Empowering Care through Communications Technology
January / February 2007
Empowering Care through Communications Technology

Partners Telemedicine
September 18 — 19, 2006
The Conference Center at Harvard Medical
Boston, Massachusetts
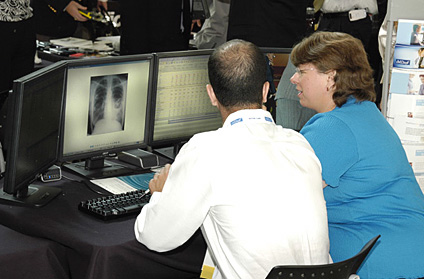
 Nearly 600 attendees participated in Partners Telemedicine’s 3rd Annual Connected Health Symposium. Panels and workshops covered a range of practical and theoretical issues in connected health, such as establishing telestroke and other connected health programs, new models for payment strategies, telehealth investing, wireless communications, public policy, clinical practice in the telehealth era, research challenges, and applications for connected health in pharmaceutical research and development.
Nearly 600 attendees participated in Partners Telemedicine’s 3rd Annual Connected Health Symposium. Panels and workshops covered a range of practical and theoretical issues in connected health, such as establishing telestroke and other connected health programs, new models for payment strategies, telehealth investing, wireless communications, public policy, clinical practice in the telehealth era, research challenges, and applications for connected health in pharmaceutical research and development.
In his opening remarks, Dr. Joseph Kvedar, director of Partners Telemedicine, challenged participants to answer five questions central to the future of connected health, a term that best captures the broad range of telehealth, remote care, and disease and lifestyle management programs that are changing the healthcare delivery system and improving quality patient care:
- What do patients want, and what are they willing to pay for?

- How can we change the healthcare economics to provide incentives to encourage better care and improved adherence to therapeutic regimens?

- How can we design better technology that is easy to use and that will create meaningful, accurate, and reliable data?

- How can payers and providers be encouraged to implement new models of care that encourage quality and cost effectiveness?

- What are the applications of connected health in the areas of fitness and wellness?
A particularly poignant panel discussion addressed the need to increase convenience, quality, and patient satisfaction, clearly illustrating the role patients must play in their healthcare. Each panelist relayed personal experiences with the healthcare system that were not patient friendly. Perhaps the most dramatic story was told by Gene Sacco, MBA, associate director of business practices for Wyeth and an advocate for his 20-year-old son, who dying of cancer at the time, spent 12 hours waiting in a doctor’s office for test results. After an exhausting and unexplainable wait, Gene and his family were told that the test he was there to discuss was inconclusive and that they would need to retake the test again in a week.
After hearing this and other similar stories, panelist John Henderson, PhD, a network theorist from the Boston University School of Management, proclaimed that a new metric for healthcare should be considered — Return on Time Invested (ROTI).
This discussion naturally led to other questions and ways to think about how we value healthcare services and how we measure healthcare quality. To date, efforts to track quality have been limited mostly to process measures and patient satisfaction. Managed care organizations have measured patient satisfaction with the care experience and current pay-for-performance systems still base their compensation on a fee-for-service model — yet the crowded waiting room remains the rule rather than the exception.
“I think that ROTI, in combination with a series of other metrics that speak to technical quality in healthcare could be a powerful combination and another accelerant for the connected health market place,” said Dr. Kvedar. “I know many of my clinical colleagues will object to this type of metric. They will say it undervalues the knowledge and experience they bring to the healthcare encounter and over emphasizes the ‘bedside manner’ portion of the provider-patient relationship.”
So, who or what will push connected health into common use? Large self-insured employers are viewed as sleeping giants, with potential to become a leading force in the adoption of connected health. However, most conference attendees expressed the belief that consumers will drive the adoption of connected health, with the Centers for Medicare and Medicaid Services (CMS) driving payers. Intangible forces will also encourage the adoption of connected health. As noted by Barry Zallen, MD, chief medical officer of Blue Cross Blue Shield of Massachusetts, the healthcare quality movement is trending toward clinical outcome measures rather than process-oriented metrics, as well as the pressure of pay-for-performance programs, and these factors will facilitate interest in connected health.
Other drivers discussed include the general integration of technology into society, which creates both a comfort level with and expectation for technology-enabled living; policies on standards for interoperability; and new data as well as program opportunities arising from Medicare Part D.
How We Get There
Attendees agreed unanimously on connected health’s potential to transform healthcare quality and delivery. The cost of chronic disease care, the opportunity to decrease medication errors, and the ability to improve the efficiency of care delivery — problems that exist throughout our healthcare system — were cited by organizations, clinicians, administrators, and consumers as their top reasons for becoming involved in connected health. Life sciences and pharmaceutical companies are also realizing the potential and are embracing connected health programs. For example, by illustrating the high cost of managing non-adherent patients, Terri McGinnis, MD, MPH, a medical director at GlaxoSmithKline (GSK), made a compelling case for implementing connected health interventions to improve medication adherence in chronic disease populations.
The acceptance and implementation of connected health throughout our healthcare system will require appropriate technologies and social acceptance, in order to drive adoption. Several technologists noted that a convergence of multiple technologies — Wi-Fi, IP networks, and cellular networks — will be necessary to support a mobile user population. Another consideration is capacity to support many networks and devices on the move. Availability of reliable wireless networks, which will require expansion beyond the current 75% penetration rate, may be the greatest technological pre-requisite on the minds of technologists.
On the sociopolitical front, speakers called for new policy to protect consumer privacy in a connected world, as well as a public education effort to promote consumer confidence in the exchange of their health information. From a market perspective, participants agreed that initial investment in projects, consumer education, and low price points will be necessary to support a connected health eco-system.

With the goal of developing technology standards for a wide range of interoperable devices from fitness equipment to heart monitors and weight scales, the Continua Health Alliance is the definition of a modern-day ecosystem. Continua has brought together leading technology, healthcare, and fitness companies to better address the need for proactive involvement of patients in their healthcare needs through the application of consumer technologies. David Whitlinger, president of Continua Health Alliance, participated in a panel discussion, along with other members of Continua, and Harvard School of Public Health ethicist, Jeremy Nobel, MD, to discuss how Continua and connected health will foster independence, empower patients and consumers, and improve care.
It also became apparent during the two-day symposium that a deeper sharing of knowledge between the healthcare and technology sectors is needed to foster successful partnerships in telehealth. In addition to divergent knowledge bases, technologists and healthcare providers/administrators experience differing industry realities — such as dramatically different times-to-market for consumer devices as compared to new medicines. These realities translate into substantial differences in culture and expectations that will need to be addressed in order for partnerships to thrive.
Overcoming Barriers
As with any burgeoning industry or new approach, there exist obstacles to acceptance. Perceived barriers to the widespread implementation of connected health fell into three categories: technological, sociological, and systemic.
In terms of technology, participants expressed concerns about legacy systems, interoperability, real-time data delivery, device battery life, and the finite availability of spectrum for wireless connectivity. Technologists were acutely aware of the need for devices that address a diversity of lifestyles and comfort levels among their users. Similarly, remote care systems companies expressed the need to understand and categorize consumer behavior at the micro-level in order to provide appropriate information and motivation.
Others were concerned by a seeming lack of compelling evidence that consumers and physicians should invest in connected health. Compounding that problem is a misalignment of incentives arising from the structure of our current healthcare system that puts consumers, physicians, and payers at odds. In fact, participants implicated the entire healthcare financing/payment system as an obstacle to the advancement of connected health, though they appeared motivated to create solutions to address this critical hurdle.
Connected health researchers expressed interest in developing the skills to identify those data most likely to compel behavior change, in order to limit data collection. Dena Puskin, ScD, director of the Office for the Advancement of Telehealth, noted in her presentation that the multidisciplinary nature of connected health has complicated funding for research.
One prevalently discussed barrier to connected health was the enormous investment of time needed to implement an electronic medical records (EMR) system, yet a national EMR network was named implicitly as a future goal of connected health.
In the minds of conference participants, large-scale studies and programs are also needed to help define the usefulness of connected health and demonstrate its application in various clinical settings.
Motivated to Change
Though attendees openly acknowledged the challenges ahead, the overarching tone of the meeting was one of conviction and commitment to a vision.
If this vision is realized, healthcare will take on an entirely new meaning for consumers, beginning with “whenever, wherever” healthcare, lifestyle and fitness coaching, as well as remote monitoring of elderly dependents. Connected health programs could yield a better return on time invested (ROTI) for patients as they traverse the healthcare system as compared to non-technology-enabled healthcare delivery. Implementing and improving on this metric would provide an enormous lifestyle benefit to patients and caregivers that, as interaction with the healthcare system becomes more convenient, might eventually translate into health benefits.
The connected health paradigm shift would further bring entertaining, compelling technology and easy-to-use, interoperable devices. Customized health and fitness incentives would be built into every health interaction. Targeted education would become an integral part of healthcare transactions, further strengthening patient-physician relationships. Coordination of care, lab test follow up, and allergy and drug interaction checks would become reliable and automatic. In this new system, patients would have care, information, and support at every turn.
By contrast, the use of IT networks associated with connected health would change the daily lives of clinicians. Their vision for connected health includes a technology-facilitated exchange of information between all relevant providers as well as improved data access and analytic capability. Healthcare providers hope for improved patient care enabled by the integration of information and a dynamic, evidence-based practice where care is better coordinated and safer. If and when EMR becomes universal, physicians should be able to devote more time to patient care and less to administering the paper trail. Further, professional medical education and decision support, already Web-enabled, would become more targeted and accessible.
Administrators and researchers would also benefit from connected health. In pharmaceutical and biotechnology research, new devices and connectivity could improve clinical trials management and follow-up, enhance the efficiency of pharmacovigilance, and facilitate a reduction in the size of clinical trials, predicted Dr. Una Ryan, CEO of AVANT Immunotherapeutics, who chaired a panel discussion on drug adherence and clinical trials. Dr. Ryan also foresaw an enormous benefit to global health in the area of infectious disease, with connected health programs and devices being applied to disease surveillance and monitoring, and managing all manner of crises in infectious disease and natural disasters.
Connected Health in Action
Numerous connected health programs and pilots are underway. During the conference, panelists, presenters, and meeting attendees shared experiences and practices currently being implemented in healthcare settings throughout the U.S. Following are highlights from some of the programs presented:
- Military Psychiatry – Through the use of PDAs, military psychiatrists in Iraq can access a network of specialists in the U.S., enhancing field care for patients.

- Retiree Telehealth – Partners Healthcare provides EMR system access to a few physician practices in Florida to improve coordination of care for snowbirds. Massachusetts General Hospital physician, Dr. Timothy Ferris, called this “a micro solution,” but this kind of technology-enabled coordination demonstrates the potential of connected health to facilitate better care for consumers on the move.

- Preventive Telephony – Harvard Pilgrim Health Care uses interactive voice technology to conduct phone outreach to patients to reduce hospital recidivism in patients with co-morbidities and to encourage patients to schedule important lab tests. Similarly, Tufts Health Plan reaches out to its members on issues related to inpatient and outpatient utilization.

- Emergency Care – MassShare, a program to advance the regional sharing of health data in Massachusetts, is piloting an exchange of basic patient data between Brigham & Women’s and South Shore Hospitals to coordinate emergency room visits.

- Technology Integration – CIMIT (Center for Integration of Medicine and Innovative Technology), an incubator for novel applications of technology in medicine, provides engineers and clinicians with seed money and expertise to adapt promising technologies for medical use. CIMIT is currently supporting development of a virtual operating room, an epileptic seizure detection and intervention device, as well as a project in trauma care that draws on battlefield experience, to name a few of its fascinating projects.

- Remote Monitoring in Chronic Disease – Philips Motiva has developed a television platform for remote patient management in chronic diseases. The system is already in use.

- Tele-ICU – The New England Healthcare Institute (NEHI) is focused on determining the role and value of technology and accelerating the adoption of technologies whose potential is proven. NEHI’s Doug Johnston said that Tele-ICUs, which variously combine hardware, software, staff organization, and clinical processes for remote patient monitoring and management, “have both significant value and great metrics, but not enough of an evidence base to promote widespread adoption.” NEHI is working collaboratively with several organizations to develop that evidence so that hospitals will invest in tele-ICUs.
The Future of Connected Health
Among the more innovative research programs presented at the symposium was a joint program between RIM, the maker of the BlackberryTM PDA, with Toronto Rehabilitation Institute and Laurier University. Building on the GPS capability of RIM’s device, experts are working to develop an automated diary for daily activities in diabetics. The diary combines satellite tracking, digital pen technology, accelerometers, and other physiologic sensors to provide patients with feedback on their daily activity level and health status.
MassPro, the Quality Improvement Organization (QIO) for Massachusetts, is looking into electronic imaging and image transfer as a means of managing and monitoring pressure sores in nursing home residents, which put patients at risk for complications.

Investors in connected health talked in general terms about their strategies for investing in novel technologies. Nokia takes a consumer perspective and is interested in new software applications, particularly in the area of diabetes. Tyco is focused on products capable of integrating divergent systems seamlessly, while AstraZeneca looks for innovations that fall within the company’s “care mission” and align with key value drivers in connected health: convenience and the push for improved healthcare quality.
At the close of the symposium, attendees were encouraged to continue asking questions and challenge themselves to advance the cause of connected health through action and courageous investment. Speakers summarized practical suggestions forwarded during the event, such as engaging human resources managers to consider connected health-based wellness programs, approaching benefits managers at large self-insured companies, making proposals to CMS, and seeking multiple funding sources for new projects.
The dialogue generated at the symposium is continuing online. You can join the discussion at www.connected-health.org.
Joseph Kvedar is the founder and director of Partners Telemedicine, a division of Partners Healthcare that is applying communications technology and online resources to increase access and improve the delivery of quality medical services and patient care. Partners Telemedicine works with Harvard Medical School-affiliated teaching hospitals, including Massachusetts General and Brigham and Women’s Hospitals. Kvedar is also a board-certified dermatologist and vice-chair of dermatology at Harvard Medical School.
In his role with Partners Telemedicine, Kvedar launched the first physician-to-physician online consultation service in an academic setting. He is also leading important research into novel approaches for telemedicine in a variety of medical specialties, including post-operative care in the home, wound care, and remote monitoring of patients with chronic diseases. In establishing the new Connected Health Initiative, Kvedar is bringing together a number of collaborators from technology, healthcare, and academic organizations to create a more patient-centered healthcare delivery system using communications technology.
Kvedar is a past president of the American Telemedicine Association (ATA) and is chair of the American Academy of Dermatology (AAD) Task Force on Telemedicine. Kvedar may be contacted at jkvedar@partners.org.
