Digital Health: Using Technology to Improve Patient Care
By Cristina Vaz de Almeida, PhD
Opportunities in digital health (WHO, 2020) have been revealed to be self-evident in this pandemic, as well as opportunities to meet the Sustainable Development Goals (SDG) related to health and well-being. All health organizations must make the effort to provide digital applications for their patients (WHO, 2020).
Digital health requires the effective involvement of health professionals, whether for telemedicine, video conferences, or mobile applications for consultations, screenings, or follow-up. To their credit, when the pandemic hit, hospitals and care units acted immediately in response to this need to maintain collaboration and care for their patients.
By themselves, health professionals have the technical value of their expertise, but their role is strengthened by the involvement of top leadership (Brach et al., 2012). This is the general principle that underlies health-literate organizations (Brach et al., 2012).
Top managers must be strongly involved in health literacy strategies (digital and non-digital) and pass this perspective on to their teams in their planning, development, and implementation of any activity, including also their final recipients (i.e., patients).
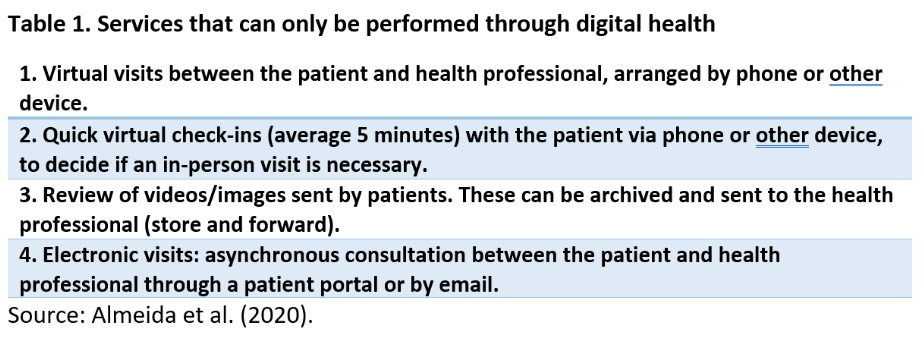
Digital health solutions can revolutionize the way people access services, strengthen their health and well-being, and achieve higher health standards (WHO, 2020; Table 1).
There are several examples of success in healthcare organizations through the use of digital media. We evoke here the relational model of health communication competence (Kreps, 1988), represented graphically by a wheel with axes (spokes), in which the center of the wheel represents the patient and the spokes represent the various healthcare providers (e.g., health professionals, organizations, other related services). Through the interdependent roles of each provider, a level of relational communication (Kreps, 1988) between professionals and patients is generated in the wheel, and digital tools can help keep that wheel spinning.
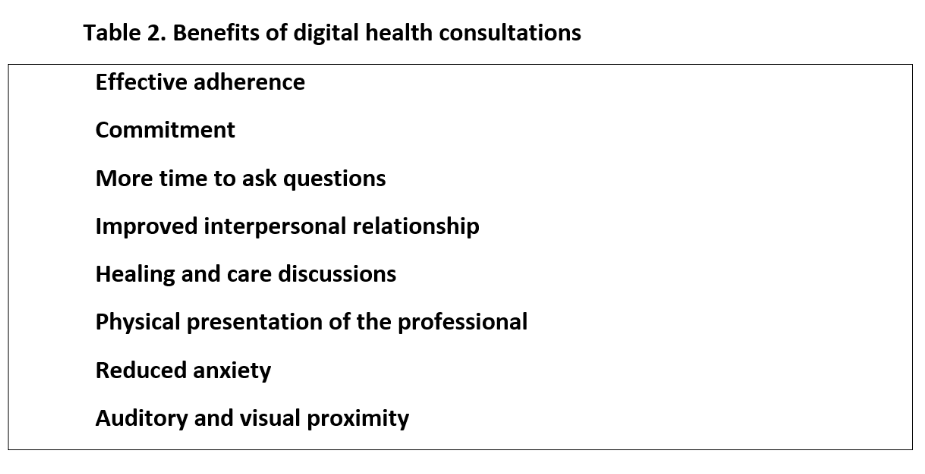
Even in cases of people with low reading and comprehension skills, mobile phones are one of the most useful tools to establish proximity with the patient, as seen in two large hospitals in Lisbon, Portugal. These follow-up “teleconsultations,” either with patients with low vision at the Gama Pinto Ophthalmological Institute (IOGP) or patients at the Central Lisbon Hospital Center (CHULC), were organized by nurse Susana Ramos and performed by both a doctor and a nurse. They showed that digital proximity tracking allowed for effective adherence, patient commitment, satisfaction with contact, decreased anxiety, feelings of closeness, social connection, time to ask questions, and a generally improved state of mental health.
Patients used to online health services, on the other hand, yearn for a frictionless health experience (Change Healthcare, 2020). These patients want to have more capacity to access services, make an appointment online, ask for follow-up, ask questions with direct answers, and pay for the service in one place (Change Healthcare, 2020; Figure 1).
Figure 1. What do patients with greater digital literacy want?

Source: Change Healthcare (2020).
For these teleconsultations to have a better result in terms of patient adherence and follow-up, health professionals involved in these processes during the pandemic revealed that the consultations had to meet the principles of health literacy (Almeida, 2020). Along these lines, the health professionals demanded greater adaptation to digital interaction with or without video, use of clearer language, and above all several repetitions of the information, given that “the more the message is repeated, the greater the probability of memorization” (Rodrigues, 2020). Through these techniques, used in the promotion of health literacy, patients have the opportunity to realize several benefits of digital health consultations (Almeida et al., 2020; Table 2).
Source: Almeida, based on Brach et al., 2012; European Commission, 2020b; Almeida et al., 2020.
Three pillars to support a digital approach
In Europe, the European Commission is working on ways to bring about a greater digital transformation for the benefit of all, including health professionals and health organizations. The European Commission highlights three guiding principles for an effective digital solution (European Commission, 2020a) (Table 3).
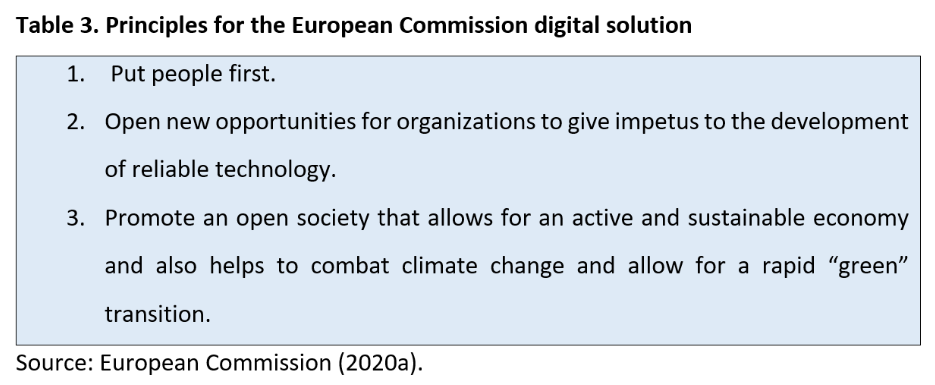
To succeed in digital health, the European Commission guidelines show that it is necessary to invest in digital skills, accelerate the deployment of broadband internet to private homes, and invest in the supercomputing capacity of innovative solutions for medicine.
Figure 2. Strategies for digital improvement
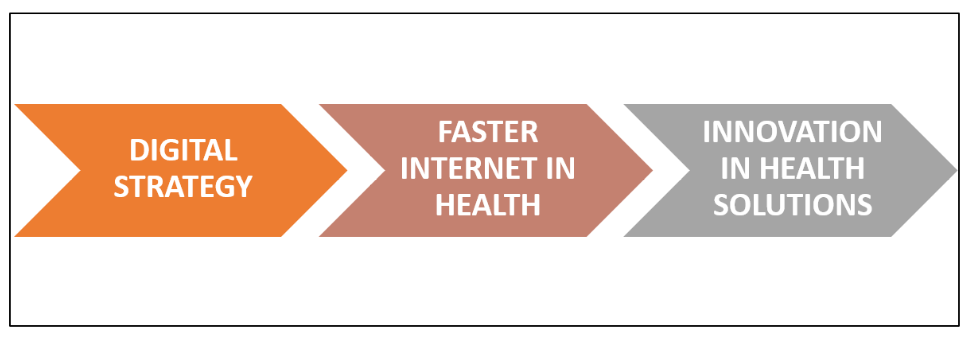
Source: Almeida, based on European Commission (2020a).
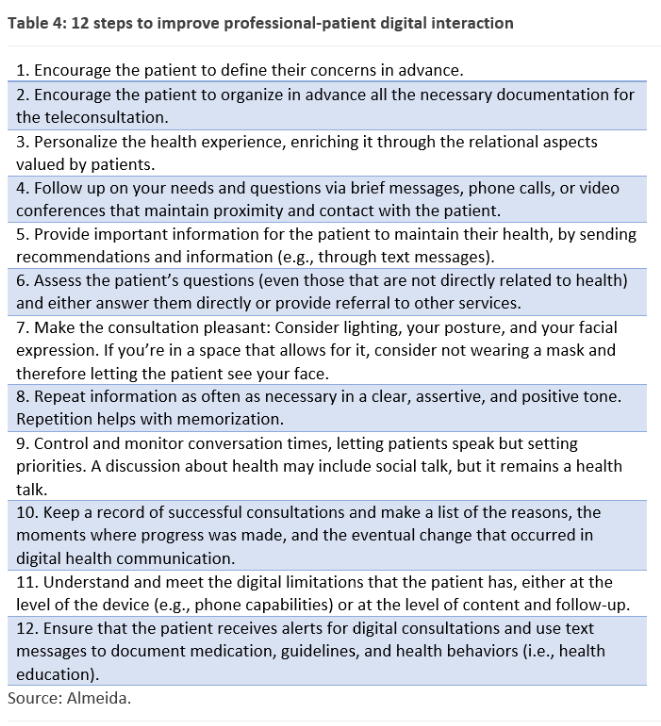
To make greater use of digital technologies and respond to the most immediate needs of digital health, professionals must become more qualified, including through training. In addition, patients need better and greater “advocacy” (Ramos, 2020) and support from organizations (Brach et al., 2012). Table 4 sets forth several steps that professionals can take.
The empowerment of citizens for better health literacy allows patients to better protect their health and contributes to the common digital strategy that benefits society as a whole (WHO, 2017). One way to do this is to create easy, assertive, clear, and positive means of passing on messages and specific actions for greater effectiveness (Bandura, 1999) in the use of digital health.
We recognize, however, that the health literacy level of the European population is low (Espanha et al., 2016). Half of Portuguese and European patients are unable to properly access, understand, evaluate, and use health information to make health decisions (Sorensen et al., 2012).
Since the COVID-19 lockdown began in March 2020, health organizations have started a reactive process of building digital solutions to maintain connection and continuity in the provision of health services. However, to truly reap the benefits of digital solutions, organizations’ move to digital health must ultimately be intentional, not reactive.
This voluntary scientific and technological leap by organizations, which is bolstered through a series of joint efforts between regulatory authorities and promoters of European funds (European Commission, 2020c), allows for more steps toward proactive improvement of health services; stimulates the promotion of research, diagnosis, and treatment; and helps with “combating online misinformation and promoting diverse and reliable media content” (European Commission, 2020a).
The increased use of technology in the face of the pandemic creates and reinforces other needs, so it is also necessary to have good legal support (Law of Digital Services) to regulate the provision of online services. In particular, attention must be paid to the protection of confidential data that healthcare organizations generate on a daily basis (European Commission, 2020a).
The European Commission is convinced that well-regulated health data can contribute to the common good (European Commission, 2020a). The data can provide clues—for example, through the reuse of health records or publicly available social data—that help in the development of personalized medicines or to advance research on cures for specific diseases (European Commission, 2020a).
Cristina Vaz de Almeida, PhD, is director of the Post Graduate Course on Health Literacy at ISPA in Portugal.
References
Almeida, C. V. (2020). Organizações literadas, literacia em saúde e boas práticas em tempo de pandemia – ao encontro dos Objetivos do Desenvolvimento Sustentável [Literate organizations, health literacy, and best practices in a pandemic – meeting the Sustainable Development Goals]. APDH. https://www.apdh.pt/artigo/67
Almeida, C. V., Moraes, K. L., & Brasil, V. V. (2020). Introdução [Introduction]. In C. V. Almeida, K. L. Moraes, & V. V. Brasil (Coords.), 50 técnicas de literacia em saúde na prática. Um guia para a saúde (pp. 8–12). Novas Edições Académicas.
Bandura, A. (Ed.). (1999). Self-efficacy in changing societies. Cambridge University Press. https://doi.org/10.1017/CBO9780511527692
Brach, C., Keller, D., Hernandez, L. M., Baur, C., Parker, R., Dreyer, B., Schyve, P., Lemerise, A. J., & Schillinger, D. (2012). Ten attributes of health literate health care organizations [Discussion paper]. Institute of Medicine. https://nam.edu/perspectives-2012-ten-attributes-of-health-literate-health-care-organizations
Change Healthcare. (2020). The draw of frictionless healthcare: 10 best practices for creating an outstanding digital patient experience. changehealthcare.com
Espanha, R., Ávila, P., & Mendes, R. M. (2016). A literacia em saúde em Portugal. Lisboa: Fundação Calouste Gulbenkian
European Commission. (2020a). New opportunities for digital health startups and SMEs. https://ec.europa.eu/digital-single-market/en/news/new-opportunities-digital-health-startups-and-smes
European Commission. (2020b). Shaping Europe’s digital future. https://ec.europa.eu/info/strategy/priorities-2019-2024/europe-fit-digital-age/shaping-europe-digital-future_en
European Commission. (2020c). Shaping Europe’s digital future – questions and answers. https://ec.europa.eu/commission/presscorner/detail/en/qanda_20_264
Kreps, G. L. (1988). Relational communication in health care. Southern Speech Communication Journal, 53, 344–359.
Ramos, S. (2020). Advocacia do paciente [Patient advocacy]. In C. V. Almeida, K. L. Moraes, & V. V. Brasil (Coords.), 50 técnicas de literacia em saúde na prática. Um guia para a saúde (pp. 14–18). Novas Edições Académicas.
Rodrigues, P. (2020). Repetição [Repetition]. In C. V. Almeida, K. L. Moraes, & V. V. Brasil (Coords.), 50 técnicas de literacia em saúde na prática. Um guia para a saúde (pp. 93-94). Novas Edições Académicas.
Sorensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health Literacy and Public Health: A systematic review and integration of definitions and models. BMC Public health, 12, 80.
WHO (2017) Patient empowerment can lead to improvements in healthcare Quality. Retrieved from: https://www.who.int/bulletin/volumes/95/7/17-030717/en/
WHO (2020). Digital health. Retreved from: https://www.who.int/health-topics/digital-health#tab=tab_1
