Improvement Interventions and the IOM Aims for Quality: STEEP-7
By Shea Polancich, PhD, RN; Terri Poe, DNP, RN; and Rebecca Miltner, PhD, RN
Healthcare organizations should be continuously looking for ways to improve the quality and safety of the care they provide. The current healthcare environment, however, is complex and constantly changing, making the quest for continuous improvement a challenge. In 2001, the Institute of Medicine (IOM) report Crossing the Quality Chasm highlighted the gap that existed between the current and ideal state of the healthcare industry regarding the quality of patient care. This seminal work illuminated the need to provide care to patients with defined aims—namely, that patient care should be all of the following: safe, timely, effective, efficient, equitable, and patient centered. A call to action ensued for providers in the industry to develop strategies for closing the quality chasm in care delivery in accordance with the IOM aims. Now, 15 years later, there are still opportunities to improve the quality and safety of the healthcare delivery system.
The science of safety and improvement has evolved in the past 15 years. Tools and methods for improvement such as microsystem analysis (Nelson, Batalden, Godfrey, & Lazar, 2011; Transforming microsystems, n.d.), the Model for Improvement (n.d.), the Plan-Do-Study-Act cycle for small tests of changes, Lean, and Six Sigma (Langley, Moen, Nolan, Nolan, Norman, & Provost, 2009), have become common terms and practices in the healthcare industry. Tools and methods provide structure for developing, organizing, implementing, and evaluating improvement and safety interventions in clinical environments. The tools used in improvement work should add value to the work, not add complexity to the system. They should provide a simple method for accomplishing a goal.
The purpose of this article is to discuss the development and use of the STEEEP-7 tool for analyzing improvement or safety project interventions with the key focus of assessing them for potential effectiveness in meeting the IOM aims for quality care. The tool also provides a scoring algorithm for evaluating multiple interventions. Similar in form to the Failure Modes and Effects Analysis (FMEA) process (IHI: Failure mode, n.d.; ASQ: Failure mode, n.d.), the STEEEP-7 is a tool designed for improvement and safety operations.
Setting
The setting for this study is the University of Alabama at Birmingham (UAB) Hospital, an academic medical center with 1,157 licensed beds that is the primary trauma and referral center for the state of Alabama.
Methods
This project is a descriptive study based upon observational assessment and convenience sampling. The tool was developed for, initiated, and implemented at an academic organization during the process of facilitating interprofessional clinical team efforts around improvement and patient safety.
Tool evolution
Qualitative STEEEP analysis
During the process of facilitating interprofessional improvement and safety teams, it was discovered that administrative leaders lacked the ability to evaluate improvement interventions within the organization based on the IOM aims for quality. While it was an unwritten goal for improvement and safety interventions to address all of the IOM aims, there was no method to evaluate how an intervention would stack up against each of the six STEEEP goals. With this in mind, the STEEEP concepts were organized and used to evaluate three models for pressure transducer management that were currently being used in the organization.
At UAB Hospital, there was variation in the process of managing pressure transducers for central venous and arterial lines. The variation existed in multiple facets of the process, but one of the key foci of the clinical improvement team was to determine the most appropriate provider type—registered nurse (RN) or anesthesia technician—to set up and manage the pressure transducer in the ICU setting. The clinical team was asked to recommend a provider type for a standardized, organizationwide pressure transducer setup and management process.
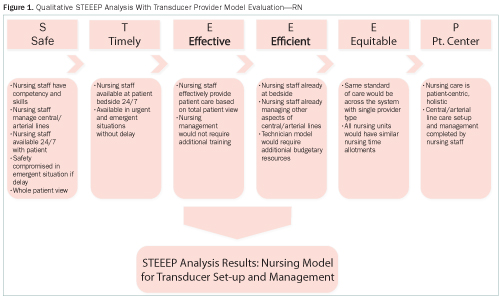
The team faced a dilemma in evaluating the provider type for this process, as there seemed to be valid reasons for using a RN or an anesthesia technician. The facilitator of the group used the STEEEP components and asked the clinical team to evaluate the provider for the process on each of the components. Figure 1 provides the outcome of the clinical team’s evaluation for the RN as the provider using the STEEEP components. Figure 2 provides the evaluation for the anesthesia technician as the provider.
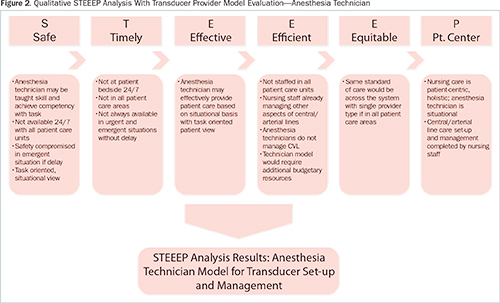
For both provider types, the clinical team used each of the six elements to provide bullet points that supported each IOM goal. The STEEEP tool provided a visual way for the interprofessional clinical team to frame the decision based on the IOM aims for high-quality clinical care.
This transducer example and the STEEEP process were subsequently used with nursing school faculty and graduate-level nursing students to assist in learning concepts related to improvement science. Feedback from this group of individuals was also positive given the tool’s effect in helping evaluate improvement interventions against the IOM aims.
Using the STEEEP components in this fashion showed that there was value in comparing the elements of the IOM aims to improvement interventions. However, the analysis was qualitative, and there was no method built into the process to evaluate multiple interventions and quantify any differences that may exist.
