Improving Adult Immunization Delivery with Policy Changes and Clinical Support Technology
September / October 2008
![]()
Improving Adult Immunization Delivery with Policy Changes and Clinical Support Technology
In the United States, vaccine-preventable diseases cost in excess of $10 billion annually. Pneumococcal disease and influenza combined were the 8th leading cause of death in 2004 (Kung, et al., 2008). Despite this, adult immunization rates continue to lag behind rates in pediatric populations, due to a variety of system, practice- and patient-level barriers that have been overcome in effective pediatric immunization programs (Nichol & Zimmerman, 2001; Santibanez et al., 2002; Fiebach 1991). Learning from the lessons of successful pediatric immunization initiatives could help improve the lagging rates in adults.
In the mid 1990s, the Denver Health and Hospital Authority (DHHA) aspired to improve pediatric immunization rates within its vertically integrated health system. This health system currently consists of 8 community health centers, a 500-bed public hospital, the local public health department, and 12 school-based health centers as well as the 911 emergency response system, regional poison control center and nurseline, correctional care, and a managed care division. In 1995, a pediatric immunization initiative resulted in the development of a computerized immunization registry and an algorithm programmed within the registry, which served as a standing order for routine pediatric immunization. The standing order was based on the current age of the patient, prior vaccination history, interval since last vaccine(s) in series, and a pediatric vaccination schedule recommended by the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices (CDC ACIP). Over time, this initiative led to a dramatic improvement in pediatric immunization rates (Melinkovich, 2007).
Case Study
The success of pediatric immunization rates in DHHA was in sharp contrast to immunization rates in adults. Chart audits showed static levels of adult immunization over the years despite several small projects implemented to improve rates. Efforts to vaccinate patients in the inpatient setting were inconsistent, documentation was uncoordinated across different parts of the system, and primary care providers had difficulty determining whether a patient had been vaccinated while hospitalized. And, unlike the process used for pediatric immunizations, DHHA did not use clinical decision support tools to identify adults eligible for immunization at the point of care. Due to the challenges in accessing documentation of immunization, vaccines were not prioritized in light of a patient’s multiple other medical issues.
In fall 2002, DHHA began an initiative to address this quality gap in adult immunizations. Under the guidance of a Denver Health Immunization Advisory Committee, this large integrated healthcare system prioritized using the registry as the central repository for administered adult immunization in addition to its current pediatric use. Vaccine history of immunizations administered at outside institutions, e.g., senior centers, grocery stores, etc, could also be entered into the registry so the registry would be complete. Accurate documentation in the registry allowed for better tracking of adult immunizations throughout the DHHA system, but immunization rates did not increase dramatically.
It was determined that for this registry to drive improvement of immunization rates, processes needed to be incorporated into routine clinical patient care visits (or ‘flow’). DHHA’s community health centers began using electronic patient check-ins by medical assistants in 2004. As part of this check-in process, vaccine history was entered into an electronic database, the lifetime clinical record (LCR). However, because the LCR and the immunization registry were not linked, the multiple step-process required to merge this information was unwieldy.
The adult inpatient services at Denver Health did not initially utilize the immunization registry and lacked processes to administer immunizations other than as part of a few key clinical pathways. In 2004, in response to a Joint Commission best practice guidelines, DHHA implemented paper standing orders for influenza and pneumococcal vaccination in the inpatient setting. At this time, all immunizations given were documented in the immunization registry.
This article describes the innovative work of a collaboration between DHHA, the Colorado Clinical Guidelines Collaborative (CCGC), a nonprofit healthcare quality improvement organization focused on the development and implementation of clinical guidelines for primary care providers, and Colorado Health Outcomes Program (COHO) to improve adult immunizations through a combined immunization registry, an electronic clinical decision support system, and a standing order.
Implementing Solutions
In August 2005, DHHA partnered with CCGC to improve pneumococcal, influenza, and tetanus immunization rates among adults in the DHHA system. A steering committee with oversight of three task forces was created: one responsible for inpatient care, the second for outpatient care, and the third for information systems (IS) issues.
Data from the immunization registry, “VaxTrax,” were analyzed and revealed variation in immunization rates among community health center clinics. It was decided to pilot efforts at one family medicine site and one internal medicine site. This program included implementation of a standing-order policy for adult immunization with the clinical decision support tools to support that policy. A summary of the multiple components of these quality improvement activities is provided in Table 1.
| Table 1: Improvement Activities | ||
|
||
|
||
|
||
Gathering Stakeholders
The DHHA Office of Regulatory Compliance appointed a multidisciplinary oversight committee with representatives from several departments including inpatient and community health services, information systems, pharmacy, and the immunization program. The committee included clinicians, data systems analysts, nursing educators, and managers. This oversight committee directed the project and sought input from additional participants as needs arose. In addition, several other stakeholders received regular progress reports on the project and were able to provide suggestions, assistance, or clarification on institutional policies and procedures.
Development of Clinical Decision Support Tools for Standing Orders
One of the goals of the quality improvement initiative was to develop a standing immunization order for adults that could be carried out by medical assistants without a written order from a provider. As the IS department was developing the immunization clinical decision support tool (CDST), members from CCGC and DHHA addressed any concerns about the quality of data in the registry, the reluctance of some providers to relinquish responsibility for assessment of immunization eligibility, and the impact on clinic flow of this new standing-order system. This group addressed each of these hurdles, patterning suggested changes after those known to be successful with our pediatric patients.
A standing order was only possible with a clinical decision support tool that could assess which patients were eligible for recommended vaccination(s) at the point of care. Because immunization recommendations are contingent on adult medical conditions and the registry did not contain ICD diagnoses, the registry alone could not generate recommendations. Linking the VaxTrax immunization registry electronically with the LCR made this feasible. While VaxTrax would remain the legal medical record and repository for all immunizations, these immunizations would populate the LCR and then the patient-specific ICD-9 codes contained within the LCR and the vaccine history from the registry were queried by the LCR to determine if a patient was due for vaccination. Distinct algorithms based on the CDC ACIP adult immunization guidelines were written for each vaccine. This proved to be a fairly complex process as it was not always easy to determine which ICD-9 codes should be included. For example, CDC guidelines recommend pneumovax for chronic heart disease but it wasn’t clear if this includes ischemic heart disease, valvular heart disease, and arrhythmias.
Though it was not possible to include some vaccination indications in the electronic system, e.g. chronic care facility residence or current medications, the immunization CDST bases its recommendation on ICD-9 codes, patient age, and immunization history. The standing-order policy implemented to accompany this CDST states that the medical assistant can use this computerized CDST in conjunction with existing routine immunization screening questions to administer immunizations. In addition, for influenza immunization, the process associated with use of CDST included yes/no questions administered by the medical assistant to detect additional indications for immunization including if the patient resided in a long-term care facility, cared for young children, or lived with an adult with a chronic disease. Any affirmative answers to routine screening questions are referred by the medical assistant to the provider for provider evaluation of possible precaution/contraindication to vaccine(s). To ensure patient privacy, the message generated by the CDST does not specifically indicate the diagnosis that prompted the recommendation.
Programming the CDST required several months due to pre-existing tasks that took priority for information systems. In February 2007, the new tool was ready for pilot testing.
Development of Standing-Order Policy
It was clear that increasing adult immunization rates across community health centers relied on all providers adhering to the same procedure. Therefore the standing-order policy provided a way to inform, educate, and enforce that there would be a standard procedure for all sites to follow and that individual providers would allow medical assistants to use the immunization CDST for assessment and administration of needed immunization. The standing-order policy was brought to the appropriate committee and approved in February 2007.
Intervention Roll Out
In fall 2006, before the LCR rule and policy were created, initial improvement efforts began at one family medicine pilot site. The pilot site formed a work group, and staff members were given feedback on their immunization rates and educated about vaccine eligibility and safety of revaccination.
By February 2007 the LCR adult immunization clinical decision support tools (CDST) and new standing-order policy were ready to be implemented. The family medicine pilot site and an internal medicine site implemented the new approach to adult immunization delivery. The new standing-order policy authorized medical assistants to administer PPV, influenza, and/or Td immunizations using the LCR clinical decision support tools as standing orders.
While the clinics were testing the LCR tools and policy, the CCGC project manager met with the work groups approximately weekly and was available by telephone so the nursing program managers at each clinic could call to ask questions, report barriers, or request additional information. The two pilot sites differed in how they implemented the standing orders, but both included certain key steps: run the LCR immunization CDST at the time the patient is checked in, inform the patient about the immunizations using Vaccine Information Statements (VIS forms provided by CDC), complete the standard adult immunization screening questions before immunizing, and develop a process for involving the provider in the event of patient refusal or potential contraindication to immunization.
In early April 2007, the CDST and standing-order policy was presented to all practice managers, and they were informed that the new CDST and approach to adult immunization was from that point onward official policy for community health services. The rollout to other clinic sites began in early May and was completed by mid July. At the same time, the CDST was also beginning to be implemented in the inpatient setting.
There were instances when providers questioned why the CDST was recommending vaccination for some diagnostic classifications of patients. When reviewed, it was determined that the CDST was working correctly but there were incorrect ICD-9 codes in the patient’s problem list. The problem lists of ICD-9 codes are generated from billing data, and if any errors are contained, the problem lists must be corrected for the CDST to function properly. In other instances, providers were unaware that the immunization was recommended for certain diagnoses.
Immunization Rates as a Tool for QI
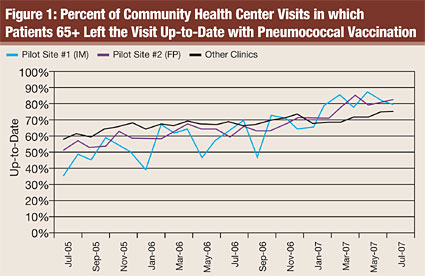
The CCGC/DHHA collaboration included an evaluation component that encouraged the group to monitor immunization rates on an ongoing basis, with these rates fed back to the stakeholders and pilot sites as a central feature for quality improvement. These rates were constructed to be sensitive to monthly changes in practices, so each month the pilot site managers would receive rates sensitive to quality improvement efforts recently implemented, suggesting whether additional barriers to full implementation existed. Additionally, DHHA leadership would also receive these reports and comment with words of encouragement or support for these sites. Though statistical analyses are not performed here, initial data suggest promise for immunization rate improvements. Rates at other clinic sites (roll-out sites) also started to improve most likely due the fact that the CDST became available for use in April 2007 at all sites even though it was not mandatory. There was also more awareness of vaccination due to the informational meeting for practice managers. Figure 1 shows the rates of vaccination among patients seen each month in community health centers.
Discussion
In an integrated healthcare system, consistent use of information technology across all departments that administer immunizations is important to obtain the highest possible rates of vaccination and to avoid over-immunization and time-consuming efforts on the part of providers to find missing documentation.
Some steps of the immunization process must be standardized while others may be flexible. For example, using the clinical decision support tool on every patient at every visit was important, while the exact flow process for administering the immunization and completing the documentation can be more flexible as long as certain steps are always completed in the process.
Using information technology to build clinical decision support tools does have limitations. For example, certain indications or contraindications for immunization will most likely be unavailable in the electronic record or database being used. This means that other steps must be built into a standardized process (such as standard of care for routine screening questions prior to immunization or the addition of questions to elicit information about living conditions that warrant immunization) to identify all conditions or patients that need to be covered by the protocol (or excluded from the protocol).
A clinical decision support tool can be built to be highly sensitive and less specific or very specific but less sensitive. It is important to include clinical expertise on the planning team and to consider who will be utilizing the tool when deciding how sensitive or specific to make the tool. Cost also needs to be considered when creating these tools. For example, due to large increases in adult vaccine administration, the cost to DHHA to supply pneumovax, tetanus, and flu increased sharply.
The CDST will not work on patients that do not yet have a record in the clinical database, i.e. new patients who do not yet have ICD-9 codes entered, or hospitalized patients who have an admission diagnosis that warrants immunization but whose diagnosis has not yet been entered into their problem list.
Conclusion
This quality improvement effort demonstrated a standing-order policy that relies on clinical decision support technology that can be implemented by clinical teams and incorporated into the workflow of medical assistants. Numerous challenges were encountered along the way and overcome. When the CDST was being used for every visit, the immunization rates for that month increased dramatically.
This adult immunization quality improvement initiative borrowed from the lessons learned in improving pediatric immunization, including the importance of designing efficient systems for identifying and tracking immunization status, prompting need for immunization at the point of care, and adopting standing-order policies so that immunizations can be given by non-licensed staff (Centers for Disease Control and Prevention, 2007). Based on our early findings to date, we have demonstrated the successful implementation of this system and increases in adult immunization rates during our pilot period. Based on the success of this project at the pilot sites, DHHA rolled out the intervention to the remaining community health centers and has plans to expand to include the medical sub-specialty clinics as well. This initiative suggests that achieving pronounced improvement in immunization rates requires systems change.
Alicia Appel is an internal medicine physician at DHHA and is an assistant professor of Medicine at University of Colorado Health Sciences Center. She served as the principal investigator at DHHA on this project. She sits on many quality improvement committees at DHHA. She may be contacted at Alicia.Appel@dhha.org.
Carolyn Swenson is a project manager at Colorado Clinical Guidelines Collaborative (CCGC), a nonprofit agency that develops clinical guidelines for primary care providers and implements evidence-based clinical guidelines in primary care settings. She has worked on adult and pediatric immunization projects; adult depression; guideline development (diabetes, depression, obesity, and immunizations), and developing quality performance measures for pediatric health.
Anne Hammer is the nursing clinical coordinator for the Denver Health Immunization Program. She serves as the clinical resource to Denver Health & Hospital Authority staff for immunization information, subject matter expert for the computerized immunization registry, and coordinates outreach immunization projects at local public school sites and county Women, Infants, Children (WIC) sites.
Stephanie Phibbs is a senior professional research assistant at the University of Colorado Denver, Colorado Health Outcomes Program. She has over 12 years of project management experience including extensive work on pediatric immunization projects. Phibbs has co-authored several articles and one book on related health services research interests.
Deborah Main is a professor of family medicine and associate director of the Colorado Health Outcomes Program. She has considerable experience conducting practice-based research to improve the health and health outcomes of poor, underserved populations, with a particular interest in designing and evaluating primary care practice changes interventions.
Moira Sheehan is a senior application analyst at Denver Health. She enjoys working for such a progressive, cutting edge information services department while at the same time remaining in the healthcare arena.
References
Centers for Disease Control and Prevention. (2007). Epidemiology and prevention of vaccine preventable diseases (10th ed.). W. Atkinson, J. Hamborsky, L. McIntyre, & S. Wolfe (Eds.). Washington, DC: Public Health Foundation, 38-41.
Fiebach, N. H., & Viscoli, C. M. (1991). Patient acceptance of influenza vaccination. American Journal of Medicine, 393-400.
Melinkovich, P., Hammer, A., Staudenmaier, A., & Berg, M. Improving pediatric immunization rates in a safety-net delivery system. (2007). Joint Commission Journal on Quality and Patient Safety, 33(4), 205-210.
Kung, H., Hoyert, D. L., Xu, J., & Murphy, S. L. (2008). Deaths: Final data for 2005. National Vital Statistics Reports, 56(10).
Nichol, K. L., & Zimmerman, R. (2001). Generalist and subspecialist physicians’ knowledge, attitudes and practices regarding influenza and pneumococcal vaccinations for elderly and other high-risk patients. Archives of Internal Medicine, 161, 2702-2708.
Santibanez, T. A., Norwalk, M. P., Zimmerman, R. K., et al. (2002). Knowledge and beliefs about influenza, pneumococcal disease, and immunizations among older people. Journal of the American Geriatric Society, 50, 1711-1716.
