ISMP: U-500 Insulin Safety: It’s Time to Rethink Safe Use Practices
By Institute for Safe Medication Practices
As the obesity epidemic continues and insulin resistance problems worsen, larger doses of insulin are more frequently required to meet glycemic goals. This has led to an increased use of U-500 insulin when dose requirements exceed 200 units per day. Along with the increased use of U-500 insulin, the Institute for Safe Medication Practices (ISMP) has been receiving a growing number of U-500 insulin-related medication error reports and/or complaints from health professionals. Most of the reports are related to dosing confusion caused by not having a syringe with a U-500 scale. This usually requires practitioners to rely on measuring doses with a U-100 syringe and teaching the patient to communicate doses in “syringe units”—that is, measure 200 units of U-500 insulin by drawing up 40 “syringe units” on the U-100 syringe. But too often, patients do not understand the difference between U-100 and U-500, so they inaccurately state the actual dose, saying, for example, that they take 40 units of insulin, which can lead to hyperglycemia if only 40 units are then prescribed. Worse, confusion can also lead to overdoses. If people using a U-100 syringe misunderstand “syringe units,” a dose of 80 units of U-500 insulin might be prepared by measuring 80 units on the U-100 scale instead of 16 “syringe units,” resulting in a dose of 400 units.
 |
|
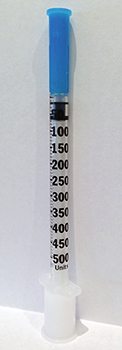
| Figure 1. Prototype U-500 Insulin Syringe |
It is difficult to understand how a high-alert drug like insulin was ever allowed to be available without a corresponding way to measure doses accurately (e.g., a U-500 syringe). Instead, practitioners have been forced to improvise by using a U-100 syringe, which we believe is more error-prone than using a tuberculin syringe that measures U-500 doses by volume. Indeed, a U-500 syringe would seem to be a much better option by providing markings appropriate for U-500 insulin. Recently, the Department of Veterans Affairs (VA) published research on a prototype U-500 syringe design (Abraham et al., 2013). One of the goals of the evaluation was to observe intuitive selection of the correct syringe for a corresponding dose. More than 100 subjects (clinicians, and experienced and inexperienced patient groups) were asked to select the correct syringe among either a U-500 syringe (Figure 1) or a U-100 syringe given three different dosing situations. When the U-500 insulin doses were below 100 units, the majority of subjects chose a U-100 syringe instead of the U-500 syringe. In such a case, the patient could receive a 5-fold overdose when using U-500 insulin. With clinicians alone, 47% chose the wrong syringe (U-100), probably thinking it would be more accurate for doses less than 100 units. The authors of this study noted a variety of other vulnerabilities with the U-500 syringe and offered helpful recommendations for improving its design.
What about an insulin pen for U-500? Given that far fewer patients receive U-500 insulin than U-100 insulin, and given the well known confusion brought about by not having a corresponding U-500 syringe, at the present time we believe a U-500 insulin pen would be the best option, despite our recommendation earlier this year to consider transitioning away from insulin pen use in hospitals. Lilly and BD will not provide information about whether this is in the works, and FDA is unable to comment on any products that may or may not be under development. However, there are additional strengths of insulin now under development that will only add to the confusion if a pen is not made available. Sanofi-Aventis is developing U-300 glargine (LANTUS), Novo-Nordisk is developing U-200 degludec (brand name TRESIBA outside the United States), and Lilly is developing a U-200 HUMALOG (insulin lispro). Tresiba is already on the market in the United Kingdom and is only available in a pen. Given the syringe selection issues raised in the U-500 insulin study, we strongly recommend that these new products be available in the United States only in a pen. If development of a U-200 syringe and/or a U-300 syringe is being considered, that will only add to inventory problems, selection issues, confusion, and medication errors. Indeed, mix-ups between syringe types were common when U-40 and U-80 insulins were available for a time, along with U-100 insulins (Moss & Galloway, 1997).
One final issue with U-500 insulin that perhaps can also lead to confusion is name similarity. HUMULIN R is the name for both the U-100 and the U-500 product even though they have different concentrations and different pharmacokinetics. It is time to rethink this, as name similarity has contributed to product selection errors from the shelf during dispensing and from the computer screen while prescribing, as well as communication errors during medication reconciliation. The same issue could arise with the new higher strength insulins (e.g., Lantus, HumaLOG). It is worthwhile studying whether or not a name change or the addition of a suffix to the more concentrated forms would help differentiate them.
Until U-500 syringes or pens are available for U-500 insulin, ISMP continues to believe that it would be far less confusing to all concerned if tuberculin syringes were used to measure doses by volume using a dosing conversion chart (Conversion information for Humulin, 2013). Total doses should be expressed in terms of both units and volume (i.e., 200 units [0.4 mL]). That way, the U-100 scale and associated confusion would not arise. One issue that has come up, however, is reimbursement for patients using tuberculin syringes. Some insurers will not cover the cost. That is shortsighted given the financial cost of dosing errors. We can only hope that insurers will begin to cover the cost of using the most appropriate syringe with higher concentration insulin.
This column was prepared by the Institute for Safe Medication Practices (ISMP), an independent, nonprofit charitable organization dedicated entirely to medication error prevention and safe medication use. Any reports described in this column were received through the ISMP Medication Errors Reporting Program. Errors, close calls, or hazardous conditions may be reported online at www.ismp.org or by calling 800-FAIL-SAFE (800-324-5723). ISMP is a federally certified patient safety organization (PSO), providing legal protection and confidentiality for patient safety data and error reports it receives. Visit www.ismp.org for more information on ISMP’s medication safety newsletters and other risk reduction tools. This article appeared originally in the October 31, 2013, issue of the ISMP Medication Safety Alert!
Institute for Safe Medication Practices. (2014). U-500 Insulin safety: It’s time to rethink safe use practices. Patient Safety & Quality Healthcare, 11(2), 16–18.
References
Abraham, K., Patail, B., & Wurth, D. (2013). Usability testing of a U-500 insulin syringe: A human factors approach. Patient Safety & Quality Healthcare, 10(5), 38–43. Available at http://www.psqh.com/september-october-2013/1753-usability-testing-of-a-u-500-insulin-syringe-a-human-factors-approach
Conversion information for Humulin® R U-500 (Concentrated) Insulin Dose. (2013 July). Lilly, USA. Retrieved from http://www.humulinhcp.com/Documents/pdfs/Conversion_Chart.pdf
Moss, J. M. & Galloway, J. A. (1977). U-100 insulin. A progress report. JAMA, 238(17), 1823–1824. doi:10.1001/jama.1977.03280180027018
