Focus Study: Osteoporosis – Screening & Treatment for the Elderly
July / September 2004
![]()
Focus Study
Osteoporosis
![]()
Screening & Treatment for the Elderly
Fractures resulting from minimal trauma result in significant morbidity and mortality in the elderly. These fragility fractures are related to underlying osteoporosis. Each year, an estimated 1.5 million women, about 4 in 10, experience osteoporotic fractures in the U.S. Up to 20% of women with a hip fracture die within one year (National Osteoporosis Foundation, 2003). The number of new osteoporotic fractures exceeds the number of new cases of breast cancer and heart disease in patients older than 65 (American Heart Association, 1999; American Cancer Society, 2000). In the following focus study of elderly female patients living in the community, we found a high prevalence of undiagnosed and untreated osteoporosis.
Study group
The subject of the study was 257 elderly participants in the PACE CNY (Program of All-Inclusive Care for the Elderly) program. PACE CNY is one of 31 programs nationwide whose purpose is to maintain frail elderly people in their homes and/or the community by maximizing independence and functional ability. A team of healthcare professionals work together to coordinate all the services necessary to help the client manage in his or her home and surroundings successfully. Most participants are nursing home eligible; however, less than 10% actually require skilled-nursing facility (SNF) services.
Study Design
The PACE CNY census is approximately 85% female and 15% male participants. All men were excluded from the study, as well as women under the age of 65, as they fell outside of the current U.S. Preventive Services Task Force (USPSTF) guidelines for osteoporosis screening.
The initial census in our study was 174 subjects. A chart review was performed on all study participants by the authors, and an informational letter was sent to participants and families informing them of our study. The study was conducted over 10 months and included active patients enrolled through March 30, 2003. At the initiation of the study, baseline data was collected. Charts were screened for an existing diagnosis of osteoporosis, a history of a fragility fracture, history of spinal compression fracture, and current treatment being provided for osteoporosis. World Health Organization (WHO) and National Osteoporosis Foundation (NOF) guidelines were utilized for screening and treatment decisions (Figure 1).
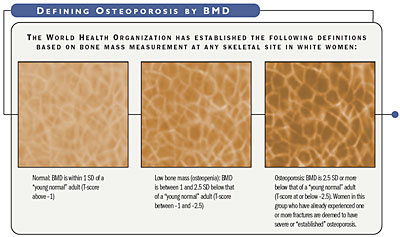
![]()
Although these definitions are necessary to establish the prevalence of osteoporosis, they should not be used as the sole determinant of treatment decisions (NOF, 2003).
After chart review, three groups were identified: Patients who were appropriately diagnosed, patients who met clinical diagnosis for osteoporosis (but had not been identified as such), and participants who did not meet clinical criteria for a diagnosis, but met criteria for screening. Some patients had been diagnosed with osteoporosis but were not receiving appropriate therapy.
Study Results
Of the 174 participants in the study, 96 met a clinical diagnosis of a fragility fracture or had a prior DXA (dual energy x-ray absorptiometry) scan showing osteoporosis. Out of 96 participants, 74 (77%) were correctly diagnosed at the time of our study. However, of the 74 correctly diagnosed with osteoporosis, only 18% were treated appropriately with antiresorptive therapy. The remaining 78 participants all met WHO criteria but had not been screened and were then placed in the osteoporosis screening arm of the study (central DXA scan). Of these, 29 participants refused to be screened, and 6 expired or disenrolled from the PACE program (2 participants were felt to have a contraindication to the scanning). The remaining 41 participants underwent DXA scanning with results showing 22 participants (54%) meeting radiographic criteria for osteoporosis, 17 (42%) showing osteopenia, and 2 of 41 (5%) having normal results.
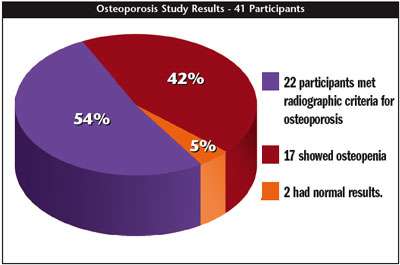
![]()
Discussion
One in five seniors in fee-for-service Medicare was treated for an injury in 1999. Medicare spent more than $8 billion in 1999 to treat injuries to seniors, with fractures accounting for two-thirds of the spending (Bishop, et al., 2002). Researchers recommend focusing on fractures in particular because of their high cost and prevalence. In 1997 Congress approved Medicare coverage for bone mass measurements that would screen for osteoporosis, and USPSTF recommends osteoporosis screening for all women over the age of 65.
Fragility fractures result in a significant morbidity and mortality in elderly patients. Some studies have estimated hip fractures result in a 10-20% excess mortality rate in one year. Additionally, up to 25% of hip fracture patients may require long-term nursing home care, and only a third fully regain their pre-fracture level of independence (NOF, 2003). Hip fractures incur the greatest osteoporosis-related healthcare expenditure. The cost of a hip fracture repair and rehabilitation has been placed in the $16,000 range (Burge, Worley, & King, 1997).
According to the WHO, osteoporosis should be considered a progressive systemic disease, characterized by microarchitectural deterioration of bone, rather than a natural consequence of aging (WHO Study Group, 1994). Therapy with bisphosphonates has been shown in multiple studies to most effectively reduce (hip) fracture risk in osteoporotic women and is well tolerated. A 40% relative risk reduction was noted in The HIP Intervention Program in women with osteoporosis (McClung, et al., 2001). Therapy can be provided at an estimated cost of approximately $1,200 a year. Impact on quality of life is an obvious benefit to reduction of fractures.
Current treatment guidelines call for bisphosphonate therapy as the preferred therapy based on effectiveness in reducing the risk of fragility fractures. Calcium supplementation with vitamin D should also be provided to all patients both at risk of osteoporosis and in the presence of osteoporosis in combination with bisphosphonates. Contraindications to bisphosphonates include esophageal disease such as dysmotility, active GI bleeding, esophageal ulcers, or severe reflux disease. For patients with a creatinine clearance less than 30ml/minute alternative therapy should be considered or frequency of dosing may be extended.
Summary
We found an extremely high prevalence of osteoporosis in this elderly female population and a very low rate of diagnosis and appropriate treatment. Only a small percentage of patients eligible for screening as recommended by USPSTF and WHO actually received bone mineral density (BMD) testing.
Intervention
During a 10-month period following the initial chart reviews, intervention took place. Interventions included staff education, implementation of DXA screening, and treatment per WHO and NOF guidelines. At the conclusion of our study, all participants except those who refused were diagnosed, screened, and treated appropriately. Further education of the medical profession is necessary to increase awareness of this condition. Our program also includes a comprehensive falls prevention program involving all staff, patients, and family. In addition, we have added osteoporosis screening and treatment as a quality indicator on our Quality Report Card and will be adding it as part of our standard admission orders for all new enrollees.
Conclusion
Our results represent the practice patterns of a wide spectrum of healthcare practitioners from a wide range of specialties. Most of our participants were recently enrolled in the PACE program and were previously cared for by other community physicians. Study results show that healthcare providers are not consistently diagnosing, screening, or treating osteoporosis, a condition with significant negative impact on the elderly. Effective treatment for this condition is available and is considered the standard of care. Healthcare providers should focus on screening and treating osteoporosis as aggressively as they do heart disease and other common diseases.
- All post-menopausal women should be on calcium and vitamin D supplementation.
- Elderly female patients suffering a minimal trauma fracture should be presumed to have osteoporosis and be treated with anti-resorptive therapy.
- All other women over the age of 65 should undergo bone mineral density testing with appropriate follow-up and treatment.
The medical community largely under-appreciates the impact of osteoporosis on elderly patients.
References
National Osteoporosis Foundation. (2003). Physicians’ guide to prevention and treatment of osteoporosis.Washington, D.C.: Author.
Dennis D. Daly, MD, is the medical director for PACE CNY and Loretto Geriatric Center in Syracuse, New York. He is board certified in family practice with added qualifications in geriatrics. Dr. Daly is a Diplomate of ABQAURP and serves as the chairman of the Utilization Review Committee at Community General Hospital in Syracuse. He has a private practice in Camillus, New York, and consults for several insurance companies and dispute resolution agencies. Dr. Daly may be contacted at dalyde@lorettosystem.org.
Lisa Carr, RN, is the director of quality assurance and process improvement at PACE CNY in Syracuse, New York. She is a Diplomate of ABQAURP and has 10 years of experience in the field of quality improvement. Carr has experience in malpractice case reviews and plays a vital role in the Utilization Review Committee at PACE CNY, particularly in the field of pharmacy and therapeutics. Carr may be contacted at arrli@lorettosystem.org.
