Medical Mayhem Room: Enhancing Situational Awareness of Patient Safety Risks in the Hospital Setting
By Marcie Metroyanis, DNP, RN, NEA-BC, Patricia Reagan Webster, PhD, CPPS, and Robert Panzer, MD
Abstract
Background: Medical errors are the third leading cause of death in the United States (Makary & Daniel, 2016). Situational awareness, monitoring, and remediating risks in the clinical setting are hallmarks of the high reliability necessary to prevent patient harm.
Design: To enhance awareness of hazards of medical errors that jeopardize the safety of patients, we created a “Medical Mayhem Room” to simulate safety risks that may be found in the patient care environment. Scenarios for each simulated patient included diagnosis, age, allergies, and precautions or special considerations. We deliberately introduced mistakes and hazards into each of these scenarios. The Medical Mayhem Room staged four patients with a total of 95 patient safety risk factors.
Implementation: A team of experienced nurses developed simulation scenarios, compiled medical supplies, and staged the scenarios with deliberate medical errors. This team also greeted participants, explained how to navigate through the activity, and provided a debriefing.
Outcomes: Participants in this learning activity included 310 nurses, attending physicians, advanced practice providers, patient care technicians, pharmacists, environmental service workers, and other clinical support staff. The average time spent for participants to assess all of the patients was approximately 45 minutes. While participants identified 100% of the risks, some errors were far less likely to be detected than others. Eighty percent of the participants indicated that they learned something new about a safe environment in a patient care area, while 93% indicated that they found value in the activity.
Background
Hospitals are a critical part of our healthcare system and a place where very ill people can get excellent, and often life-saving, care. However, it has been well established that hospitals can also be very dangerous for patients (Institute of Medicine, 2000; James, 2013). Patient safety specialists work with caregivers and clinical staff to develop systems, processes, and protocols that reduce safety risks associated with hospitalization. While these tools are important in preventing or mitigating human error, they do not replace the vigilance needed by all healthcare workers to keep patients from experiencing preventable harm.
The further reduction of safety risks requires that all providers, nurses, and other staff in the clinical environment are aware of the unsafe conditions they routinely see and often, unintentionally, cause. Aspects of the high reliability necessary to prevent patient harm include situational awareness, monitoring, and remediating risks in the clinical setting (Fore & Sculli, 2013). Nursing and medical schools are increasingly aware of the importance of teaching students about the hazardous conditions found in hospitals through use of experiential safety activities (Penn State News, 2013; Farnan et al., 2016; Clay et al., 2017). However, as these students become busy caregivers and clinicians in hospitals, they often overlook the risks that could harm their patients. Safety hazards become part of the clinical landscape.
To increase situational awareness of safety hazards in the hospital setting, quality improvement staff at Strong Memorial Hospital, the flagship hospital of a large academic medical center, implemented an experiential learning activity, the Medical Mayhem Room, during National Patient Safety Week in March 2019. This workplace-based activity was designed as a voluntary educational opportunity for nurses, resident and attending physicians, pharmacists, and other clinical support staff.
Implementation
To begin the development of the Medical Mayhem Room, six experienced nurses of varying expertise formed a project team. Prior to moving forward with project planning, the team had to identify adequate physical space to accommodate four simulated patients. Once this was done, the project team outlined the various components required to develop the activity. First, the team created basic scenarios for each patient and included diagnosis, age, allergies, and precautions or special considerations. This was followed by gathering supplies and equipment based on the details of the scenarios. The planning also incorporated costs and advertising (Figure 1).
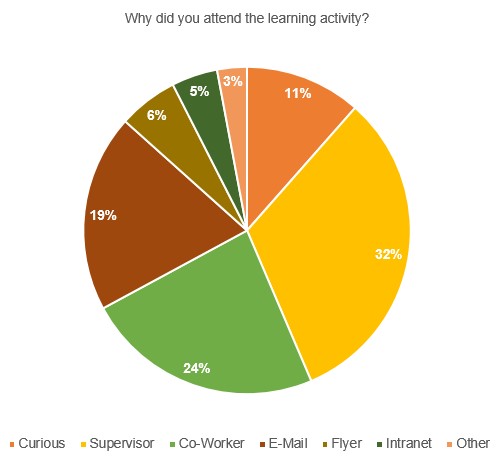
Figure 1. Advertising Methods
Design of the workplace simulation
There are a variety of methods to increase learning and engagement among healthcare workers and achieve patient safety goals. We decided to adopt the “Room of Horrors” simulation approach by staging errors and hazards for healthcare workers to identify during an assessment (Farnan et al., 2016). The activity here is referred to as the “Medical Mayhem Room,” a simulated hospital room filled with medical and environmental issues and concerns.
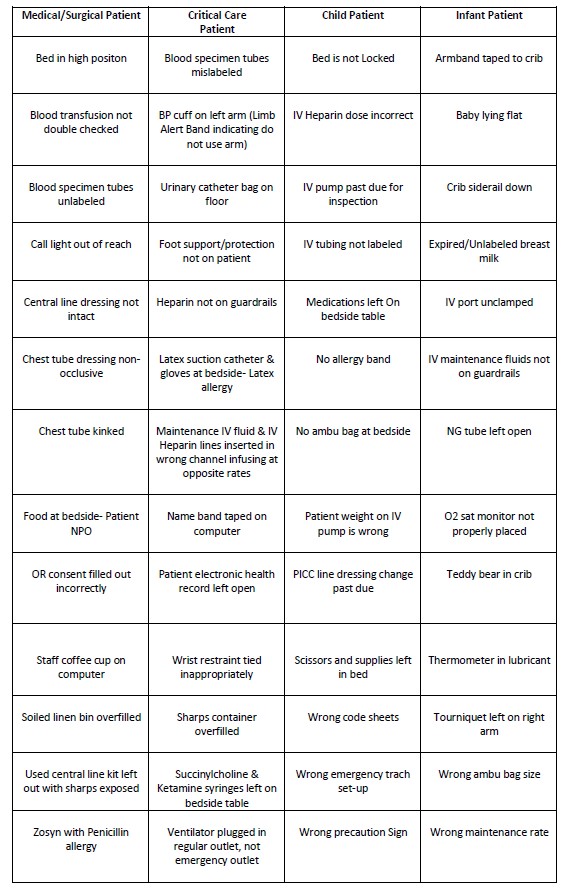
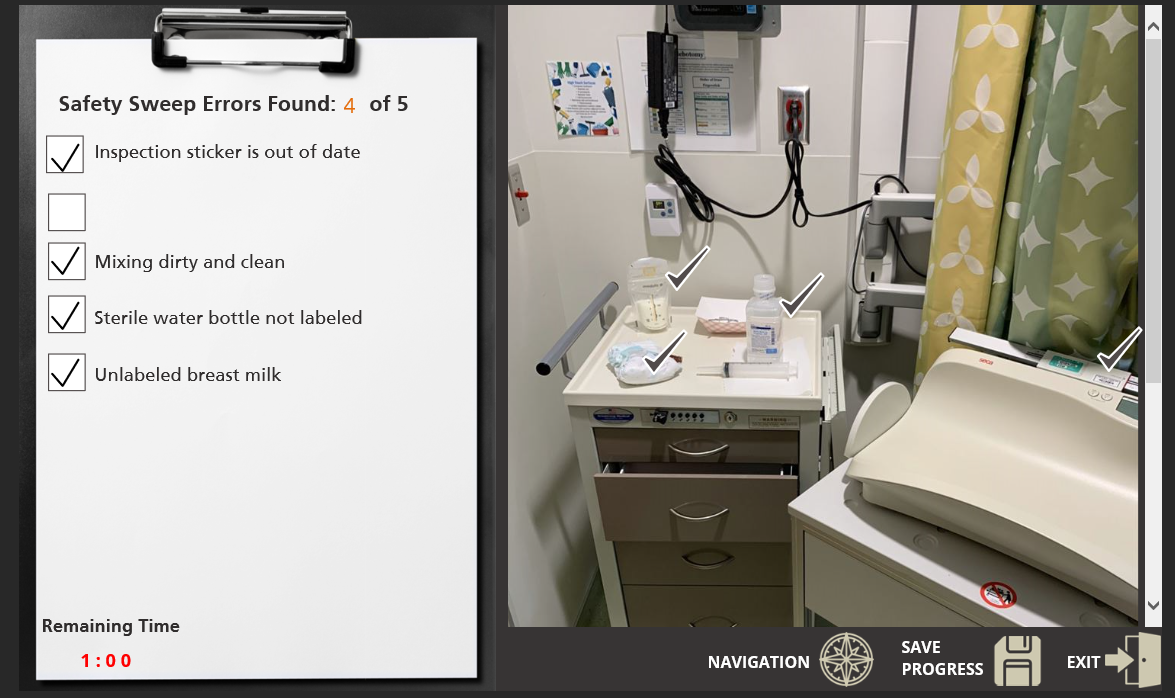
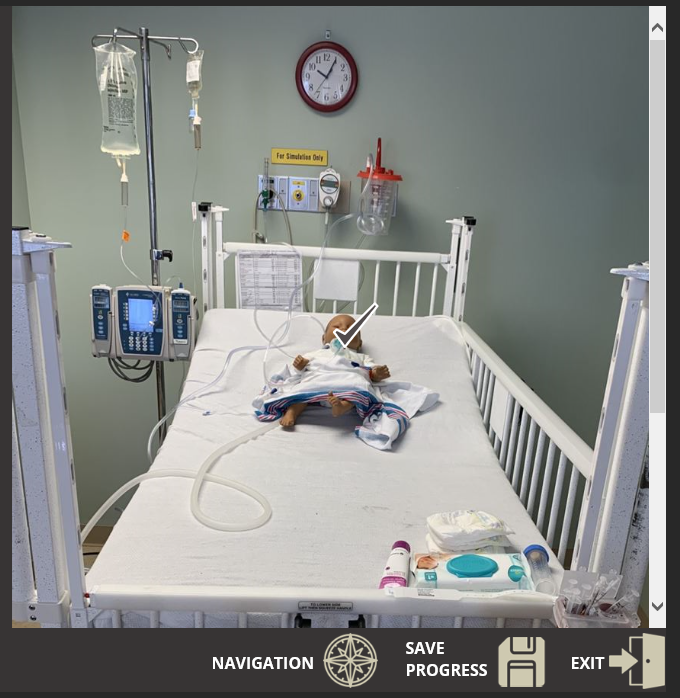
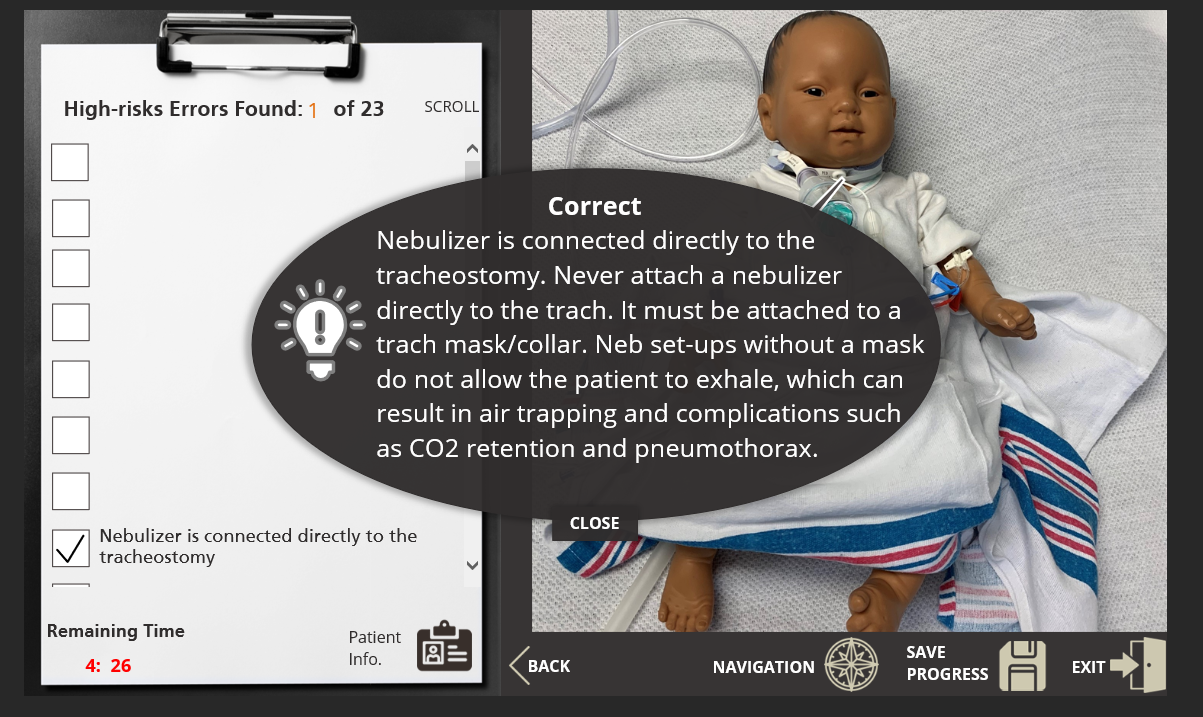
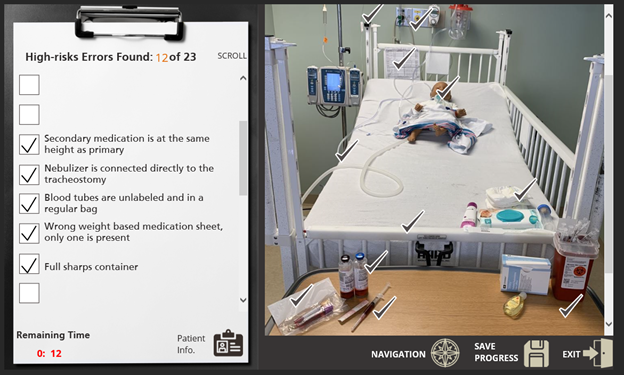
The first Medical Mayhem Room session consisted of four patient scenarios including a medical/surgical patient, an adult critical care patient (Figure 2), a child, and an infant (Figure 3). Each patient had unique types of errors according to their age and acuity, plus similar errors that occurred across all four patients. In total, 95 types of patient safety risk factors and environmental issues were staged among the four simulated patients. Types of errors and hazards within the room included, but were not limited to, patient physical safety, appropriate use of devices, IV medication management, oxygen management, patient identification, expired items, and patient documentation management (Table 1).
Figure 2. Adult Critical Care Patient

Figure 3. Infant
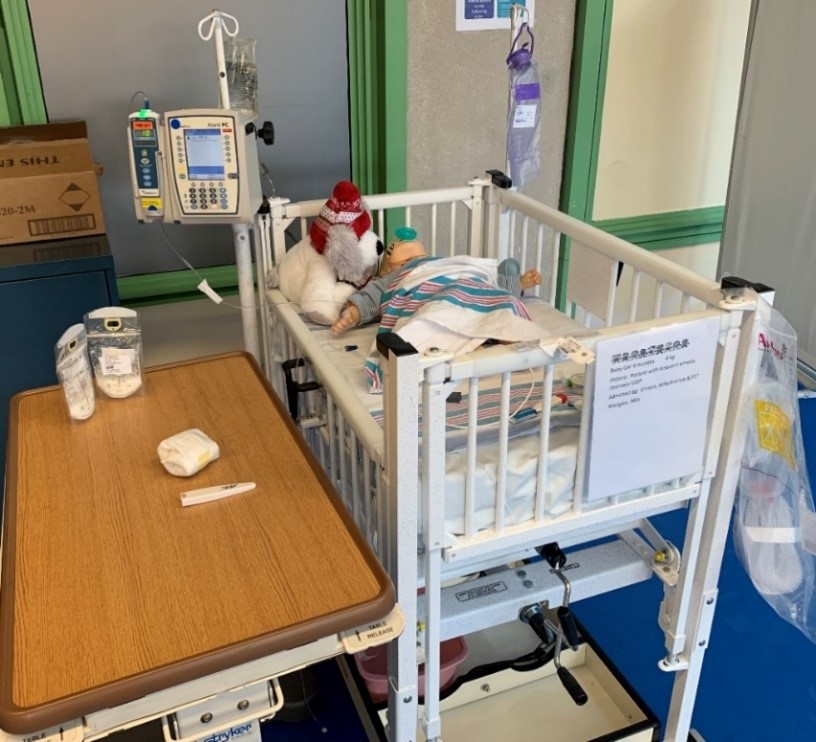
Table 1. Sample of Patient Safety Risks Included
The next step was to develop tools such as an activity sheet for participants to track their findings while assessing the patients and their patient care environment. As participants toured the room and assessed the patients, they would record the mistakes and hazards they found for post-project evaluation.
Once each participant completed the activity, they were offered an opportunity to review the errors compared to their own findings. Upon exiting the room, each participant was provided a debriefing that included risk reduction strategies and information about high reliability and the journey to zero preventable harm. Following the debriefing, participants could undergo a voluntary evaluation.
Outcomes
Participants in this learning activity included 310 nurses, attending physicians, advanced practice providers, patient care technicians, pharmacists, environmental service workers, and other clinical support staff. Nonclinical healthcare workers enjoyed the experience and were also able to identify what they thought were errors and hazards. For example, one environmental service worker was assessing a patient and stated, “I do not know what this is, but it doesn’t look right.” This reflected an effective safety culture as we strive to encourage all hospital employees to “see something, say something.”
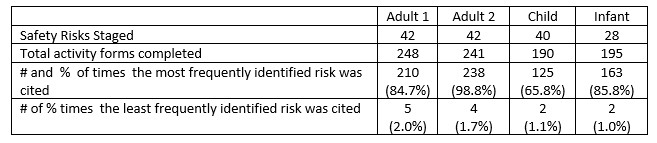
A total of 95 types of errors were staged among the four simulated patients. To accommodate a consistent learning experience despite any time constraints, some of the same errors were staged on each patient. As a result, each simulated patient had 28–42 safety risks staged as part of the learning experience (Table 2).
Participants were not evaluated on their ability to find all of the staged risks because we did not have control over the amount of time each participant could devote to the activity. Furthermore, participants often worked in teams and may have only turned in one scoring sheet for the team. Based on the conversations between facilitators and participants, the variation in time spent during the activity was primarily due to the availability of time away from clinical care or other work duties. On average, participants took 10 minutes to assess one patient followed by 5–10 minutes of debriefing; therefore, it took approximately 45 minutes to complete the entire activity.
We were able, however, to assess the relative likelihood of detecting different medical and environmental safety risks. The number of identified risks varied across participants. While all of the risks were identified by at least one participant or team, some types of risks were far more likely to be identified than others. Over 200 participants caught food at the bedside of an NPO (i.e., nothing by mouth) patient, while only five identified the illegibility of an initial signature on a blood transfusion. Similarly, though 238 participants found an overfilled small sharps container at the bedside, just 14 found an unlocked vent and only six found unclamped saline locks. One hundred twenty-five participants found scissors and supplies left in a child’s bed, while only two participants caught a pump due for inspection. Likewise, 162 participants found expired unlabeled breast milk, while only 19 participants noted the infant’s wrong weight and just two participants identified an infiltration. Table 2 demonstrates the range in the likelihood that safety risks would be detected.
Table 2. Likelihood That Safety Risks Are Detected
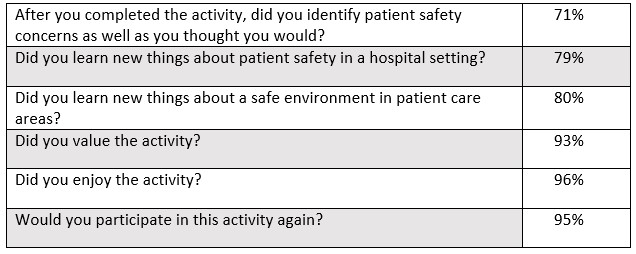
According to the post-survey results, 70%–80% indicated that they identified safety concerns as well as they expected and learned something new about safe patient care and a safe environment; 93%–96% had a positive experience and reported that they would participate in future activities. Eighty percent of the participants indicated that they learned something new about a safe environment in a patient care area, while 93% concluded that they found value in the activity (Table 3).
Table 3. Medical Mayhem Post-Activity Evaluation
Key insights
Our experience with the Medical Mayhem Room safety simulation demonstrated that:
- Hospital caregivers have varying degrees of awareness regarding patient safety risks based on errors and hazards that occur at or around the bedside.
- Simulating patient safety errors and risks in a setting that mimics a typical hospital room helps teach and reinforce the importance of complying with protocols, standards, and guidelines.
- Establishing the simulated patient room near patient care units ensured that more healthcare workers could take part in the educational activity.
- The number of errors discovered among participants varied, and some participants may have been overconfident that they would recognize all of the errors prior to completing the exercise; both of these findings indicate an ongoing need for patient safety education.
- Participants learned while performing assessments, having discussions with each other, and generally enjoying the experience.
- The most frequently overlooked safety risks and errors provided insight into areas that may require further education and reinforcement. Some of these included (in addition to the ones mentioned previously) past-due PICC line dressing change, no allergy band, wrong precaution sign, inaccurate weight programmed in IV pump, wrong IV fluid maintenance rate, and crossed IV lines (IV fluids and medications infusing on wrong channel at opposite rates).
Next steps
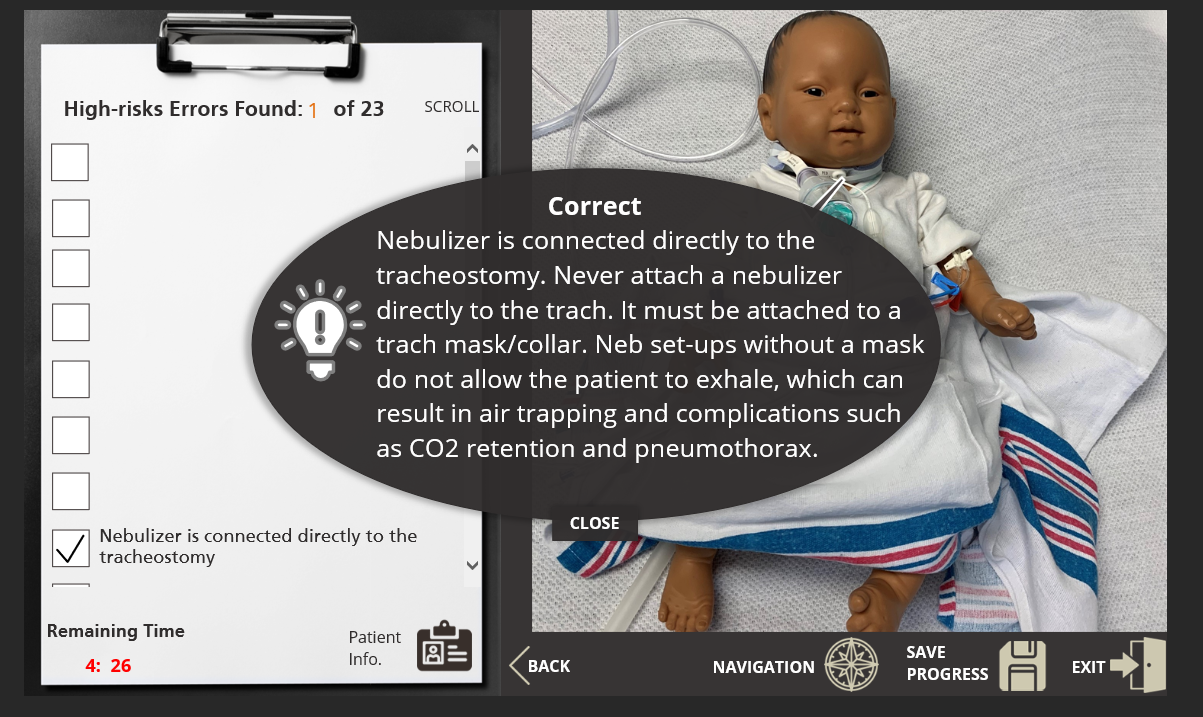
The Medical Mayhem Room served as a pilot for developing future experiential learning opportunities around patient and staff safety. Based on the data and observations collected during the activity, the Medical Mayhem Room was a positive experience for a majority of participants. As most claimed the activity was enjoyable and valuable, the activity will continue to be offered on an ongoing basis. During the COVID-19 pandemic, the structure of the program will convert from a hands-on method to an electronic interactive approach (Figure 4) to ensure the safety of our staff, nurses, and providers. The goal is to develop a library to accommodate all clinical specialties, support staff, and students. This will require simulated setup and staging of a wide range of patient populations. It will also require clinical experts from each department and nursing service to collaborate with the Medical Mayhem Room coordinators to ensure that each scenario is accurate and that common and high-risk errors are identified. Each room will be recorded, capturing all medical and environmental errors. The program will then be available online in an interactive format to enhance the learning opportunity.
Figure 4. Online Learning Module
Marcie Metroyanis, DNP, RN, NEA-BC, is assistant quality officer, Patricia Reagan Webster, PhD, CPPS, is associate quality officer, and Robert Panzer, MD, is chief quality officer at University of Rochester Medical Center.
References
Clay, A. S., Chudgar, S. M., Turner, K. M., Vaughn, J., Knudsen, N. W., Farnan, J. M., Arora, V. M., & Molloy, M. A. (2017). How prepared are medical and nursing students to identify common hazards in the intensive care unit? Annals of the American Thoracic Society, 14(4), 543–549. https://doi.org/10.1513/AnnalsATS.201610-773OC
Farnan, J. M., Gaffney, S., Poston, J. T., Slawinski, K., Cappaert, M., Kamin, B., & Arora, V. M. (2016). Patient safety room of horrors: A novel method to assess medical students and entering residents’ ability to identify hazards of hospitalization. BMJ Quality & Safety, 25(3), 153–158. https://doi.org/10.1136/bmjqs-2015-004621
Fore, A. M., & Sculli, G. L. (2013). A concept analysis of situational awareness in nursing. Journal of Advanced Nursing, 69(12), 2613–2621. https://onlinelibrary.wiley.com/doi/abs/10.1111/jan.12130
Institute of Medicine. (2000). To err is human: Building a safer health system. The National Academies Press.
James, J. T. (2013). A new, evidence-based estimate of patient harms associated with hospital care. Journal of Patient Safety, 9(3), 122–128. https://doi.org/10.1097/PTS.0b013e3182948a69
Makary, M., & Daniel, M. (2016). Medical error—the third leading cause of death in the US. BMJ, 353, i2139. https://doi.org/10.1136/bmj.i2139
Penn State News. (2013, October 29). College of nursing gives students “spooky” assignment to stress patient safety. http://news.psu.edu/story/293127/2013/10/29/academics/college-nursing-gives-students-spooky-assignment-stress-patient
