Informed Consent for Rapport and Communication
May / June 2008
![]()
Informed Consent for Rapport and Communication
![]()
If true to their Hippocratic Oath, healthcare providers are deeply committed to ensuring that their actions are nothing less than helpful and curative. They go to great lengths to safeguard against errors, oversights, actions, or omissions that might intensify symptoms, exacerbate disease states, or cause death.
But no matter how dedicated their efforts, mistakes occur and some diseases are not cured. This leaves providers with the onerous task of delivering bad news to the patient and family. These situations are, at best, uncomfortable and, at worst, devastating. It makes sense for healthcare professionals to carefully consider how they can adequately prepare themselves to disclose adverse effects and apologize for disappointment (poor outcomes) or harm (iatrogenic outcomes) if appropriate.
Preparing to Deliver Bad News
“Bad news” falls into one of two broad categories:
- Disappointing or unfavorable outcomes, when the recommended treatment did not fully produce the results desired. For instance, I treated a prostate cancer patient several years ago. We had discussed both radical surgery and radioactive seed therapy. He chose the latter but, unfortunately, his cancer recurred. The patient was understandably disappointed — as was I — but appreciative of the information that I had previously provided him.

- Medical errors, where a healthcare provider made a mistake — sometimes with no repercussions but other times with deadly consequences. A radiologist might overlook a simple hairline fracture on an X-ray of a fractured tibia that eventually heals without intervention, for instance. On the other hand, a nurse may administer the wrong dose of heparin to a cardiac patient, resulting in death. These, clearly, are more difficult issues to address.
Both categories are potentially explosive. Yet the impact of the news, as well as the patient’s reaction, will be greatly affected by the relationship he or she has developed with the provider. If the provider has been open and upfront throughout diagnosis and treatment, the patient’s response will reflect the trust that has been established. If confidence is lacking, the provider can expect anger, accusations, and possible legal action.
“Disclosure” Begins with First Visit
The concept of “disclosure” — which is really “communication” by another name — should be initiated long before bad news may need to be delivered. It begins with the first office visit or encounter, when the provider has the opportunity to establish rapport with the patient. At that point, doctors, non-physician practitioners, nurses, and medical assistants are able to engage the patient as a “partner” on the healthcare team. Ongoing dialogue and a genuine concern for the patient’s long-term well-being cement a mutually respectful and trusting relationship.
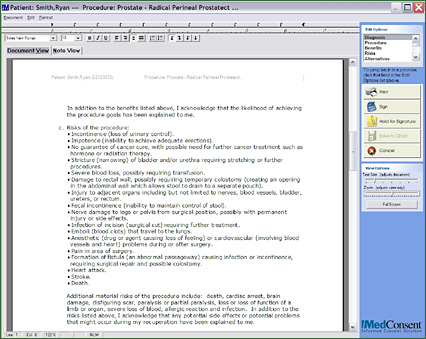
This collaboration is advanced by discussions surrounding informed consent. Increasingly, circumspect healthcare providers view informed consent as an ongoing process — not a one-time, form-signing event. It entails detailed discussions that fully explain the patient’s condition and factors that affect it. In addition, the provider is able to outline the benefits likely to result from recommended tests, studies, or treatments — as well as the potential risks and the impact they might have on subsequent decisions. Patient and provider can also explore the full spectrum of possible outcomes, as well as side effects affiliated with the procedure.
Within the context of these factors, the provider can likewise present alternative therapies and the pros and cons of each. In fact, this discussion was largely responsible for the composed reaction of my prostate cancer patient whose cancer recurred. He told me that he was comfortable with his decision to undergo the seed therapy and, because he fully understood his available choices and their risks, he was able to accept the results he experienced.
Informed Consent Encourages Dialogue
In other words, thorough informed consent discussions ensure that “disclosure” is inherent to the entire process. Patients are made aware of virtually all factors that might affect their health. They will be less likely to say, “I did not realize that could happen,” or “I wish I had known about option number 2.” I often hear this in my practice as a urologist. Patients treated elsewhere for prostate cancer who subsequently suffer from erectile dysfunction frequently tell me they had not understood the magnitude of this risk before their procedure.
Overall, informed and involved patients are empowered to make better healthcare decisions and choices, are more compliant with instructions, and are more satisfied with their care experience. This satisfaction — and the positive relationship they share with their provider — typically means patients are less likely to initiate litigation in the event of errors or undesirable outcomes.
Without a doubt, comprehensive consent activities require a greater investment of time and effort on the provider’s part. However, it has also been noted that better communication, afforded by tools employed during the informed consent process, may be key to reducing a physician’s risk of lawsuits (Baum & Dowling, 2007). Providers are supported in this by employing automated systems. Applications supply a library of customizable consent forms and can often be appended directly to the patient’s medical record electronically. In addition to documenting the consent process, these software solutions put reproducible materials at the provider’s fingertips — making it easy to educate patients. Best-of-class applications can be customized to a patient’s specific circumstances and are written in jargon-free terminology.
This approach to ensuring that disclosure is in effect an extension of the informed consent process has proven valuable during my tenure as a physician. I have been subjected to only one malpractice lawsuit in my 38-year career. The patient presented with elevated PSA, but the initial biopsy of his prostate was benign — as was his second. A few years later, we performed yet another biopsy that revealed a malignancy. I expressed my regret about the diagnosis, and we spent an hour discussing his options. Nevertheless, he considered the benign biopsies medical errors and sued. Fortunately, our informed consent discussions at the time of the first biopsy were comprehensive and well-documented. The signed informed consent form indicated that the patient had been told there might be an undetectable malignancy and that he might need further biopsies to confirm his condition. This validated the propriety of my actions and the case was judged in my favor.
![]()
Obstacles to Productive Dialogue
Besides the investment of time and effort, other obstacles interfere with a provider’s inclination to establish productive dialogue with patients. These are not topics routinely covered at most medical schools. Instead, providers are typically left to their own instincts when it comes to patient relations, which often leads to suboptimal results.
Some providers are not “natural communicators.” They may be at the top of their field and unmatched in skill but find it difficult to hold extensive conversations with patients. Fictional Dr. Gregory House, from the wildly popular television program, House MD, epitomizes these providers.
Many providers likewise struggle with social, cultural, or gender barriers with patients. Providers raised in a highly stratified society may have difficulty relating to patients who are members of a different class — and vice versa. Other providers are hesitant to discuss certain topics with members of the opposite sex — perhaps a daughter has accompanied her father as interpreter to discuss a prostate condition, for example. In other instances, communication may be impeded by the patient’s relatives. A colleague of mine once treated an elderly gentleman who spoke no English and his family wished to keep his cancer diagnosis from him.
A smaller portion — those providers who still adhere to the “omniscient physician” philosophy — may regard disclosure and apology as a sign of weakness. These providers are often placed in this position by their patients — patients who want to abdicate their role in the informed consent process (“Doc, do what you feel is best”). As a result, these providers are concerned that admission of failure or error will undermine their patients’ confidence in their professionalism and skill.
Perhaps the most significant impediment, however, is fear of litigation. Providers are not entirely sure about what they are “allowed” to say. This uncertainty is often reinforced by risk managers and malpractice insurance carriers who insist that the less said, the better.
This position has been much debated in recent years. In fact, organizations such as the Sorry Works! Coalition (www.sorryworks.net) have promoted a viewpoint that is diametrically opposed to the traditional “suppression” model. Sorry Works encourages providers to adopt a customer service mentality throughout their enterprise to facilitate communication and problem solving with patients and families after adverse events.
![]()
Strategies Overcome Communication Barriers
To overcome barriers to communication, the healthcare industry as a whole must adopt a wide range of strategies to normalize disclosure and, when appropriate, apologies. Providers should be trained about how to most effectively encourage dialogue with patients — beginning in medical school and continuing within healthcare organizations and practices. Leadership should make tools and technology available to support providers throughout informed consent processes and other opportunities for relationship building.
At the same time, providers need to be fully informed about state laws, facility directives, and medical malpractice insurance polices that guide their approach to disclosure and apology. Many do not understand, for instance, that offering a simple apology for an undesirable outcome or even an error is often acceptable. According to a January 1, article in the New York Times, 17 states have enacted legislation encouraging such apologies, some even making providers’ expressions of remorse inadmissible in court (Jauhar, 2008). The same article notes, “Physicians’ apologies do not necessarily increase malpractice lawsuits. In fact, they may protect against litigation.”
Because attitudes toward disclosure and apology are in flux, many forward-thinking healthcare leaders are devising programs to guide provider actions. This may include advance training, briefings about situations that require special attention, and cheat-sheets to help providers determine who best to respond when bad news needs to be delivered. It may be wise, also, for organizations to consider establishing a special “risk response team,” available to providers when difficult situations arise. This team can facilitate the provider’s conversation with the patient or family — supporting the established relationship and maintaining trust, while avoiding potential legal and professional hazards.
Without a doubt, patients and providers are best served if disclosure of an unfavorable outcome is less of a surprise to all. Ideally this disclosure, and acknowledgement of regret in regard to the outcome, is part of the ongoing communication that extends from the first visit until treatment is completed. When executed effectively, patients have a greater understanding of their condition, treatment options and attendant risks, while providers benefit from the increased confidence in their judgment and abilities. And, at the end of the day, this proactive, collaborative approach discourages patients from pursuing retribution through the courts.
James Gottesman is a practicing urologist in Seattle. He also serves as a consultant for Atlanta-based Dialog Medical, a leading provider of informed consent and patient education systems for hospitals and physician practices. He may be contacted at james.gottesman@comcast.net.
References
Baum, N. H., & Dowling, R. A. (2007, February 1). Informed consent: Use it to improve care, reduce risk. Urology Times. Available at www.modernmedicine.com/modernmedicine/article/
articleDetail.jsp?id=401902
Jauhar, S. (2008, January 1). Explain a medical error? Sure. Apologize too? The New York Times. Available at www.nytimes.com/2008/01/01/health/views/01case.html
