Five Essential Components of an Effective Stroke System
January / February 2010
![]()
Five Essential Components of an
Effective Stroke System
Approximately 795,000 Americans will have a stroke this year. Stroke is the third leading cause of death in the United States and a leading cause of serious, long-term adult disability. The direct and indirect costs associated with stroke are projected to exceed $65 billion in 2009, according to the National Stroke Association.
These ominous statistics fuel efforts within the medical community to continue to improve stroke prevention and treatment. From a care perspective, there have been tremendous advances in diagnosis and treatment. New endovascular treatments for cerebrovascular disease coupled with enhancements in the quality and availability of imaging studies have revolutionized stroke care (Guzick, 2009).
A stroke patient’s outcome, however, depends on more than dedicated clinicians, advanced technology, and a sense of urgency. The complexity of the disease demands an integrated, collaborative approach to care. Evidence suggests that success depends on having a well-coordinated and fully integrated stroke system in place and ready to act. This system should encompass prevention, outreach, education, transient ischemic attacks (TIAs), acute stroke, and rehabilitation.
Outreach to the community is a critical component within an effective stroke system. Organizations that can treat the full range of stroke victims must leverage these capabilities to address the unmet care needs in their region. This is accomplished through a “hub-and-spoke” model in which the stroke center (hub) establishes a transfer relationship with other area hospitals, clinics, nursing homes, and healthcare providers (the spokes) that lack the primary center’s sophisticated stroke care capabilities.
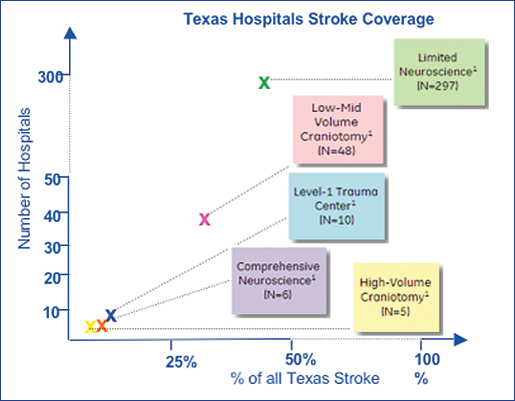
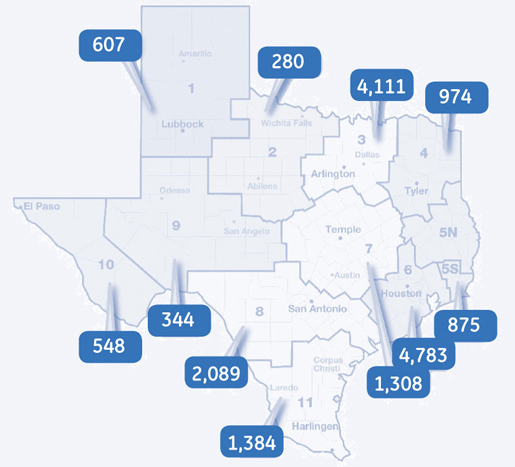
The neurological care landscape in Texas is just one of many examples of the need for a hub-and-spoke approach to stroke care. Of 409 hospitals in Texas, 297 have limited capabilities to treat patients with complex neurological disease (Figure 1). Yet, 80% of the state’s stroke patients are seen at these hospitals. The Houston region has the highest incidence of stroke discharges in the state and is home to three institutions that meet criteria outlined by the Brain Attack Coalition for Comprehensive Stroke Centers (Figure 2). However, only 25% of Houston’s stroke patients currently receive care at these centers.
Putting a hub and multi-spoke system in place can overcome treatment inequities and ensure that the best possible stroke care gets disseminated to the highest percentage of the population.
Within such a system, patients are swiftly navigated through a complex web of individualized decisions to expedite care. A well-run system that effectively integrates these decisions can yield significant clinical, operational, and financially payoffs.
The role of stroke systems in improving patient outcomes is being recognized by healthcare policy-makers. In August 2009, for example, the state of Illinois joined New York, Florida, and others in implementing legislation that allows emergency medical services (EMS) providers treating stroke victims to bypass the nearest hospital in favor of a designated stroke center (Graham, 2009).
According to the American Stroke Association (ASA), “dedicated stroke units can reduce a patient’s risk of death by 40%.” If every state had stroke systems of care in place, says the ASA, the country could make “significant progress toward a 25% reduction in coronary heart disease, stroke, and risk.”
To achieve that goal, the ASA has convened a Task Force on the Development of Stroke Systems to encourage the implementation of coordinated stroke care. Comprising experts in the areas of stroke prevention, emergency medical services, acute stroke treatment, stroke rehabilitation, and health policy development, the Task Force has determined that a stroke care system should serve three critical functions (Schwamm et al., 2005):
- Ensure effective interaction and collaboration among all the agencies, services and people involved in caring for stroke patients.
- Promote the use of an organized standardized approach in each facility and component of the system.
- Identify performance measures (both process and outcomes) and provide a mechanism for evaluating effectiveness so the stroke system can continue to evolve and improve.
Meeting these criteria is a complex undertaking that involves multiple operational issues. To create a system capable of providing integrated, standardized, and effective stroke care, we believe there are five “make-or-break” operational requirements for the primary stroke center:
- Collaborative relationships with EMS providers
- Stroke-focused emergency department (ED) operations and patient flow
- Trust between neurologists and ED physicians across the system
- Effective governance of the stroke program at all levels
- Strong technology backbone
1. Relationships with EMS providers
EMS is the transmission of an effective hub-and-spoke stroke system. Effective coordination and communication between hospitals and EMS is essential to a stroke system.
A hospital can have the most advanced neurosciences program in the community, but if ambulances aren’t routinely bringing stroke victims to the emergency department, the stroke program will not thrive. One hospital that engaged a consultant to help upgrade their stroke care capabilities was shocked to learn that EMS providers in the community avoided their ED whenever possible because, according to the EMS personnel, it was always at capacity and the nurses were not accommodating and often rude. It’s critical to have candid discussions with EMS providers in the community to learn how your hospital is perceived by the very people who determine a stroke victim’s treatment destination. If problems are identified and documented, you can work to create conditions that enable a more effective relationship with EMS.
2. Emergency department operations and flow
Upon arrival at the hospital, the patient will be seen by either the rapid response team, the acute stroke team or, in many cases, the ED staff to assess, diagnose, and determine whether the patient should be admitted or transferred to a higher level of care, receive thrombolysis, and/or undergo surgery or intervention. Pre-existing conditions must be considered, and care pathways must be adjusted accordingly.
Delays at any point in this decision tree may be life-threatening, and there is often little margin for mistakes. This is complicated by two additional factors: first, key clinical resources are often not in close proximity; and second, the organization is overburdened by other patients with emergency needs. Since a stroke case could present at any time of any day, stroke programs must have every aspect functioning effectively 24/7/365.
Discharge planning is one of the most significant operational issues for acute stroke. A stroke center needs appropriate processes to monitor length of stay and guide placement of patients in a lower level of care, such as a skilled nursing or rehabilitation facility. If proactive discharge planning is not occurring between the medical staff and the hospital caregivers, stroke victims are likely to spend additional days as an inpatient. This drives up cost and—for congested facilities—claims inpatient beds that could be used for other patients.
3. Relationships between neurologists and
ED physicians across the system
To be effective, a stroke system of care must be supported by a network of physicians who share not only protocols, but also mutual trust and respect. Shared protocols are essential, but they are not enough. The network will only be effective if neurologists, neurosurgeons, and emergency medicine providers have established relationships that can be called upon for both consults and transfers. When building a stroke network, special attention should be paid to build and nurture these relationships.
4. Governance of the stroke program
Continuous, systematic improvement is the hallmark of any well-run clinical program, including stroke care. The governance structure for a stroke program is critical to success. Great governance includes a clear vision, mission, and guiding principles that are embraced across the network.
5. Technology backbone
Delivering great stroke care requires multiple technologies that are effectively integrated and available to caregivers. At a minimum, stroke centers must provide timely access to a CT that is capable of scanning to industry-accepted standards for stroke care. While state-of-the art stroke care continues to evolve, capabilities should include tissue classification (to visualize the infarct core and salvageable penumbra), quantification of blood flood, and maximum coverage with a single bolus of contrast.
Telemedicine for stroke, or “telestroke,” uses various forms of technology, such as videoconferencing and teleradiology, to quickly link patients from the pre-hospital setting to the ED or from an ED or outpatient setting in an underserved area to expert stroke care. These technologies range from the basic (telephone and email) to the more advanced (robot systems). Physicians such as stroke neurologists can access CT studies and laboratory results, perform standardized stroke scale assessments, and even discuss treatment options with patients and families via telemedicine systems.
The benefits of advanced stroke care technologies include accurate stroke assessment to determine appropriate treatment, improved outcomes, increased comfort in the administration of therapeutic drugs, and wider access to acute stroke care in a variety of settings.
Realizing the Promise of Stroke Care
According to the ASA Task Force, a stroke system should
provide both patients and providers with the tools necessary to promote effective stroke prevention, treatment, and rehabilitation. Effective stroke care requires coordination of the activities and resources of a broad range of individuals, facilities, and organizations…to ensure that the appropriate patients are receiving care from the appropriate providers in the appropriate amount of time (Schwamm, 2005).
When knowledgeable and committed practitioners in every region of every state are enabled by an effective system such as this, the improvement in stroke care and patient outcomes in the United States will be dramatic.
Jeff Terry is managing principal for clinical excellence at GE Healthcare’s Performance Solutions. He is a member of the American College of Healthcare Executives (ACHE), Institute for Healthcare Improvement (IHI), and the Texas Hospital Association. Terry earned a BE in electrical engineering from Vanderbilt University in Nashville. He has a master’s degree in business administration from Marquette University in Milwaukee and is a Certified Six Sigma Black Belt. He may be contacted at Jeffrey.Terry@med.ge.com.
Jennifer Jefferson is senior manager at GE Healthcare’s Performance Solutions. She leads GE Healthcare’s Stroke System of Care model, which focuses on improving outcomes for stroke patients through increased ability for underserved areas to provision advanced neurology & neurosciences care. Jefferson has also worked in healthcare supply chain management and e-commerce with multiple Fortune 500 companies She earned a BS in business administration from the University of Colorado at Boulder and is a Certified Six Sigma Black Belt.
References
American Stroke Association & American Heart Association. (n.d.). Stroke systems of care – Making the case. Accessed October 14, 2009 at http://www.strokeassociation.org/downloadable/heart/1186427558267Stroke%20Systems%20of%20Care%20-%20Making%20the%20Case.pdf
Graham, J. (2009, August 14). Quinn signs bill to open stroke centers. Chicago Tribune Accessed October14, 2009, at http://mobile.chicagotribune.com/inf/infomo?view=breakingnews_article&feed:a=chi_trib_1min&feed:c=latest_breaking_news&feed:i=CD58EAF0C30D223EF8AE796F6F2C529A
Guzick, D. (2009, February 23). Miracles of modern medicine: Advances in stroke management. University of Rochester Medical Center, School of Medicine & Dentistry. Accessed November 18, 2009, at http://www.stroke.org/site/DocServer/STROKE_101_Fact_Sheet.pdf?docID=454
National Stroke Association. (2009). Stroke 101 fact sheet. http://www.stroke.org/site/DocServer/STROKE_101_Fact_Sheet.pdf?docID=4541 Accessed October 6, 2009.
Schwamm, L. H., et al. (2005). AHA scientific statement: Recommendations for the establishment of stroke systems of care. Stroke, 36, 690.