoring involves adult learners, who tend to be self-directed and goal-oriented (Knowles 2005). Mature adults, with their previously acquired knowledge and life experiences, are often motivated more by internal goals and personal satisfaction than younger learners. Mentoring programs thus should establish a vigorous and respectful educational environment that acknowledges mentees’ history and treats them as peers and colleagues. Research shows that a failure to recognize past experiences can result in feeling devalued and ignored, which can undermine the learning process (Knowles 1990).
The mentoring process begins with development of the initial framework for a teaching plan, often created by an in-house team comprising human resources professionals, risk managers, education and training specialists, and clinical leaders knowledgeable about relevant operational processes. The framework should align objective job demands and expectations based on job descriptions, departmental policies and procedures, and established best practice, using worksheet formats (see Figures 1 and 2). The planning objective is to ensure that mentees understand:
- which skills and strengths are already present,
- what they need to learn,
- which capabilities require further development, and
- what is expected of them in their new role and how it differs from past situations.
|
Figure 1. Sample Self-Appraisal Worksheet
* Core actions that support competencies |
|
Figure 2. Sample Teaching Plan Worksheet
* Core actions that support competencies |
Learning activities will focus on assessing and developing essential competencies related to these job needs, as well as recognizing the mentee’s prior knowledge and perceptions of abilities. The mentee’s self-appraisal worksheet (Figure 1) is completed and jointly reviewed with the mentor, with findings incorporated into a collaborative and cohesive teaching curriculum through use of a teaching plan worksheet (Figure 2). The teaching plan worksheet:
- outlines mutual expectations for the mentoring experience;
- lists the core skills, knowledge, and actions needed to perform learning objectives; and
- describes teaching methods, peer observation/verification of learning behaviors, and next learning steps.
The mentor can use the teaching plan worksheet to create an individualized experience that considers the level, history, and learning style of the mentee. This worksheet will reflect the teaching plans and mentee’s learning evolution, as the mentor becomes acquainted with the mentee. In addition, the mentee will discover more about the organization and specific performance expectations. Observations and revised planning goals should be documented on this worksheet following mentoring sessions.
Self-appraisal is a critical aspect of the mentoring process. It should be viewed positively, as a means of self-discovery for the mentee, intended to encourage discussion and strengthen the relationship with the mentor.
Managing Issues
Mentoring involves establishing open and supportive interpersonal relationships, which can be a psychologically and emotionally challenging process. The following guidelines can help create healthy boundaries and mitigate some of the more common problems that may arise:
- Foster compatible relationships. Realistically, not every mentor is suitable for every mentee, and vice versa. Encourage both to be honest about the nature of comfortable partnership in terms of age, sex, personality type, and professional attainment, and respect these preferences to the extent possible.
- Maintain a clear distinction between mentor and supervisor. Mentorship emphasizes support rather than assessment, and combining these different functions can lead to confusion and conflict. Mentors and mentees should be able to discuss learning activities and related sensitive subjects honestly, without a fear that disclosures will go on the record in the form of negative performance evaluations.
- Encourage gradual autonomy and self-reliance. Mentoring relationships tend to create an initial dependence, as the mentee looks to the mentor for both guidance and approval. The mentor can bolster the mentee’s leadership skills and decision-making ability by providing flexibility and ongoing positive feedback, until the mentee develops the requisite self-confidence to act independently and develop similarly trusting relationships with others. While mentor-mentee relationships may continue, at least informally, beyond the agreed-upon time limit, they should taper off in intensity as the mentee gains in experience and poise.
- Mentor the mentors. Mentoring is a demanding process, and mentors should have access to a seasoned and reliable advisor with whom they can chart strategies, discuss conflicts, and vent feelings. The advisor should exercise some degree of supervision and offer an occasional tactful reminder of the need to model professional, respectful, and sensitive behavior toward mentees.
- Take steps to prevent mentor “burn-out.” There is always a risk of overloading mentors, who must fulfill their own organizational responsibilities while they are teaching others. Mentoring should be treated by leadership as a serious and time- consuming commitment, factored into performance evaluations, and rewarded in terms of recognition and career advancement.
A successful mentoring program helps humanize the workplace by encouraging the treatment of staff not as passive order-takers motivated by avoidance of punishment, but as partners and potential leaders with an emotional stake in the enterprise. As the level of fear within an organization declines, commitment increases. A more compassionate, patient-focused culture and a lower level of risk are thereby achieved.
Evaluating the Mentoring Experience
Each learning experience should be evaluated jointly by the mentor and mentee in a timely manner, through use of the following threshold questions, among others:
- Were both parties adequately prepared and motivated?
- Did the mentee fully communicate his or her thoughts and questions?
- Did the mentee understand the learning objectives and address the associated core actions?
- Was the mentee able to identify his/her strengths and weaknesses objectively?
- Did the mentor incorporate narratives, examples, hypothetical situations, and other adult teaching strategies?
- Was the mentee able to identify risks, alternatives, and acceptable solutions?
- Did the mentor provide adequate guidance and support?
- Was the mentor objective about his/her own teaching strengths and possible biases?
The duration of the mentoring experience depends on various objective and subjective factors, including the mentee’s learning pace, comfort level, observed competence, and the availability and types of experiences.
The mentor determines when the mentee is able to function independently, based on the ability to:
- consistently perform the core actions associated with specific learning objectives;
- apply learned concepts and principles to specific scenarios provided by the mentor (Figure 3), since not all types of experiences are available for learning ; and
- identify appropriate resources that can be used to help solve actual or potential problem.
|
Figure 3. Case Scenerio Based upon findings arising from the previous patient safety rounds addressing medication safety, the team’s recommendations on involving Pharmacy in staff training have not been implemented. |
All stakeholders—the mentee, the mentor, and leadership—should participate in the evaluation process by addressing the following questions:
- Was the program of sufficient duration?
- Was supervision adequate?
- Was constructive rapport established between the mentor and mentee?
- Did both parties receive regular and useful feedback from the other during the mentoring process?
- Were learning and teaching goals achieved?
While learning never ceases, the formal mentoring relationship comes to a natural conclusion when the mentee demonstrates command of core skill sets and the ability to apply those competencies to real-world scenarios. If the agreed-upon end date arrives, and goals have not been entirely met, the participants may request additional time together or, in consultation with management, may consider alternative strategies.
Assessing the Mentorship Program
Leadership is ultimately responsible for evaluating the mentoring program. Benchmark indicators, such as recruitment and retention figures, quality measures, and employee satisfaction levels, should be established and closely monitored. Program evaluation efforts also should examine how the mentoring program affects mentors, in terms of additional workload, compensation issues, fairness, professional satisfaction, and continued role expectations. Administrators must understand that mentors are expected to maintain assigned workloads while engaged in mentoring activities. They also must recognize that mentees learn at different rates and require different levels of time and effort. In light of these variables, management should maintain a flexible attitude, as well as a reasonable ratio of mentors to mentees, in order to preclude overload and “burnout.”
 |
|
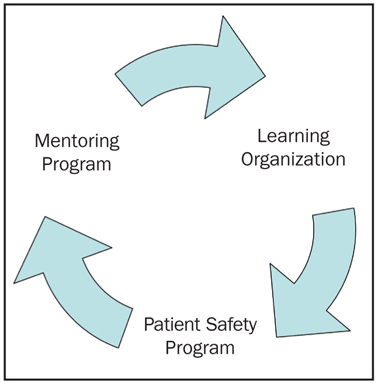
| Figure 4. Sustainability through Mentoring |
From a quality perspective, the mentorship program should be objectively evaluated on an ongoing basis according to cogent, consistently applied criteria. Senior management should respect mentors’ observations regarding their mentees’ progress and prospects. However, management’s perspective differs from that of mentors, focusing less on the learning process and more on overall performance. The process works best when all parties—mentors, mentees, and organizational leadership—regularly communicate and work together to develop clearly articulated educational objectives.
The American College of Healthcare Executives (ACHE) states that an enterprise-wide commitment to patient safety and quality improvement involves “a culture of improvement that includes an organization-wide commitment to continuous learning” (ACHE 2008). An effective, ongoing mentorship program represents the cornerstone of a learning culture and long-term sustainability. A sound mentorship system supports this commitment, promoting safety and reducing risk through staff development, training, and leadership (Figure 4).
Conclusion
Many areas of healthcare management—including staff recruitment and retention, education and training, quality improvement, patient safety, and risk management—can benefit from carefully planned, leadership-supported mentoring programs. By supporting internal learning experiences and relationships, organizations can foster improved performance and morale, nurture future leaders, and prepare to meet the many challenges and changes that will present in the years ahead.
Mary Seisser is a CNA healthcare risk-control consulting director who provides consulting services to healthcare organizations and their providers through risk assessment, education, and development of tools and resources. Seisser’s 35-year career as a healthcare professional includes experience as a clinician, nurse educator, published author, and national presenter on the topics of healthcare risk management, quality, and patient safety. Seisser earned a bachelor of science degree (major in nursing) from Northern Illinois University and a master of science degree in nursing (major: medical-surgical nursing; minor: teaching) from the University of Texas at Austin. She may be contacted at mary.seisser@cna.com.
Rosalie Brown is a CNA healthcare risk-control director, responsible for leading healthcare consulting services for the eastern and mid-Atlantic regions. Brown has more than 25 years of healthcare experience, including an extensive background as a surgical staff nurse, educator, administrator, and risk manager for an integrated delivery system in Pennsylvania. She has presented a variety of risk management programs at the state and local level. Brown graduated from the Coatesville Hospital School of Nursing in Pennsylvania and received a bachelor’s degree from Graceland College in Iowa and a master’s degree in healthcare administration from Wilkes University in Pennsylvania. She may be contacted at Rosalie.Brown@cna.com.
References
