Engaging as Partners in Patient Safety: The Experience of Librarians
March / April 2009
![]()
Engaging as Partners in Patient Safety:
The Experience of Librarians
In today’s healthcare environment, a broad team of professionals should engage in the quest to improve patient safety through identifying and discussing the successes and failures that lead to organizational learning. Often it is stated that management engages the entire organization in this work, but rarely is the role of the librarian explicitly noted. It has been observed that multidisciplinary teams are wiser when they allow for diverse input (Surowiecki, 2004). Broadening the base of experts in the clinical environment to include librarians and information professionals can help to accelerate progress by improving access to what the organization knows and learning from the experience of others (ISMP, 2008; Conway, 2008).
Opinions are mixed as to whether improvements in patient safety have been achieved since publication of the Institute of Medicine’s To Err Is Human (Kohn et al., 2000; Leape & Berwick, 2005; Wachter, 2004). This notable publication created urgency for changes in care processes to mitigate failures, reduce medical errors, and subsequent harm to patients. Since 2005, improvements have been realized due to national and local campaigns focusing on improving distinct areas of care delivery, but still much work needs to be done (Leape, 2007). In 2001 a call to action to involve librarians was elicited after an incomplete literature review contributed to the death of a health research volunteer (McLellan, 2001).
Due to these benchmarks, librarians’ involvement in patient safety work has received increased visibility. According to a survey of librarians first reported in 2004, librarians were not proactively engaged by leadership as partners in efforts to improve the safety of medical care. Librarians, however, definitely saw a role for themselves in safety work, building on their established skills in information access, providing training and on-demand research (Zipperer & Sykes, 2004).
Librarians working in a healthcare environment are increasingly exposed to patient safety as an area for professional discourse and development. A symposium featuring nationally recognized speakers was held at the Medical Library Association (MLA) annual meeting in 2006. The National Library of Medicine web site hosts a training course and annotated bibliography, and posters and professional papers have been delivered at national and regional conferences (Patient Safety Resource Seminar, 2007). Publications that explore efforts related to the impact of information resources on safety are beginning to appear (Robinson & Gehle, 2005; Hendler & Napp, 2006; Albert, 2007). In addition, health literacy, an avenue that librarians are working to influence, is now seen as a component of effective and safe, patient-centered healthcare (Medical Library Association).
This increased visibility over the past several years set the stage for measuring improvements in how librarians see their role in patient safety. A survey was undertaken as a means of focusing attention on the topic of safety in the healthcare arena. The authors wanted to assess the extent to which librarians’ understanding of safety science and safety behaviors had matured and if they were communicating to clinicians and leadership how their experience in information management and knowledge transfer can positively impact patient care. A survey used in 2003 to explore this impact was revised slightly and re-disseminated to the library community in 2006 to:
- ascertain whether librarians envision a broader application of their skill set,

- determine whether librarians had established new or more robust roles in the patient safety work of their organizations,

- define relationships being built by librarians to educate and involve themselves in safety work, and

- identify opportunities for librarians to uncover and correct areas of potential failure that could affect the safety of patients.
Data collection was closed in early 2007.
Mapping the Landscape
The 2007 survey was comprised of 12 questions: the first two asked the respondents to describe their job functions and the types of organizations for which they worked; the remainder asked about librarians’ involvement with patient safety, including whether or not they had witnessed a safety incident, their comfort level in discussing safety issues with hospital personnel, and their concerns about how professional literature is accessed and used. The survey distribution was broader and included announcements in a print publication as well as electronic vehicles outside the professional network of librarianship. The exact number of persons receiving the invitation to participate in the survey is unknown since it was posted to multiple discussion lists and also forwarded from the discussion lists to persons thought to be interested in the topic. The 2003 survey was modified slightly to improve the reliability of the results and to respond to changes in the environment since the first survey was disseminated.
Two topics not addressed in the 2003 survey were added to the 2007 survey. In the first survey, it was learned that leaders in healthcare organizations typically did not engage librarians in identifying opportunities for safety improvements or in peer-to-peer education. In reaction to this, the 2007 survey asked librarians to identify people with whom they discussed patient safety concerns.
The 2003 survey did not ask if librarians and information professionals (including persons working in the library, information management, and knowledge management fields who may or may not have a library or information science degree) observed errors or safety infractions in the course of their daily work. Given that the library community has been exposed to more safety concepts through education and publications, the authors attempted to gather benchmark data on the experience of librarians in dealing with error or near-misses in the 2007 survey.
Results for Discussion
This article presents highlights from the 2007 survey. It also discusses the need for clarification and continued development of the role librarians can play in impacting safety based on what was learned from the survey responses. Librarians and other information professionals from a variety of clinical environments in a variety of roles responded to the survey. The survey questions and the complete data from the survey are available from the authors.
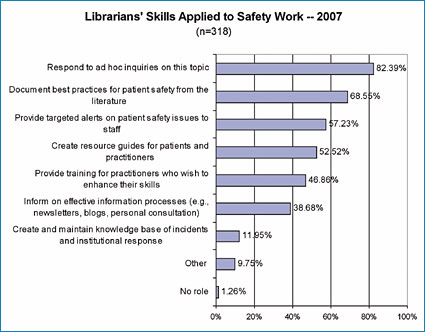
In order to learn whether librarians and information professionals have expanded their involvement in patient safety, the 2007 survey again asked respondents to choose from a list all of the activities in which they participate. In the 2003 survey, only four persons (of 174 total respondents) indicated they had no role in patient safety activities. In 2007, four persons (of 318 total respondents) indicated they had no role in patient safety activities. In 2007, 82.4% of the survey population responds to ad hoc inquiries on patient safety. As in the 2003 survey, this activity ranked first of all the options offered. More than half of persons who responded are also involved in documenting best practices for patient safety from the literature (68.55%), providing targeted alerts on patient safety issues to staff (57.23%), and creating resource guides for patients and practitioners (52.52%).
It is significant that 46.86% provide training for practitioners who wish to enhance their skills, since respondents reported a lack of confidence in practitioners’ research skills as well as concerns about how the research/evidence was accessed and used. Related to this, another 38.68% inform others regarding effective information processes (e.g., via newsletters, blogs, or personal consultation). Creating and maintaining knowledge bases of incidents and institutional responses are not yet practices widely assigned or embraced by librarians and information professionals; only 11.95% report involvement in such efforts. Librarians’ training and experience in creating and using databases should prove to be a valuable resource for preparing such knowledge bases.
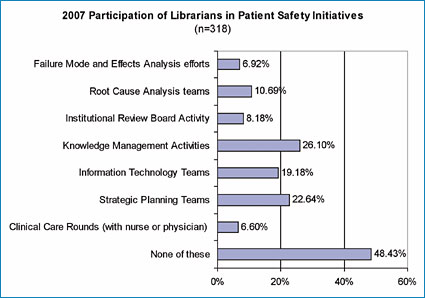
The involvement of librarians and information professionals in higher-level knowledge management (KM), strategic planning, and safety management remained relatively low among survey respondents.
There is a distinction between information management and knowledge management that is worth clarifying. Knowledge management activities involve connecting “what people know” in a largely undocumented manner. It tends to focus on sharing of experience in a rich context-oriented fashion.
Information management activities revolve around the maintenance and organization of tangible items that report on or encapsulate data or information (e.g., collecting, organizing and distributing content such as documents or reports created within an organization or published outside of the organization such as journals, books, or research studies).
A metaphor to illustrate the difference could be:
If someone asks directions, information delivery would be handing them a map; knowledge delivery would be explaining the bumps in the road, describing the house at the corner, suggesting they stop at the great coffee stop just past the turn and the warning to be careful about the cop that hides behind the large lilac bush.
The examples used to define KM on the survey instrument included building expertise directories, managing communities of practice, collecting and sharing best practices, and involvement in collecting and sharing stories. Membership on IT or strategic planning teams and other activities that demand interaction and discussion about patient safety with persons in other departments were also noted. Only 26.10% of the survey respondents reported being involved in KM activities, while almost half (48.43%) of respondents do not participate in KM activities. This is a 20.38% decline from the 2003 survey. In the 2007 survey, examples of KM activities were listed on the survey instrument and the authors speculate that the distinction between information management and knowledge management activities may not have been clear to persons responding to the 2003 survey.
It is encouraging that some information professionals are stepping up to participate in these activities, including 72% that participate in selecting tools for evidence-based medicine (EBM) decision-support and 6.6% who report participating in clinical care rounds with a nurse or physician.
![]()
To explore opportunities for partnership in safety work, the survey asked the question: “With whom do you discuss patient safety issues?” Of 318 respondents, 63.72% reported participating in discussions about patient safety with nurses. This level of trust and interaction is noteworthy and warrants further study to learn how this openness has developed and if it could be achieved with other healthcare professionals. Other groups with relatively high levels of interaction with librarians are: risk managers (49.21%), administrators (43.85%) and physicians (43.53%). The survey instrument invited multiple responses to this question.
A new question was added on the 2007 survey regarding the respondents’ observation of or interaction with error incidents to ascertain librarians’ ability to play a role in recognizing and mitigating failures.
When reflecting on errors (defined as failure of planned actions to reach specific goals; Reason, 1990) that could potentially impact patient care, 6% reported they had witnessed an incident, 6% had intercepted a potential incident, and 5% had personal involvement with an incident; 6.3% preferred not to answer or did not know if they had witnessed an incident, 12.3% did not know or preferred not to answer regarding interception of an incident, and 8.2% did not know or preferred not to answer regarding having personal involvement with an incident. These percentages are relatively small, but suggest that librarians are alert to and cognizant of the impact of errors. How can this sensitivity be tapped to give them a full voice in the discussion of error?
Narrative Responses in 2007 Survey
As in the 2003 survey, narrative comments were categorized under six general themes:
- Culture. A lack of librarian involvement at a strategic level on patient safety information-related issues still persists. In general, librarians are not effectively promoting their unique skills and expertise, while management is not actively seeking out their participation/contribution in safety initiatives.

- Leadership. These issues were less prominent in the 2007 results although a lack of leadership commitment to respecting librarians as partners in safety improvement was noted.

- Process. Concerns centered on the belief that information resources and literature identified by librarians for safety work were not effectively shared, thus illustrating a knowledge management issue for the hospital. In addition, the process for obtaining information did not regularly involve librarians to ensure correct and complete results of literature searches.

- Research skills. Librarians continue to be troubled by clinicians’ lack of literature research skills and the fact that incomplete results can seriously affect patient care. Comments regarding clinician reliance on prepackaged evidence reviews (without additional scrutiny of materials for currency, authority, applicability, and specificity), and extensive use of Internet search engines illustrated this concern.

- Individual responsibilities and skills. Survey participants expressed unease that convenience trumps quality in retrieving published clinical evidence. There was concern voiced that the need for hospital staff to identify and refer to patient safety information was more often reactive than proactive.

- Resource/access issues and time factors. Librarians recognize that clinical staff has little time to fully explore the literature. This suggests an opportunity for librarians to partner with clinicians to address this gap, but a mechanism to effectively establish this relationship is lacking. Financial resources needed to build adequate collections related to safety, and updating general medical resource collections were also mentioned as concerns.
![]()
Steps for Moving Forward
The authors were encouraged by the engagement reflected in the response to the survey, but recognize that the survey results provide only a snapshot of the role of librarians in patient safety work at a given moment in time. A more systematically executed, statistically powered, in-depth survey is required to obtain a more definitive understanding of the profession’s impact on safety work in hospitals. Such analysis was beyond the scope of this project.
To underscore the opportunities for improvement in safety work through partnership with librarians, the authors re-emphasize the need for medical personnel and healthcare leadership to:
- Acknowledge the potential negative impact of incomplete or erroneous literature search activity on patient care and accept responsibility for addressing this as a patient safety issue. Accountability for safety rests at every level (Kohn et al., 2000).

- Seek opportunities to learn about the positive impact of effective information and knowledge partnerships in the clinical environment (Banks et al., 2007; McGowan et al., 2008; Vaida & Zipperer, 2006).

- Engage the library and information professional community more aggressively to understand how information biases affect safety and how information professionals can mitigate such biases by providing training on resources and search techniques. Risks exist in mismanagement of information (Choo, 2005).

- Explore how experiences involving librarians in knowledge management initiatives in the non-clinical healthcare and corporate sectors can be applied to the clinical care setting (Donaldson & Gray, 1998; World Alliance for Patient Safety, 2008).

- Measure the impact librarians have on patient safety through their ability to recognize and address health literacy weaknesses in their interface with patients, patients’ families, and caregivers.
Librarians also have a responsibility to engage in their organization’s safety work. It would behoove them to articulate a commitment to safety in their strategic planning process to demonstrate their role to leadership. In addition, they should capitalize on opportunities to learn about safety though organizational sessions, local conferences, or national symposia.
The survey revealed that some librarians are already supporting safety work. Tactics include:
- Ordering key publications in the field of safety (even if it means cutting other areas) and communicating that to stakeholders.

- Setting up RSS feeds with safety news for the intranet.

- Establishing relationships with practitioners (e.g., nurses) and non-clinical staff (risk managers) to regularly discuss the topic.

- Participating in executive walk-around programs to learn from that experience.

- Hosting learning sessions or book discussions on safety topics.

- Folding health literacy expertise into projects related to patient safety.

- Setting up and contributing to communities of practice to support learning at the unit or project level (Bandy et al., 2008).
When librarians are engaged to identify and proactively address areas where failure might occur in the information retrieval and transfer processes, they are in a position to contribute to organizational learning efforts. The increased participation of librarians and information professionals in the survey was encouraging and confirms librarians’ desire to apply their search expertise and knowledge of information seeking behaviors into the patient care process because they share a commitment to patient safety. The authors hope to see librarians increasingly involved on failure analysis and safety strategy teams.
Jan Sykes has more than 20 years of experience in the information industry. Currently, she leads Information Management Services, Inc., which concentrates on information and knowledge management projects, including needs assessments, strategic planning activities, and resource selection. Jan relies on a thorough understanding of information market trends, information-seeking behaviors, and the synergies between information, knowledge, and learning to help clients realize the greatest value from their spending on information resources.
