Improvement in Healthcare Is Possible — Just “Be the Ball”
May / June 2007
Improvement in Healthcare Is Possible — Just “Be the Ball”
It’s no secret that the current system of healthcare in the United States needs improvement. Costs continue to grow; errors persist in treatment; overall dissatisfaction with availability, responsiveness, and hospital-acquired infections climb. While the statistics tell a disheartening story, the stakeholders in today’s healthcare system — payers, providers, and policy makers — are constantly launching major activities to improve this historically complicated and dysfunctional system. But despite all the efforts and good intentions, true systemic change continues to be elusive. Disparate approaches, which can lead to significant local or functional improvements, have done little to address the systemic issues that plague healthcare.
The challenge then is not in the desire to change, nor having the tools to change, or the technology to change or even the incentives to change — it is the lack of a singular, holistic approach to ground healthcare system participants and help organizations that determine who, what, when, where, why, and how the tools, methodologies, and technologies should be applied to deliver significant and sustainable systemic change.
Fortunately there is a simple and intuitive approach, adapted from industry, that can help chart a dramatic course for improvement. By understanding the end-to-end process, or value stream for care delivery, opportunities to apply quality improvement tools, system transparency, measurement systems, and information technology become clearly visible. Without question, the core purpose of any healthcare system are the basic activities required to deliver a particular treatment for a particular condition for a particular patient. The patient value stream, as this is called, provides a sensible, visual, and highly effective approach for systemic diagnosis of the entire stream of actions from diagnosis through reimbursement.
Long utilized in other industries such as manufacturing, value streams focused on the customer (or in this case the patient) are just beginning to be embraced by the healthcare community. Providers, payers, and other participants are gaining new insight into the system and are now able to determine where the most immediate need to apply quality improvement tools such as lean and six sigma rests — where the best opportunity for streamlining the supply chain exists, where bottlenecks and potential failures exist, and areas that have the most to benefit from information technology. This type of insight provides direction for systemic improvement and optimism for the future of care.
As with any new approach, early adopters are realizing that rapid and dramatic improvement is not only possible, but life changing for patients and care givers. By unleashing the creativity of the associates involved in delivering care with a culture focused on the patient value stream, organizations such as Virginia Mason Medical Center, The Cleveland Clinic, and Intermountain Healthcare are realizing double digit improvements in quality, turnaround times, efficiency, and throughput.
The Patient Defines Value
Creating and understanding the patient value stream begins with an understanding of the end-users and how they would define the value delivered by the care delivery process. In industrial companies this is a relatively intuitive task. In healthcare, the end-users or patients are not always sure which course of treatment might yield the most desirable outcome. They certainly know what outcome is desirable, but often need to rely on the expertise of a provider to help determine the roadmap. Thus, to understand value you must have standardized characteristics that can be applied to the patient value stream.
To be “value added” an action must:
- Be something the patient would be willing to do, such as waiting in a treatment room at an ED while results from labs are being processed.

- Transform or change the medical condition. Simply moving from one department to another, whether it is the physical patient, a lab result, or an order for medicine, does not transform anything.

- Be done right the first time. Rescheduling appointments are not value-added actions from a patient perspective.
Studies show that 40% to 50% of all activities required to treat a medical condition add no value from a patient’s perspective. While this is a somewhat humbling statistic, by taking on the perspective of a patient, it is very clear what is not considered value: redundant tests, unnecessary treatments, duplication of information, and long waits to get treatment or consultation. There is no question that a patient relies on the input and recommendations of providers, but the patient also clearly understands what is not considered value.
A simple rule of logic that can be applied when determining value: “If we do this very well, would a patient be willing to pay more for us to do it rather than use another care provider?” If something is wasteful, the answer will almost always be no.
Mapping the Value Stream — Be the Ball
In the movie Caddyshack, Chevy Chase’s character Ty Webb tells his young caddy that to be a great golfer you must “be the ball.” While it’s not often you find wisdom from a fictional golfer, what Ty is trying to say is that you must clearly understand the forces and actions which act on the ball as you play. The same applies to healthcare. To truly improve, an organization must clearly understand all the forces and actions that might impact the delivery of treatment for a specific medical condition. This understanding can be accomplished by creating a patient value stream map.
A patient value stream map captures end-to-end information regarding the current condition of the care delivery system for a particular medical condition. It follows a patient or patient case from diagnosis through reimbursement and includes all actions that take place — both value added and non-value added — as well as the outcomes expected.
When creating a patient value stream map, the goal is to capture all of the activities, errors, interactions, and experiences of all the participants in the system. By following the flow of a patient or patient case from end to end, you can begin to see the opportunities for improvement in the short term as well as the long term, and also see how support processes impact the delivery of care.
The mapping of the patient value stream also provides an opportunity to get representatives from differing functional organizations to view the care delivery system from the same perspective. In many cases, the patient value stream map is the first time a participant has seen the entire treatment cycle a patient follows from end to end. This new perspective provides the added benefits of alignment, communication, and shared vision among a traditionally silo-based system.
It’s About Time
While simply understanding the end-to-end value stream is a significant step forward, it is also important to overcome the typical preponderance of unaligned metrics and create a common dimension for understanding and improving the patient experience. The most effective way to do this is by translating all activities in the value stream to the common dimension of time. Every activity within a value stream can be quantified by time consumption — a defect consumes time to correct, a patient or activity that is waiting for the next step consumes time, room turnover can be measured in time. The common element of time provides a language of improvement that every individual involved can understand.
While certainly there are many more metrics that are important to the patient and other stakeholders within a healthcare system, time is a common element that will help to prioritize opportunities. An example might be when an organization is considering deploying information technology (IT) resources for an enterprise resource planning (ERP) system or for an electronic medical records system. Which should have priority? Both would certainly yield improvement. The answer lies in which one would impact the patient value stream most significantly. Whichever would provide the most significant reduction in end-to-end cycle time and improve the patient experience is the correct use of the IT resources.
Creating the Current State Map
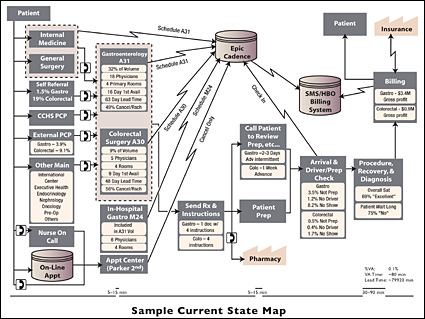
The patient value stream map is a graphic documentation of all activities — both value-adding and wasteful — required to provide treatment for a particular medical condition. The map consists of information flows as well as physical flows of activities to create a closed-loop circuit. The current state map is the visual diagram of the current real process as it is experienced from a patient or patient case perspective — from diagnosis through reimbursement.
To create a current state map, the first step is to form a cross-functional team. Ideally the team is composed of representatives from every functional group in an organization, but at a minimum it should include a multi-functional group of middle managers responsible for implementing change. The team will be tasked with following the patient, or case, from beginning to end and documenting what they actually observe. The goal is to end with a visual representation of every process in the patient and information flows (Figure 1).
![]()
Figure 1. Sample Current State Map
(Click hereto view a larger version in a separate window.)
The next step is to quantify the end-to-end process from the perspective of time. This includes total time from beginning to end, but also a quantification of the value added time — which can be less than one-half of 1% in some processes.
The next step for the patient value stream is to leverage the same cross-functional team that created the map to determine what opportunities exist for improvement. Where should a lean or six sigma project be deployed, and what is the desired state? Should you put effort into the revenue cycle improvement? Should you deploy electronic medical records? The team will clearly see the opportunities after mapping the current state process.
Creating the Future State Map
Once a current state map has been documented and the actions that must be taken are identified, prioritized, and scheduled for action, the same team must create a “visionary map” (future state map) depicting what the future state of the value stream might look like. This map clearly shows the improved state and provides a longer term (minimum 1 year) perspective of the value stream. It can be revisited frequently to validate and confirm direction, be used for communication with the remainder of the value stream participants, and also provide the jumping-off point for future improvement.
Case Study — Colonoscopy Screening Process
A large market, highly regarded healthcare system determined that it would like to employ a value stream approach for improving the screening colonoscopy patient value stream. The organization had recently begun to adopt lean and six sigma improvement tools, but it already had a history of superior care and a legacy of continuous improvement. There was skepticism for the approach, and in many cases the organization’s complexity caused road blocks.
The core team was formed from a cross-functional group of physicians, administrative staff, nursing, financial representatives, and the organization’s continuous improvement team. The team was charged with radically improving patient access to colonoscopy screening as well as improving patient, physician, and staff satisfaction of the process.
The team spent approximately 7 days documenting the performance of screening colonoscopies across five facilities in the system, with more than 45 physicians completing the procedure in various settings and with varying outcomes. The variation in performance discovered included end-to-end cycle time from appointment to outcome from as little as 9 days to more than 69 days. In addition, room utilization was less than 47%, patient satisfaction varied greatly by facility from 36% to 70%, and process variation included more than 37 different pre-procedure instructions.
Following the completion of the current state map, the team conducted a 1-day “visioning event” where the current state map was reviewed, opportunities were identified, prioritized, and assigned, and a future state map was created.
Over the course of the next 60 days, the team implemented a variety of actions including two collaborative problem-solving kaizen breakthrough events to improve process flow and standardization and implementation of a new scheduling procedure that included an electronic dashboard for tracking availability. As a result of the actions taken, the team delivered outcomes of:
- 30% increase in procedures per hour.

- First appointment availability reduced to less than 9 days.

- Room utilization increased by 5%.
This same organization is now achieving exceptional results by leveraging the same approach to improve operating room efficiency and throughput, revenue cycle, and call center performance.
Imagine the Potential
There is no question there are challenges to improving the American healthcare delivery system. But with the application of tools from industry, including patient value stream maps, there is ample expertise to achieve unprecedented transformation in a system that has a history of being difficult to change. A Toyota executive once stated: “We obtain brilliant results from average people operating brilliant processes. But we observe that most companies obtain mediocre or worse results from brilliant people working around broken processes.”
Imagine the potential of brilliant people operating brilliant medical processes.
Co-founder, president, and chief executive officer of Guidon Performance Solutions, Ron Wince has nearly two decades of experience leading performance improvement and cultural transformations within manufacturing, service, and government organizations.
Prior to founding Guidon, Wince led an internal consulting group for Bank One and later at JP Morgan Chase. During his tenure, he led the introduction of LeanSigma® within payment operations, check processing, and financial reporting, as well as in various consumer lending, treasury services, and information technology functions. His pioneering work implementing LeanSigma, GE performance management techniques, and lean information technology in service industry environments is the foundation of Guidon’s Execution Model, which helps clients realize desired, sustainable results. Wince can be reached at rwince@guidonps.com.
