How a Captive Insurer Uses Data and Incentives to Advance Patient Safety
November / December 2009
![]()
How a Captive Insurer Uses Data and Incentives to Advance Patient Safety
The Institute of Medicine (IOM) report (2000), To Err Is Human, unveiled a truth about the U.S. healthcare system that was previously either obscure or unrecognized: we have a “non-system” of care with a relatively high frequency of errors. The high defect rate leads to the death of thousands of people each year from preventable errors — more individuals than die from motor vehicle accidents, breast cancer, or AIDS (Kohn, 2000). In the decade since publication of the IOM report, improved patient safety has become a major focus of attention of consumers, healthcare providers, governmental and private insurers, employers, and non-governmental organizations dedicated to healthcare improvement. Indeed, the 2009 update for the National Quality Forum’s “Safe Practices for Better Healthcare” includes as its fourth practice statement: “Healthcare organizations must systematically identify and mitigate patient safety risks and hazards with an integrated approach in order to continuously drive down preventable patient harm” (National Quality Forum, 2009).
Better understanding of the causes of preventable error has focused attention on the need to address the systemic problems that allow errors to remain undetected prior to patient injury. Many sources of data indicate that a high proportion of preventable errors relate to defects in systemic rather than individual performance. For example, a review of 10 years of closed malpractice claims found that more than 40% of obstetrical cases related to problems in teamwork and communication (CRICO/RMF internal data).
However, implementing and sustaining improvements in systemic processes such as teamwork and communication can be challenging. Such improvements often require a shift in organizational culture, changes in practice at the front lines of care, and reorganization of the systemic infrastructure of the organization — to provide electronic health records, reminder systems, decision support, and improved handoffs, for example. Leaders of quality efforts at healthcare organizations may struggle to get the attention and necessary buy-in of the busy clinicians whose actions are critical to patient safety efforts. They may grapple with the question of how to successfully implement and maintain a patient safety initiative.
Medical malpractice insurers not only defend the claims brought against the providers they insure, they also seek to prevent claims in the first place. The incentive to prevent claims is especially obvious for captive insurers — insurance providers that are owned by the institutions they protect. Every claim avoided represents both an avoided tragic event and avoided costly claim, helping to maintain the captive’s financial stability and support its owner institutions. For these reasons, captive insurers have every reason to support patient safety initiatives.
However, the staff of malpractice carriers is not at the front lines of care, doesn’t control the promotions or salaries of frontline providers, and is rarely in a position to mandate patient safety interventions, even if they are based on proven best practices. Instead, carriers must find other means for promoting patient safety efforts. This article will highlight the efforts of one captive insurer to promote patient safety while at arms’ length from the frontline providers. It also will show how the strategies used by the group are applicable to non-insurance organizations that need to bolster or maximize their patient safety practices.
A Patient Safety Mission
CRICO/RMF is the patient safety and medical malpractice company owned by and serving the Harvard-affiliated hospitals and healthcare organizations. The Controlled Risk Insurance Company, LTD (CRICO), the malpractice insurance arm of the company, was established in 1976 when commercial carriers stopped issuing malpractice coverage in Massachusetts. Risk Management Foundation (RMF) was incorporated three years later by the Harvard Medical Institutions as a charitable, medical, and educational membership organization. Together, CRICO/RMF provides malpractice coverage and evidence-based risk management to nearly 11,440 physicians, 20 hospitals, and more than 200 other Harvard-affiliated healthcare organizations.
During the first decade of its existence, CRICO/RMF applied a risk management approach that was traditional for the time, with a reactive strategy that involved mitigating and avoiding events similar to ones that had already occurred. Coincident with the release of the 1999 IOM report, leaders of the organization shifted to a patient safety focus. According to CRICO/RMF President Jack Mc Carthy, “We started looking at claims as being a problem with the system or a lack of system. We opened up a dialogue with physicians to say, ‘Look, you are on the receiving end of a bad system.’ It was a liberating concept that took a lot of the guilt away and led people to start thinking of how to improve.” Chief Medical Officer Luke Sato, MD, concurs. “When I joined CRICO/RMF in the late 1990s, my initial goal was to help physicians see the patient’s perspective so they could begin to understand that many errors are related to systems breakdowns. Presenting physicians with real-life, detailed patient information from depositions, case descriptions, and claims data is a very effective tool for engaging them in patient safety work.” The IOM report provided the malpractice carrier with a unifying concept that opened the door for dialogue with physician leaders about specific patient safety interventions.
With the shift in approach, CRICO/RMF staff needed to understand clinical processes to a level of detail previously unnecessary — a task that required convening healthcare providers. After all, if you want to encourage practices that promote patient safety, you need to fully understand those practices. According to Robert Hanscom, JD, vice president of Loss Prevention and Patient Safety at CRICO/RMF, “After the first IOM report in 1999, we saw that our data could be powerful for the proactive version of risk management, which is not only understanding what happened in the past, but in a proactive, predictive way, developing methods to point people to the fact that if they don’t implement certain interventions in a particular arena, it is likely they’ll see similar kinds of claims. Even more importantly, they’re going to have human tragedy. And by avoiding the tragedy, you will hopefully avoid the malpractice cases.”
Robert DeVore, senior vice president of Strategy and Special Projects, was brought in to CRICO/RMF for his business acumen — he had no experience dealing with malpractice insurance or medical error. As he recalls, he said to the senior vice president of loss prevention at the time, “Let me just ask a dumb business question. What are the top three to five errors that cause the vast majority of harm to patients and indemnity payouts?” Surprisingly, the organization had not analyzed the data on errors to uncover such trends. Within a month, CRICO/RMF had invested in the necessary software, and analysts had culled the claims data. Leaders learned that the four areas associated with highest risk of claims — obstetrics, surgery, missed and delayed diagnosis, and medication error — identified 91% of the indemnity payouts and 67% of harm. Following DeVore’s lead, organizational leaders developed business plans for the four target areas and reorganized loss prevention activities to focus strictly on these targets. “If a proposed project didn’t fall within one of those four buckets, there had to be a really good reason to pursue it,” DeVore notes.
This reorganization allowed staff to prioritize patient safety efforts based on the clinical areas associated with the most frequent and highest severity losses. Because CRICO/RMF retains its claims, loss prevention, and analytical activities in-house rather than outsourcing these services, it maintains a high degree of control over data collection, coding, and analysis. Data from every claim is coded with a high degree of specificity, which provides clinically relevant information that healthcare providers can use to plan specific interventions. The organization now has 33 years’ worth of data on malpractice cases that have been analyzed to a high level of detail, providing a wealth of information for identifying areas of potential liability and planning relevant interventions.
The organization founded RMF Strategies in 1998, to create a national database of clinically-coded data on practice claims. CRICO/RMF board members had frequently requested comparative information, eager to learn how the loss profile of Harvard-affiliated hospitals measured up to those of outside healthcare organizations. A department of CRICO/RMF, RMF Strategies provides database software with analytic capabilities and consulting services to external healthcare organizations. Consultants apply the same approach to external clients as the Harvard affiliates, thus allowing for expansion of the comparative database and cross-community reciprocal learning opportunities.
The governance structure of CRICO/RMF has been essential for promoting patient safety initiatives. Many members of the organization’s board of directors are trustees, executives, and senior physicians of the Harvard-affiliated hospitals that own the captive. These individuals serve as translators of a sort, providing CRICO/RMF with valuable insight about the specific needs of healthcare providers and about the particular culture in their individual institution while helping providers identify CRICO/RMF tools and services to support their patient safety efforts.
Overall Strategy
CRICO/RMF leaders have applied an intentional, deliberate strategy for promoting patient safety efforts: putting the right data in front of the right people, letting them identify gaps and forge solutions, and supporting those solutions, where possible, with financial incentives. To achieve success with this strategy, members of the loss prevention/patient safety department at CRICO/RMF strive to build relationships with providers and administrators at each owner institution through face-to-face meetings and by convening working groups of providers and administrators. The staff then presents highly specific, actionable data to clinical leaders and providers and allows these individuals to discuss gaps in processes and potential risks. Rather than mandating specific patient safety initiatives, the CRICO/RMF staff focuses on fostering working conversations among administrators and providers, so that these individuals can identify solutions likely to be successful at the frontlines of care. For example, CRICO/RMF staff convened a series of meetings over a 12-month period of the chiefs of surgery of all the Harvard-affiliated institutions. CRICO/RMF staff presented highly detailed claims data and asked participants to confirm the identified vulnerabilities. The data provided sufficiently specific information for the surgery leaders to return to their institutions and begin to craft solutions to address those gaps. According to Ann Louise Puopolo, director of loss prevention and patient safety, “Our position is that we want to help people to do the right thing, but we’re not in the business of mandates. What we’d like to be is a lever for change. We’d like to be able to use the data, the educational content, and the impact from the educational content to make the business case to the chiefs of service or hospital-based leadership, that these educational core components should become a term of credentialing. That’s where we’d like to see the tipping point.”
Being able to provide highly specific data to administrators and providers is a significant boon to engaging them in creating and sustaining solutions. Because CRICO/RMF maintains centralized, in-house data collection services, claims data are coded according to a common language and taxonomy, providing a robust body of evidence regarding specific areas of vulnerability within a practice, institution, or group of institutions. Using the claims database, CRICO/RMF staff can show, for example, that a hospital’s obstetrics department has a relatively high rate of shoulder dystocia claims that involved communication gaps between residents and attending physicians. On a more global level, the organization can identify the locations within clinical processes where gaps are most likely, stating, for example, that across the Harvard system 61% of the dollar losses associated with outpatient diagnosis-related claims involved problems with the ordering of diagnostic tests.
The organizational leaders at CRICO/RMF also recognize that each Harvard-affiliated institution has a unique culture and that the most effective approach for implementing sustainable patient safety interventions will vary from one institution to another. When working with hospital administrators and providers to encourage the adoption and spread of patient safety practices, CRICO/RMF staff tries to remain cognizant of the existing culture. According to Kenneth Sands, MD, senior vice president of health care quality at Beth Israel Deaconess Medical Center in Boston, CRICO/RMF staff provides “customized initiatives, which create uniquely valuable offerings because they’re not ‘cookie cutter.’”
Clients of RMF Strategies also have benefited from the CRICO/RMF approach of “leading with the data.” Larry Smith, vice president of risk management of MedStar Health, a health system and captive insurer in the Maryland-D.C. area, says his organization created an obstetrics risk reduction task force, provided task force members with data that had been collected and analyzed using the claims management software developed by RMF Strategies, and let the group determine potential solutions. “In the last eight years, this obstetrics program has been one of the most visible patient safety-risk reduction initiatives across the system. The obstetricians are envied by many of the physicians elsewhere in the hospital system because they have come together as a collective group, have a system-wide identity as a group, and have become patient safety experts in their own right… It has transformed the way our obstetrics department looks at patient safety.” Smith says that patient outcomes, such as cesarean section rates and APGAR scores have improved due to the risk reduction program. In addition, since the intervention, the obstetrics-related claims rate remains lower than anticipated based on previous experience.
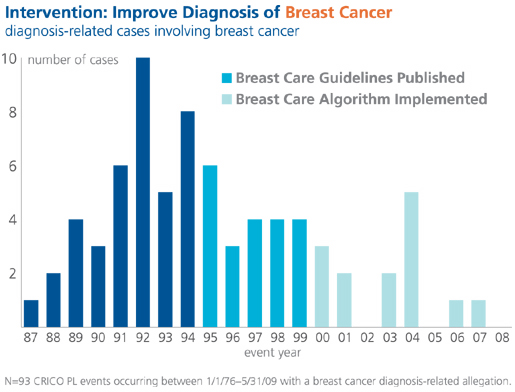
CRICO/RMF staff crafts a variety of risk reduction tools based on needs identified through claims data to help providers identify and mitigate gaps in care processes that increase the risk of an error. For example, data analysts at CRICO/RMF identified an increase in claims related to failure to diagnose in the ambulatory setting. One area of specific need that emerged was breast cancer diagnosis. CRICO/RMF staff worked with clinical experts to develop decision support tools for the diagnosis of breast cancer. One tool, the Breast Care Management Algorithm, is used to remind providers of potential pitfalls in diagnosis, such as failure to create a system for tracking ordered tests and outside referrals to ensure notification of test results and referral outcomes. Work on the algorithm began in the early 1990s, when CRICO-insured primary care providers expressed concern over the frequency of malpractice claims alleging a failure to diagnose breast cancer. The first iteration was published in 1995; the document has been revised four times, culminating in the most recent (2009) edition. (View the algorithm at http://www.rmf.harvard.edu/files/documents/cricormf_bca.pdf.)
Many CRICO-insured hospitals have embedded the algorithm in their electronic decision support systems. The Breast Care Management Algorithm, along with other breast cancer care initiatives, has resulted in a reduction in cases asserted, as shown in Figure 1.
Incentives to Support Patient Safety Initiatives
In addition to providing the right people with the right information, incentive programs have been a key strategy that CRICO/RMF leaders have used to support patient safety initiatives. The organization reinvests 5% to 7% of collected premiums, a total investment of more than $6 million, into two types of incentive programs: premium discounts and patient safety grants. The premium discount program involves the return of a portion of the paid premium to the institution upon completion of a specified risk reduction activity. CRICO/RMF staff has no control over where the funding from premium discounts is spent. Funds are returned to the same financial department that paid the premium, and departmental leaders determine how the funds will be allocated. With patient safety grants, CRICO/RMF staff maintains more control over where funds are reinvested. CRICO/RMF awards patient safety grants to specific practices or hospitals to foster systemic or environmental change, such as improved management of specialist referrals. CRICO/RMF leadership has the discretion to stipulate which individuals or practices receive the funding. As CRICO/RMF leaders design specific grant programs to target systemic or individual change, they take into consideration the specific risk-related behaviors they hope to influence with the incentive.
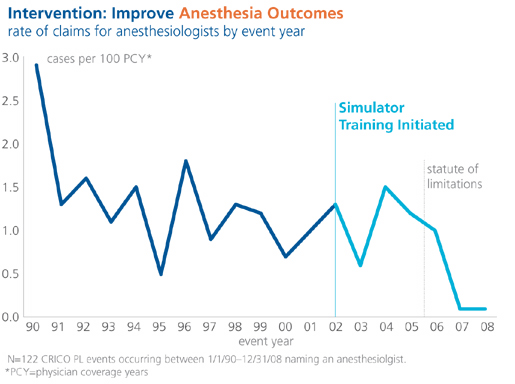
The CRICO/RMF anesthesia simulation training and the obstetrics team training are incentive programs that have successfully improved patient safety, as evidenced by a drop in claims for both departments. Initiated in 2001, the anesthesia simulation training was the first CRICO/RMF incentive program. Hospitals or anesthesia practices receive $500 per physician when their anesthesiologists complete the individual-based simulation training. The mannequin-based exercises run learners through simulated scenarios based on actual cases that led to prior claims. Learners can make — and learn from — mistakes without risk to patients. The training also can be carried out as a team exercise, providing valuable teamwork and communication experience.
Initially, the anesthesia simulation training was voluntary. However, after about seven years, actuarial data showed that the risk of a claim was 24% lower for simulation-trained anesthesiologists than for those who had opted out (see Figure 2). In fact, the actuarial data indicated that the anesthesiologists who had participated in the simulation had achieved a totally different risk class. These data prompted leaders of the Harvard-affiliated academic hospitals to make the training a requirement for certification. CRICO/RMF leaders responded by requiring the training for malpractice coverage as well. This sort of iterative process in which CRICO/RMF patient safety staff works collaboratively with administrators of the owner hospitals is ideal for achieving patient safety improvements, according to Sato. “We can use data to shift priorities, as long as we have a liaison to the insured organization.”
The CRICO/RMF obstetrics team training initiative was launched in 2003. Whereas the anesthesia simulation program is completed by either individuals or teams, the obstetrics training is solely team-based, reflecting the need for communication and teamwork in difficult delivery situations. The participating team, which is composed of obstetricians, obstetrical nurses, and obstetrical anesthesiologists, participates in an experiential six-hour program held in a realistic medical setting that is equipped with the supplies and devices normally found in a labor and delivery unit. The team participates in simulated clinical scenarios based on prior obstetrical claims, using a computerized mannequin and fetal heart rate simulator. After the simulation, trained instructors review videotapes of the activities with participants in structured group debriefings.
In addition to completing team training, participants are required to pass a written test on obstetrical practice guidelines and complete online courses on electronic fetal monitoring and management of shoulder dystocia. Participating hospitals are required to offer providers the opportunity to practice safety drills on site. Both the total number of obstetrical claims and the number of claims for high-severity events have dropped across the Harvard system since the training began. During the four-year period prior to the training, there were a total of 53 obstetrics-related claims across the system associated with a cost of $62.6 million. During the four-year period after the training, there were just 31 obstetrics-related cases; these cases were associated with a cost of $44.7 million. According to Anthony D. Whittemore, MD, chief medical officer at Brigham and Women’s Hospital in Boston, the fact that simulation training has reduced obstetric claims makes sense, “The obstetrician who finished training 30 years ago is probably not up on facing shoulder dystocia or complicated deliveries, because of the emerging technology and the fact that they just haven’t had to face these situations very often at all. For any low-frequency event, simulation is very, very useful.”
The simulation training also has been effectively applied at community hospitals. Mitchell S. Rein, MD, chief medical officer and senior vice president of medical affairs at North Shore Medical Center in Salem, Massachusetts, notes that the program was “Hugely successful. We’re still applying some of the lessons that we learned from the initiative to other areas such as the operating rooms and our hospitalist program. Obstetrics is a multidisciplinary effort, and the simulation and teamwork training lends itself to improving a variety of the human factors in healthcare.”
According to one survey, the majority of participants of the simulation program reported having experienced a critical clinical event since taking the course and that aspects of teamwork had either significantly or somewhat improved due to the training (Gardner, 2008). Additionally, 90% stated they had responded better to critical events, and 87% reported that they communicated more effectively during the most significant critical event that occurred since taking the course.
The obstetrics team training premium discount program offers a savings of 10% for each insured physician or nurse midwife. Over the five years of the program’s existence, CRICO/RMF has refunded more than $5 million back to participating practices and hospitals.
|
|
|
Translating the CRICO/RMF Strategy to Healthcare Organizations
Despite the disadvantage of having weaker leverage points for shifting practice patterns than entities that control salaries and credentialing, CRICO/RMF staff has engaged providers in successful patient safety initiatives. The strategies that CRICO/RMF leaders used to create and sustain these initiatives can also be applied by healthcare executives and patient safety champions to plan, implement, and sustain patient safety efforts. The overall strategy used by CRICO/RMF leaders and staff is to “lead with the data.” Their goal is to collect and present consistent, accurate, actionable data that are sufficiently detailed to inspire behavior change and action supportive of patient safety. Presenting the data to individuals capable of the changes needed to improve patient safety requires the development of relationships at all levels of the organization. Finally, use of incentives often is necessary for capturing the attention of busy clinicians and encouraging them to prioritize time, energy, and thought for a new patient-related activity. (See sidebar for six specific tips for patient safety initiatives.)
Conclusion
Patient safety is a top priority to many constituents and organizations today. The CRICO/RMF strategy for promoting patient safety initiatives in its owner hospitals is to build key relationships with leaders and providers, present detailed, actionable data, and provide financial incentives, with the end goal of shifting providers toward practices that reduce the risk of error. Premium incentive programs based on simulation training are examples of a specific tool that CRICO/RMF leaders have successfully utilized to promote patient safety at Harvard-affiliated organizations. Leaders of healthcare organizations and patient safety champions can apply similar approaches for implementing patient safety initiatives at their organizations.
References
