Health Competencies: Beyond the Biomedical
How knowledge, skills, and attributes improve the effectiveness of results
By Cristina Vaz de Almeida
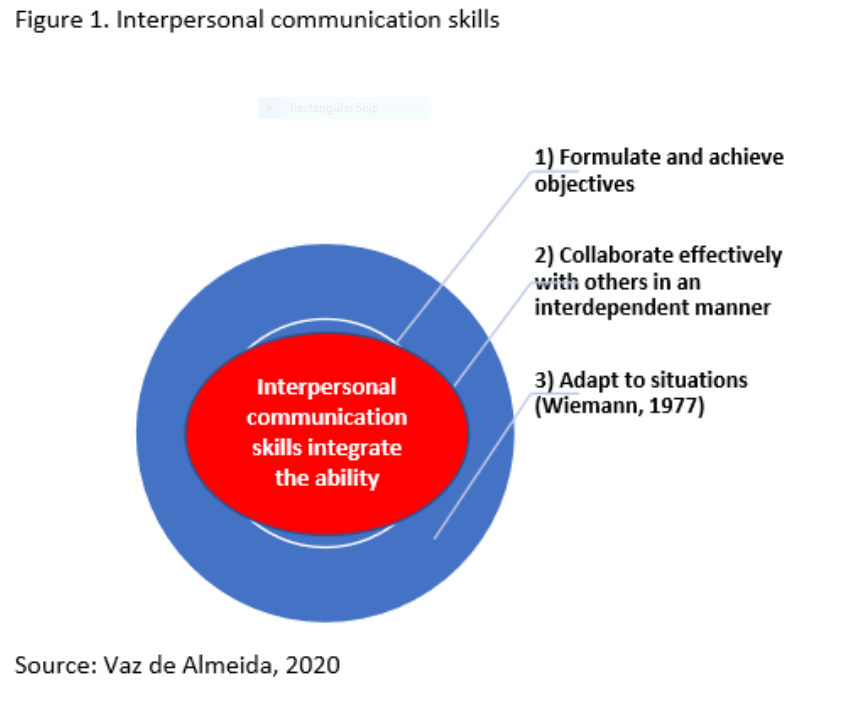
Dealing effectively with human relationships (Moscovici, 1981) through adaptation to situational needs and demands (Wiemann, 1977) is a permanent challenge, and particularly in healthcare, it requires a Herculean effort from health professionals.
In this context, competence is an important factor in the way individuals help shape the world, not just in how they deal with it (OECD, 2005). And in healthcare, it is the competencies that improve the effectiveness of health results.
According to a qualitative study of health professionals organized in 14 focus groups in Portugal between July and November 2018: “Health professionals are transformers. We manage to transform people’s lives, and so we have a huge responsibility.”
In the domain of information exchanged in the health relationship, it is necessary to “know how to question” (Hargie, 2011), with the communicative competencies central in the interaction between professional and patient, such as:
1) Asking questions
2) Providing information and encouraging the patient to express concerns or report symptoms clearly and completely
3) Verifying that the information received is understood, which implies clarifying issues, increasing understanding, and remembering the information (Cegala, 2003).
“Competence” is described in the literature as a multidimensional construct (Flynn, 2014) in which communication skills are also integrated, based on the functionality of communication, adequacy, and sufficient knowledge, judgment, and skills (Light & McNaughton, 2014).
Communicative competence allows individuals to function effectively in society using language and non-linguistic behavior (Wiemann & Backlund, 1980).
Skills: Healthcare professionals must be holistic
Thus, competence means using knowledge, skills, and attributes to act in society. And the more complex the society is, the more demands are placed on health professionals. Adopting a holistic view makes the health professional a “transformative” human being, as many health professionals said during an investigation carried out in Portuguese hospitals in 2019 by the author (Vaz de Almeida, C. (2019).
Within the biomedical model, health professionals are probably among the most careful professionals in our society (Leape, 1994). They are not supposed to make mistakes, to have unforeseen events, or to be exhausted and worried; there is a strong emphasis on perfection, whether in diagnosis or treatment (Leape, 1994). In this demand for perfection, centrality operates through the health professional’s power over the patient in a relationship between the expert and the layperson.
An improvement in professional-patient communication will increase patient compliance, assuming that adherence depends on the patient’s literacy and the professional’s communication skills (Leonard, Graham, & Bonacum, 2004).
The OECD (2005) stresses that key competencies are determined by the goals of individuals and society and must relate to the main resources and requirements in life. Thus, individuals’ personal qualities and cognitive skills cannot be determined only by arbitrary decisions (OECD, 2005).
Individuals with interpersonal competence have an open (available) posture to receive messages from other people, do not cause anxiety in others (Wiemann, 1977), and are empathetic, affective, supportive, and calm while interacting. They adapt their behavior to situations within an encounter and change as they move between encounters.
Competence is thus a combination of skills, knowledge, and personal attributes that leads to superior performance (Tench & Konczos, 2013).
In professional-patient interaction, different skills (acquired and learned) are used (Hulsman, 2009), which allow continuity of care and include clinical and communicative skills. In the therapeutic relationship, interpersonal strategic communication is used, along with previous information and knowledge, empathy, commitment to balance of power, and assertive and clear language and behavior, whose focuses in the patient’s life involve a conversation of healing and care (Greenhalgh & Heath, 2010).
Communication skills include (Epstein et al., 2005):
- Creating a sustainable relationship with the patient
- Exploring the patient’s perspective and helping the patient verbalize emotional experiences
- Using empathy
- Encouraging the sharing of tasks and the joint development of strategies that aim to improve health outcomes
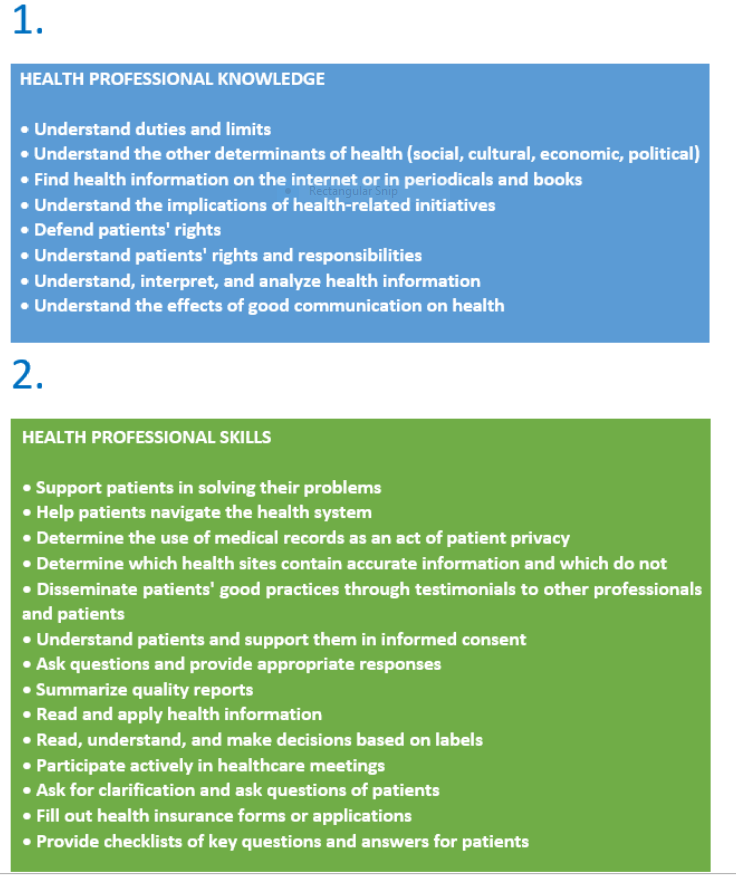
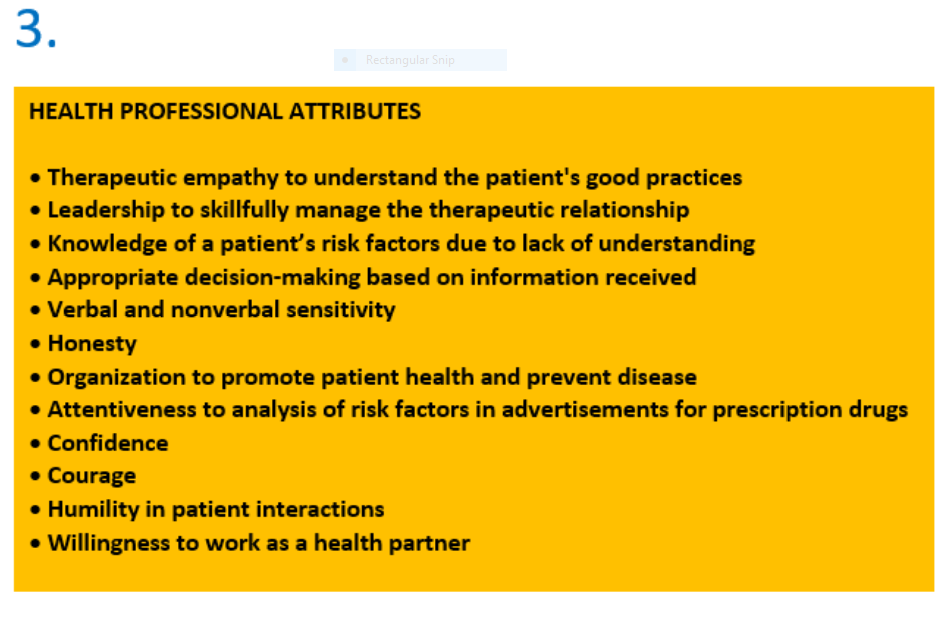
In Table 1, we summarize some of the main competencies of health professionals integrated respectively in knowledge, skills, and personal attributes.
Competencies of health professionals
Examples of competencies: Knowledge, skills, and attributes of health professionals
Cristina Vaz de Almeida is director of the Postgraduate Course on Health Literacy at ISPA in Portugal.
References
Cegala, D. J. (2003). Patient communication skills training: A review with implications for cancer patients. Patient Education and Counseling, 50(1), 91–94. https://doi.org/10.1016/S0738-3991(03)00087-9
Epstein, R. M., Franks, P., Shields, C. G., Meldrum, S. C., Miller, K. N., Campbell, T. L., & Fiscella, K. (2005). Patient-centered communication and diagnosis testing. Annals of Family Medicine, 3(5), 415–421. https://doi.org/10.1370/afm.348
Flynn, T. (2014). Do they have what it takes? A review of the literature on knowledge, competencies, and skills necessary for twenty-first-century public relations practitioners in Canada. Canadian Journal of Communication, 39, 361–384. https://doi.org/10.22230/cjc.2014v39n3a2775
Greenhalgh, T., & Heath, I. (2010). Measuring quality in the therapeutic relationship: An inquiry into the quality of general practice in England. The King’s Fund. https://www.kingsfund.org.uk/sites/default/files/field/field_document/quality-therapeutic-relationship-gp-inquiry-discussion-paper-mar11.pdf
Hargie, O. (2011). Skilled interpersonal communication: Research, theory and practice. Routledge.
Hulsman, R. L. (2009). Shifting goals in medical communication. Determinants of goal detection and response formation. Patient Education & Counseling, 74(3), 302–308. https://doi.org/10.1016/j.pec.2008.12.001
Leape, L. L. (1994). Error in medicine. Journal of the American Medical Association, 272(23), 1851–1857. https://doi.org/10.1001/jama.1994.03520230061039
Leonard, M., Graham, S., & Bonacum, D. (2004). The human factor: The critical importance of effective teamwork and communication in providing safe care. BMJ Quality & Safety, 13(Suppl 1), i85–i90. https://doi.org/10.1136/qhc.13.suppl_1.i85
Light, J., & McNaughton, D. (2014). Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication? Augmentative and Alternative Communication, 30(1), 1–18. https://doi.org/10.3109/07434618.2014.885080
Moscovici, F. (1981). Competência interpessoal no desenvolvimento de gerentes [Interpersonal competence in the development of managers]. Revista Administração Empresarial, 21(2), 17–25. https://doi.org/10.1590/S0034-75901981000200002
OECD. (2005). The definition and selection of key competencies: Executive summary. https://www.oecd.org/pisa/35070367.pdf
Tench, R., & Konczos, M. (2013). Mapping European communication practitioners competencies: A review of the European Communication Professionals Skills and Innovation Programme: ECOPSI. ECOPSI. https://pmr.uni-pannon.hu/articles/4_2_tench_konczos.pdf
Vaz de Almeida, C. (2019). Capacitação dos profissionais de saúde. Literacia em saúde e competências de comunicação dos profissionais de saúde. O modelo de comunicação em saúde ACP [Training of health professionals. Health literacy and communication skills of health professionals. The ACP health communication model]. Revista Nephros, 21(1), 25–28.
Wiemann, J. M. (1977). Explication and test of a model of communicative competence. Human Communication Research, 3(3), 195–213. https://doi.org/10.1111/j.1468-2958.1977.tb00518.x
Wiemann, J. M., & Backlund, P. (1980). Current theory and research in communicative competence. Review of Educational Research, 50(1), 185–199. https://doi.org/10.3102/00346543050001185
