Health Information Network – Just What the Doctor Ordered: Using an HIN to Improve Care
January / February 2006
![]()
Health Information Network
Just What the Doctor Ordered: Using an HIN to Improve Care
According to a report released in 2005 by the Centers for Disease Control (CDC), less than one third of the nation’s hospital emergency and outpatient departments use electronic medical records. While computerization of information across all sectors of our economy has spread like wildfire, healthcare lags behind. Billing processes were first to come into the information age and are now used in the majority of physician offices. Clinical records, however, are another story.
In an effort to catapult medical record keeping into the 21st century, President Bush outlined a plan in 2004 to ensure that within 10 years, most Americans would have electronic health records. That plan, along with increased quality reporting requirements and public demand for accountability of patient safety, is driving the push for widespread adoption of electronic health records.
A special task force has been assembled at the Department of Health and Human Services to spearhead the initiative and develop a “medical Internet” that would facilitate confidential transmission of medical records across the country — a system the president correctly credits with the ability to save money and lives.
How will that play out over the long term? And, what can be done to achieve such goals in the short term? Converting paper records to computer records, as evidenced by the experience of the administrators, physicians, and other clinicians at Middlesex Hospital in Middletown, Connecticut, has been delivered by an award-winning electronic central database that has proven invaluable to patient care and quality improvements.
Part of Middlesex Health System, Inc., Middlesex Hospital is a not-for-profit, patient-focused health network where state-of-the-art technology is combined with an uncommon level of personal concern for patients and families. For more than 100 years, our resources have been focused entirely on the health needs and priorities of the residents of the communities in Greater Middlesex County. We cultivate an environment of excellence and maintain high levels of patient satisfaction based on the quantity and quality of caregiver time at the patient bedside. Middlesex Hospital operates more than 30 inpatient, outpatient, primary care, and emergency facilities throughout Greater Middlesex County. We have nearly 300 active physicians on our medical staff representing every major specialty.
Today, Middlesex is leading the way with its early implementation of a central database that not only demonstrates but also fulfills the need to have in place electronic records that capture clinical data — tests administered, results received, services provided, observations documented, etc. — in order to report outcomes data required for quality of care improvements. Further, Middlesex Hospital physicians can access the database from any computer at any time.
What began back in 1995 as a repository for lab results only is now a comprehensive Web-based database accessible by hospital physicians via any computer with Internet access. As an easily-navigable electronic warehouse for a patient’s medical records from hospital admission to discharge, the database of inpatient records — including dictated reports, medication profiles, written radiology reports and images, emergency department reports, cardiology reports, and EKG strips, and more than 500,000 pages of patient medical records scanned annually — has become an invaluable asset for clinicians.
So what does it mean for patient safety and quality healthcare? Physicians are practicing more efficiently and maximizing their time with patients. The hospital can take a prospective (rather than retrospective) approach to building processes that result in the delivery of safe and evidence-based care. Duplication of tests has been eliminated. A more reliable method of medication reconciliation and “drug rules” help avoid dangerous combinations of medicines on multiple levels. A patient or family member phoning to express concerns about specific treatment or billing can receive immediate assistance.
Additional improvements to the system are in the pipeline. The clinical repository is slated for an upgrade. Medical rules (i.e., aspirin before heart attack) will be written to achieve better patient outcomes. Outpatient information will be merged to reduce the lack of communication between the various settings where patients receive care. And, a pharmacy interface will further enhance medication reconciliation — with the ultimate goal being the creation of a running log of prescriptions for all patients.
How It All Began
During the Clinton healthcare era, one of three major initiatives at the hospital was information systems support, including setting up a database for lab results.
In late 1997, just more than 50% of Middlesex Health System’s revenue was coming from outpatient services, and physicians who referred most of their ancillary services to the health system were requesting increased efficiency and better service. They wanted immediate access to clinically relevant information, as well as the ability to store information for the life of a patient and easily distribute it to other caregivers and specialists. To meet those objectives, we set out to further develop our clinical data repository, which was still in its infancy, into a true health information network (HIN) that could facilitate the creation, distribution, storage, and utilization of the clinical information cost effectively while improving physician satisfaction, increasing volume, and improving quality.
We built and deployed a physician Web portal with a clinical data repository (CDR). While our initial investment of $150,000 was fairly small, the HIN has quickly become our most utilized computer system — the most significant asset we have. Most hospitals have a CDR of sorts. What makes ours interesting is that it grows by four to eight million lab tests per year (with an outpatient average of five tests per registered patient). It currently holds more than 40 million clinical results collected over 10 years on 325,000 different patients; the population of our primary service area is 275,000. The average patient has 107 different results in the system and 8 different caregivers from emergency department physicians to nurses to primary care physicians.
![]()
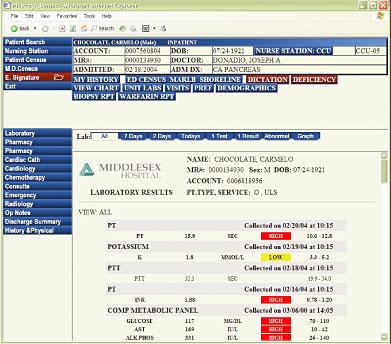
Figure 1. In many respects the most important asset of the central database system, the clinical data repository or Results System, has changed the way Middlesex Hospital physicians practice medicine.
How Far It’s Come
Today the HIN is a comprehensive Web-based database accessible by hospital physicians via computer from anywhere. Its 2,900 users — 1,200 who are outside the hospital itself — sign in through a Web browser and can access the network from any computer. Every day, clinicians retrieve pieces of information about 3,200 different patients. The HIN has become an invaluable asset for clinicians as it provides them with an electronic record from a patient’s admission to discharge including all inpatient records such as dictated reports, medication profiles, radiology results (written reports and images), emergency department reports, and cardiology reports (including EKG strips).
“I don’t know how I could function without it — honestly,” says Jesse Wagner, MD, Middlesex Hospital hospitalist. “I could spend an hour doing what takes me one minute with the system versus paperwork. I can look at trends over time, i.e. blood counts; compare EKGs. I used to have to go down six floors to see an x-ray; now I can just pull it up on the screen. Patient care is better because of it. Tests can be followed up on easily.”
The HIN has changed the way our physicians practice medicine; they can get a profile on a patient before even seeing that patient. When a specialist such as a cardiologist enters the circuit of patient care following multiple tests, he can access information about which doctors have seen the patient, what tests have been administered, and what the results show, as well as what medications have been prescribed. In the past, when doctors did not have this complete history at their fingertips, they would either redo a test or work toward a diagnosis without full knowledge.
“As a primary care physician I have to review historical trends in lab results, radiological images, and screening tests many times per day,” says Alan B. Douglass, MD, FAAFP, Middlesex Hospital family physician. “Before the HIN I would have to wade through large and often incomplete stacks of paper reports or hand-transcribe flow sheets. If another doctor in the system ordered a test, I would often not even know it was done. Now in just a few clicks I know exactly what was done by any doctor affiliated with the health system, when it was done, and what the results were, and can trend or graph individual lab values. It is an immense time saver and substantially increases the quality of care.”
Increased Efficiency and Improved Patient Care
Thanks to development and implementation of the HIN, we can now offer our physicians the ability to practice medicine more efficiently and maximize their time with patients. They can review patient profiles before physically visiting a patient (e.g., when a specialist enters into the process, he can see the entire series of events, lab results, etc. since the patient’s admission to the hospital).
By virtue of the fact that a physician can look up a patient in the HIN and see exactly what the patient’s care has encompassed throughout any hospital admission period or longer, fewer diagnostic tests are duplicated, which translates into cost-effective healthcare and greater patient convenience and continuity of care.
Currently, we have inpatient drug rules in place, including a system of alerts to identify dangerous combinations of medications and other medications, foods, known allergies, diseases, and specific lab results. Recognizing that medication reconciliation is a national problem, we’re enhancing our HIN to move beyond checking for drug interactions on an inpatient basis and include computerized physician order entry (CPOE) in the office setting. In addition, we are working toward being able to collect prior medications using nursing assessment upon presentation in the emergency department, for example. Our goal is to enhance the HIN so it can be used to create a running log through which a patient’s entire drug history from pre-admission to discharge can be illustrated. By doing so, the chance of physician error decreases, and we are able to share a patient’s complete pharmaceutical history with all professionals — pharmacies, convalescent homes, and others — who care for the patient once she leaves the hospital.
In addition, the HIN allows the hospital to take a prospective approach to building processes. The technology is a very sophisticated system that allows us to study and aggressively identify the root of any problem and attack it. Administrators have the ability to run real-time reports and enact immediate course correction measures if needed instead of waiting 3 to 6 months for results and risking development of a larger problem. For example, we can pull a report that tracks heart attack patients over the last 30 days: how many died, how many received aspirin upon presentation at the hospital, how many received beta blockers, etc.
We also have the ability to respond immediately to a phone call from a patient with concerns about treatment or billing. We can field the “complaint” efficiently in real time, rather than make him wait 5 days while we research the history of the patient’s hospital stay and investigate the situation.
Further, the HIN has been a tremendous asset in quality and safety improvements. We’ve created lab registries for all physicians so that with appropriate disease management we can identify patients who need medical attention, as well as special services such as counseling. For example, the lab registry for diabetes shows doctors which of their patients have diabetic results. A physician may realize he hasn’t seen a patient for several months, notice that the patient’s counts aren’t right, and call the patient in for a check up.
We’ve developed a list of critical test results that need to be communicated to and acted upon by a physician within 15 minutes. Those results are flagged, and the doctor is called. The HIN tracks timing from when that test result is available to when the physician receives and reads the result back to the clinician.
Healthcare is too crucial to simply implement a process and hope it works. Many hospitals continue to utilize a retrospective approach and wait six months to realize problems that require immediate attention. Our technology allows us to course correct as early as the following morning when necessary.
What’s Next?
One of the beauties of our HIN is that the possibilities are endless. Right now, we’re working to upgrade our clinical repository — we want it as comprehensive as possible when we implement CPOE. It’s our goal to create electronic health records by merging outpatient settings such as doctors’ offices with patients’ records in the existing HIN. By merging outpatient information, we can improve communication between the various settings where patients receive medical care.
In addition, we need to compose further medical rules to achieve better outcomes. And, we’re in the process of converting our ordering process for labs and ancillary services. By March 2006, we hope to have incorporated and automated a significant amount of nursing information into the HIN. We’re also enhancing medication reconciliation by creating a pharmacy interface to achieve our ultimate goal of maintaining a running log of prescription for all patients.
Medical records need to be available to all physicians anytime and anywhere. Regardless of the federal government’s commitment to bringing our industry online in the next 9 years, the establishment of electronic medical records should be at the top of every hospital CIO’s agenda. It isn’t worth the wait when the utilization of electronic medical records has been proven to prevent errors and duplication of tests, enforce standards, increase efficiency, simplify record keeping, and improve overall patient care. The mission of Middlesex Health System is to improve the health of the people and communities we serve and to manage illness with skill and compassion. Building our own fully integrated electronic medical record for patients has been an enormous undertaking, but one that furthers that mission and continually yields clear and precious short- and long-term benefits for our providers and patients.
|
Lud Johnson (lud_johnson@midhosp.org) has served as vice president of information services and chief information officer at Middlesex Health System, Inc. since 1990. He has over 30 years of experience in finance, information, and telecommunications systems management, including strategic planning and implementation activities. Johnson is also president of Company 1 Consulting, a firm that provides IS leadership management and support to the healthcare industry. In addition to Middlesex Hospital, Johnson is actively involved in the management of St. Vincent Medical Center in Bridgeport, Connecticut, and Lowell General Hospital in Lowell, Massachusetts, and other industry initiatives. Johnson received a bachelor of arts degree in business administration from Northeastern University and a master of science degree in management from Rensselaer Polytechnic Institute.
References
Burt, C. W., & Hing, E. (2005). Use of computerized clinical support systems in medical settings: United States, 2001-3. Advance data from vital and health statistics; no. 353. Hyattsville, MD: National Center for Health Statistics.
