Designing Reliability Into Evidence-Based Practice
Manager/Practitioner Strategies & Tools for Reliability-Ingrained EBP
By Benjamin E. Ruark
I. Reliable Evidence-Based Practice (REBP) in Healthcare
Never will it be more obvious that medical practice labors under a hypocritical oath to first do no harm—primum non nocere. According to the World Health Organization, a majority of us should look forward to one diagnostic error in our lifetime. In high-income countries such as ours, one in 10 hospital patients will be harmed, though as much as 80% of that harm is preventable. As potential patients, seven of every 100 of us can walk through the hospital doors with the glum expectation of getting infected. If surgery’s in our cards, one in four of us can look forward to complications during or after our stay. And in any given year, between 44,000 and 98,000 of us won’t leave the hospital alive, according to the Institute of Medicine’s 1999 report, To Err Is Human.
On the sound foundation of evidence-based practice (EBP), healthcare providers rely on the most current and credible evidence to guide decisions; make diagnostic recommendations based on test results; prescribe effective medications; determine optimal care plans; and apply the best and safest practices for all manner of diseases and illnesses. However, EBP fidelity houses a set of glitches in an otherwise sound approach to qualitative practice: the human brain, human-designed standard operating procedures, human-operated systems and institutions, and a human-populated workplace culture. All of these things are flawed, failing even to mesh with each other—which is how implementation of EBP becomes rife with unexpected complications that threaten to delay, diminish, or negate patient outcomes.
In its Introduction to Patient Safety, the Institute for Healthcare Improvement nicely sums up healthcare’s contemporary dilemma in bullet points that are paraphrased here:
- Patient diagnosis and treatment carries inherent complexity
- There is, industrywide, an absence of well-integrated care teams, partially because healthcare professionals are inadequately trained to function cohesively
- Most errors can be attributed to flawed (unreliable) processes and systems of care; only a negligible amount are attributable to caregiver negligence and irresponsibility
- Safety cultures across the industry are unmistakably weak; a majority of organizations’ shared attitudes, beliefs, perceptions, and values surrounding safety are rudimentary at best
What we need is a cultural mindset of striving to be reliable in everyday medical practice. We need an operational focus that seeks to amend current practices to remove threats of deviation or setback from an action or procedure. To that end, human-factors safeguards must be embedded in all work; they are part and parcel of any performance because they ensure the task will be completed as intended. For whenever humans are involved, intentions don’t necessarily become reality, as will be demonstrated in the pages that follow. Accordingly, as a mindset, reliable evidence-based practice (REBP) is based on the informed understanding that human factors will otherwise predictably threaten the fidelity of practice driven by current research evidence.
II. Informed Understanding of the Human Brain’s Memory Systems in a Multitasking Workplace
To torture a phrase of Einstein’s, healthcare cannot resolve its quality and safety issues with the same level of thinking that produces them. In other words, healthcare’s present approaches to conducting work do not adequately accommodate the human brain’s sporadically incompatible memory systems. This quandary is compounded by work processes and standard operating practices that completely neglect human-factors principles, exacerbated further by discordant healthcare systems that are designed to make work happen.
No matter how closely a healthcare organization’s practices are aligned with research evidence, if its people and systems aren’t disciplined to provide consistent and stable healthcare delivery at both global and granular levels, the results will be unfortunate and unflattering—and borne out in patient outcomes.
Moreover, adherence to EBP implies a reliance on diagnostic, organ function, blood analysis, toxicology, and other test metrics to determine the best care for patients. By logical extension, the same depth of reliance should be afforded to human cognitive and physical performance metrics. The findings of research evidence on cognitive performance, human factors, and perception should equally and unfailingly guide the execution of all manner of evidence-based healthcare practices.
To get acquainted with the problems at hand, let’s take a glimpse at what we’re principally talking about: human memory. Of the eight types of human memory, we are mainly concerned here with short-term memory, also known as working memory (WM). WM gets a workout during task performance, only lasting a half-minute, but is continuously renewed. All other memory types represent a breakdown of long-term memory based on whether they are held in consciousness or unconsciousness. It’s helpful to think of different memory types as having discrete residences in the brain. Each type relies on its own neural pathways to shuttle abstract concepts, emotional experiences, episodic events, facts, procedures, and skills between regions of the brain. From this perspective, it’s also helpful to think of “memory systems.” The two systems that figure here, habit memory and prospective memory, represent two significant gateways through which human error can occur.
The habit memory system—residing mainly in the brain’s basal ganglia—refers to procedural and skill learning that, through repetition, can be performed without conscious intent: walking up/down stairs, starting the car, swimming, taking someone’s temperature, driving to/from work, etc. Any repetitive action, task, or skill is a prime candidate for conversion into a habituated or automated routine; this is what we mean when we refer to actions being performed on “autopilot.” A large portion of human behavior and skill sets are prime targets for habit memory.
Habit memory in healthcare affords caregivers great mental efficiency in performance of routine tasks because it avoids a huge drain on the WM load, or information capacity. It therefore poses great savings for getting through one’s harried workday. But of course there’s a rub: Distractions and interruptions (D&I) during any routine task break the habit memory “trance.” Additionally, the brain’s amygdala—which processes emotions—can exert a similar effect under conditions of high stress. In both instances, D&Is and stress, habit memory gets immediately sidelined by prospective memory. And for good reason.
Prospective memory—residing mainly in the prefrontal cortex (PFC) and hippocampus—is an ability to recall and execute some intention at an appropriate time or circumstance. The brain’s PFC is known as our “executive function.” Located just behind the forehead, it is our personal command center from which we consciously attend to matters and stay on task; shift attention at will; form intentions and make plans; retain immediate details of interest on our WM’s “sketchpad”; inhibit undesirable impulses; think abstractly; and retrieve long-term memories from the hippocampus.
Yet in light of prospective memory’s capabilities, any distraction has the power to throw a pivotal switch on our memory tracks: going from habit memory (basal ganglia) performance of a routine task to commandeering immediate focus (via the PFC) on the interruption.
The problem comes once we’ve dealt with that interruption. Since habit memory is unconscious, and our conscious PFC faculties have no access to unconscious activity, prospective memory is at a loss regarding what our habit memory was previously handling. We are literally stuck; we don’t know where we left off on whatever routine task was underway. So we must make our best guess—based on situational cues—as to which step we were on, which vital piece of information we were about to give, etc. Unaware of the regional brain infighting going on, we push ahead, attempting to complete our current task. And in doing so, we open all sorts of windows to human error. Hence the need for built-in reliability in healthcare practices.
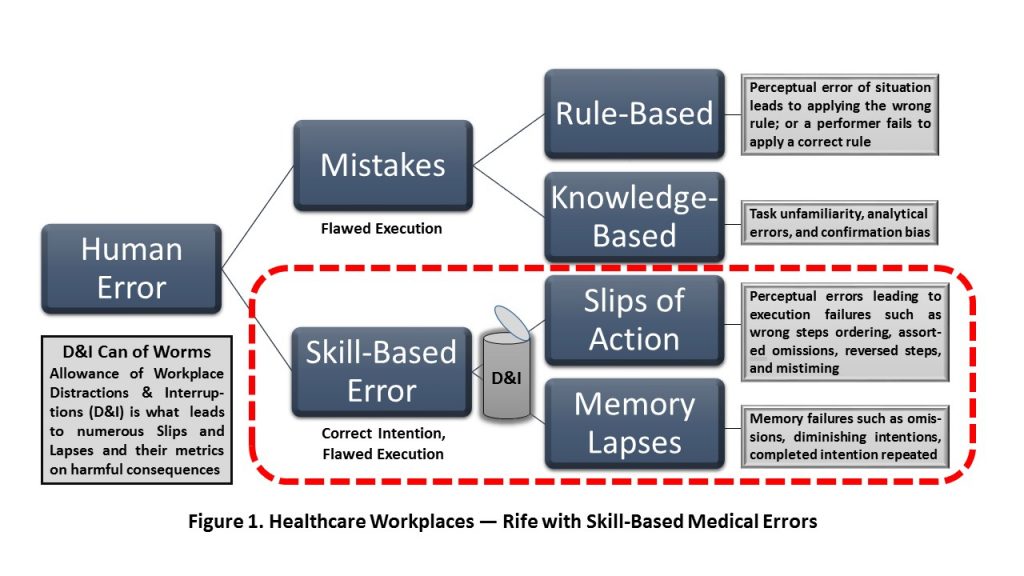
Figure 1 depicts how those unwanted D&Is that get confronted daily open a proverbial can of worms for incurring numerous action slips and memory lapses in healthcare practice. A slip occurs when we do something we didn’t intend (commission). A lapse occurs when we forget to do something we did intend (omission). General types of error are listed beside each of Figure 1’s two circled error domains. This paper’s focus is on the prevention or reduction of so-called skill-based errors (per human-factors classification).
A distraction unduly draws attention away from a task; it can be strong or weak, but it will not prevent the task from being completed. Sources of distraction include ambient noise from computers, conversations with patients, infusion pumps, overhead PA announcements, ringing office phones, socializing staff, alarms, clutter, lighting and computer screen glare, notification sources, portable devices, and telephone conversations. Noise is doubly troublesome since it is also considered a serious health hazard for patients; it adds stress and exacerbates various symptoms of disease and illness. Physical and mental distractions such as hunger, fatigue, illness, worry, and daydreaming can also derail a staff member.
In contrast, an interruption causes temporary or permanent cessation of a task before its completion. Sources of interruption include emergency/urgent action, face-to-face notifications, acquiring medications and supplies, putting in urgent requests, and looking for missing data, lab values, or urgently needed clarifications. One study notes ER physicians are interrupted every 10 minutes. Another study reports the risk of medication error increases nearly 13% with each interruption during medication administration; as it now stands, one patient dies every day from such errors. Since we cannot completely remove D&Is from healthcare settings, we need reliability-embedded countermeasures to eliminate the vulnerability to error that they create.
Healthcare’s penchant for multitasking—despite its many drawbacks—offers a third gateway for D&Is to introduce human error. One authority reports that multitasking, alone, can lower productivity by as much as 40%. Combined, the three gateways of 1) habit memory (in periods of no or light multitasking), 2) prospective memory (omnipresent), and 3) periods of heavy multitasking set up four classes of “forgetful conditions.” They are:
- Forgetting where one left off on a task (habit memory origin; high risk of omission)
- Forgetting to return to an unfinished task (cognitive tunneling origin; high risk of omission)
- Forgetting to perform an intended task when its time arrives (prospective memory origin; medium (presumptive) risk of omission)
- Forgetting that a task was previously completed (prospective memory origin; low to medium (presumptive) risk of commission)
Exactly what produces prospective memory failures is less obvious; likely there are multiple causes. In one study of it, researchers report 25% of participants made errors of commission. As for cognitive tunneling, aka cognitive capture or inattentional blindness, it’s a psychological phenomenon whereby a person’s concentration on a demanding task (or under high-stress conditions) gets fixated on a single category of information, say on another patient. It does so at the exclusion of various salient information and stimuli in plain sight, such as previously attended-to patients with uncompleted needs who are still awaiting aid. This is definitively dicey, especially when staff are attempting to multitask and administer care to many patients at a frenzied pace. Such operational states can only magnify risk.
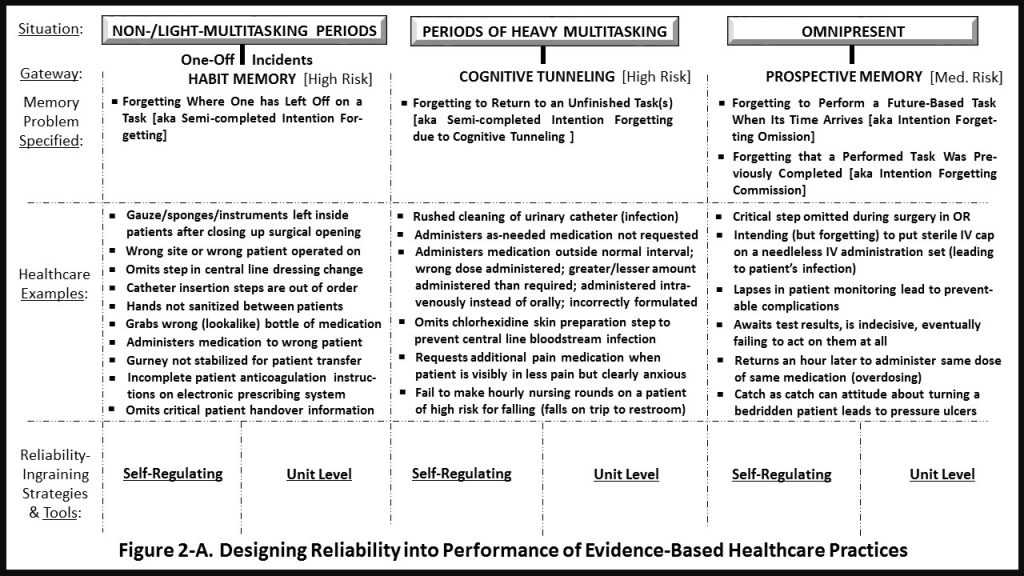
Figure 2-A depicts the two memory systems with multitasking sandwiched between them. The four classes of forgetful conditions are shown as well, along with representative healthcare examples of errors of omission and commission. At the core of this framework is the notion of conscious intent: the idea that we routinely generate both current and future intentions (a PFC function). Approximately 15% of our wakeful thinking is devoted to planning and completing intentions. More important is how those intentions interact with the aforementioned memory systems: leaving in their wake semi-completed tasks, future tasks possibly forgotten, and completed tasks erroneously repeated. Reliability safeguards will appreciably negate this heretofore unchallenged presence, which we know is ubiquitous throughout healthcare.
III. Strategies & Tools for Reliability-Ingrained EBP
The smart move would be to prohibit from practice all habit memory–dominant performances of routine tasks, with staff remaining continuously consciously (PFC) engaged instead. That could be achieved, though of course it would require more frequent and perhaps longer mental rest breaks. But habit memory has at most a small place in healthcare, just as it is shunned in aviation and petroleum exploration. These industries assess risk of harm and life among workers as unacceptably high. With healthcare rejecting such a mandate, we press on.
It doesn’t matter whether multitasking is occurring, or whether staff are working at a frenzied or mild pace: D&Is have the same capacity to derail WM and encourage errors of omission and commission, carrying varying degrees of consequences for unsuspecting patients. Forgetfulness does not correlate with IQ or education level, but it does relate to signs of arrogance, apathy, and presumed impunity insomuch as those who demonstrate such traits are more apt to err repeatedly and willfully. Thankfully, such practitioners are few in number, and the majority of healthcare professionals would relish opportunities to keep forgetfulness at bay. The way to do that is through strategies and tools designed to cut a wide berth around memory lapses and action slips. Sixteen categories of these, ranging from unsophisticated to elaborate, are at healthcare practice designers’ disposal, and they are shown in Figure 2-B.
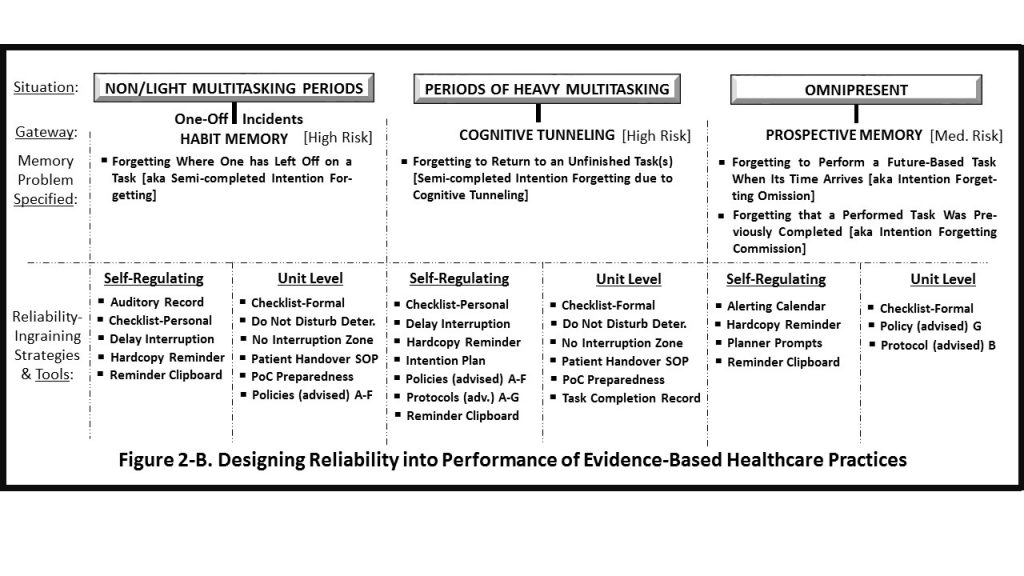
- Electronic calendar alerts – Both mobile and desktop platforms support programmable alerts and notifications to remind staff of tasks to be performed (automated prospective memory aid).
- Auditory record – We can call out the last step performed in a task when a distraction or interruption occurs. In doing so, we create an auditory-memory record, likely doubly recorded as others also hear it. (This is the same logic used, even subconsciously, by people who read phone numbers aloud: Doing so records both with their WM and their sensory memory.) There’s actually an extra scratchpad at hand: jotting down a last step performed on scrap paper, the sleeve of a gown, or the back of a glove.
- Call notification transfer – As approved, staff can notify coworkers to complete an interrupted task when the person who began the task is needed elsewhere—contingent on not introducing a delay in care, and on coworker availability. By either electronic means or face to face, the transfer is accomplished and the coworker is informed of the last step performed.
- Checklist adherence – There are two kinds of checklists: those for personal use and those for formal (unit) use. One study of 17 operating teams found they were 74% less likely to miss critical steps when checklists were applied; when operating without a checklist, 23% of the steps were omitted on average, and even with a checklist, 6% of the steps were omitted. Applied with fidelity, checklists can effectively thwart habit memory omissions and prospective memory commissions.
In truth, arrogance and checklist usage are inversely related. Topping that, look no further than a work culture’s view on performance overall: Does it think in terms of regulatory adherence, reactively preoccupied with what not to do? Or does it proactively concentrate on pursuing accuracy and consistency in all actions? Any management consultant worth their salt can tell which of these operational mindsets is in force within an hour of their visit to a customer site.
In a study of nurse adherence to standard medication administration, 6.5% read the patient’s name from a wristband; 41% administered medication at the correct time; just 4.5% consistently performed handwashing before giving oral/external medication; and 45.6% verified the amount of medication in a vial. Among all adherence categories, an average of 5.7 items were violated.
- Delaying the interruption – There are two options, based on the task: (1) Continue the present task up to the conclusion of one of its distinct subtasks; or (2) continue the task up to a natural break point where the next step is obvious. (Consider marking off subtasks/break points in all critical tasks as “officially sanctioned points of departure.” Post this codified display for quick reference prior to executing designated tasks.)
- Do not disturb – Facilities can use various interruption deterrents such as aprons, sashes, and vests that are color-coded (with staff educated on what the colors mean) or lettered with “Do Not Disturb” or a similar warning. One study of this strategy showed significant reduction in related medical errors following incidents of interruption.
- Hard copy reminder – We can post a task-reminder note in a location where it won’t get lost, covered over, or removed (it will serve as a prospective memory cue for an intended task). The note could even be posted at the point of care, observing the same caveats.
- Intention plan – Also known as an “if-then” plan or implementation intention, this concept is originally associated with research literature on goal pursuit and attainment. But it has application in healthcare and much resembles the hard copy reminder we just discussed. A meta-analysis of over 100 studies found a medium to large effect size in the significance of attaining goals through reliance on if-then planning processes.
The goal aspirant says something to the effect of: “When situation C arises, I will T at __________.” The C denotes cues highlighting the situation/context/person needing a specific task to be performed; the T denotes an abbreviated name for said task; and the blank space denotes the location. Hence, we have a rich assortment of formula-studded cues to aid prospective memory. In fact, this arrangement enhances memory automaticity: instances of naturally remembering to engage in some intended task without any external aid. Based on implementation intention research, however, this memory tool is most successful if buoyed by strong personal commitment to satisfy some intent.
9. No interruption zone (NIZ) – Once staff are duly informed, care units can post NIZ placards in certain areas to avert distractions and prevent interruptions. According to Matthew Grissinger’s seminal 2012 article “Sidetracks on the Safety Express,” prime locations for NIZs may include automated dispensing cabinets, computer order entry stations, drug preparation stations, and laminar flow hoods.
10. Patient handovers – At shift change and other handover occasions, units are advised to adopt a consistent approach, such as SBAR or I-PASS. One study noted that interruptions occurred 31% of the time for all types of staff communications. One remedy would be to simply raise a hand in a “stop” gesture to prevent staff from interrupting until all instructions, etc., have been handed over. Or staff could simply say, “Let me finish up here.”
11. Planner prompts – These are self-made forms with key fields for filling in the who, when, where, task, and date/time, for every nth time period. This prospective memory prop is used to self-regulate monitoring of various patient symptoms, both developing and developed.
12. Point-of-care preparedness – This concept discourages self-interruptions. Supply all necessary aids, instruments, and materials at the point of care, then adjust and operationally test all equipment for immediate use prior to starting an intended task. This is a prospective memory–friendly strategy.
13. Policy setting – For each of the following, consider a unit-level policy:
- Limit alarms, ambient noise, computer alerts, and allowable uses of the PA system.
- Assign crucial tasks as top priority, as feasible, during slack periods.
- Identify a designee and assign a contingency strategy for complex procedures whose key personnel are at risk of being temporarily or permanently redirected.
- Implement a “no multitasking” designation where a caregiver must stay on task.
- Ensure no patient question or request goes unaddressed or is handled in an untimely manner. Identify instances where current staff responsiveness needs immediate improvement.
- Prohibit self-initiated D&Is. Discourage daydreaming, personal use of electronic devices, and conversing socially while routine work is performed.
- Where feasible, devise surefire preparatory monitoring strategies as policy for intended tasks of medium importance. Preparatory monitoring involves scanning for a target event: something not planned for, yet expected to occur, such as a change in a patient’s condition; which hints at being a prime target for some intended action.
14. Protocol setting – For each of the following, consider a unit-level protocol:
- Instruct staff to avoid interrupting staff members who are performing designated do-not-interrupt tasks.
- Design communication redundancy to guarantee timely handoffs of critical information and ensure all need-to-know parties are contacted.
- Implement computerized decision aids as needed.
- Simplify and standardize procedures of care for pressure ulcers, catheter insertions, dressing changes, IV insertions, and tracheotomy care.
- Devise solutions for differentiating between lookalike/soundalike medications.
- Conduct SOP (periodic) staff evaluations with remedial instruction refreshers to prevent memory and/or skill “drift.”
- Mandate individual staff training on equipment changes/upgrades.
15. Reminder clipboard – A custom-designed multipurpose pad (paper or electronic) can contain a practitioner’s own selection of categories and shorthand abbreviations. Here they can also jot down salient information, to-do items, and informal recordings of potentially important observations and incidents.
16. Task completion record – An electronic/hard copy form (or checklist format) can be used to capture completed tasks’ date and time. It could represent all tasks, or focus on ones with a tendency to be repeated during periods of heavy multitasking.
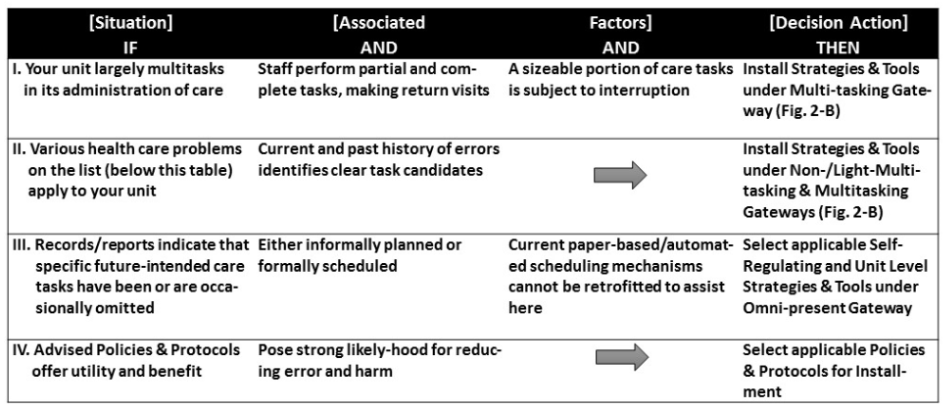
IV. Recommended Reliability Design Steps
The goal is to assign, equip, and apply as many reliability-enabling strategies and tools at the individual (self-regulating) and unit level as possible, with staff education in close pursuit. In appropriate instances, staff could practice scenarios to establish familiarity (called priming). Moreover, peer coaching should be instituted, with supervisory random spot checks also filling the organizational change need. Staff ideally begin to think and act “reliably,” on their feet, to the point of reliability becoming second nature. A decision table, below, affords a navigable design process for managers and practitioners, and their assigned task force or committee, to use as a launchpad for the REBP transformation process.
Common Healthcare Problems List
Adverse drug events Burns Equipment changes/upgrades
Prophylactic treatment Falls Patient handovers
Improper transfusions Infections Misdiagnoses/delay in diagnosis
(1 in 25 patients)
Inappropriate test chosen Failure to act on lab results Mistaken patient identities
Pressure ulcers Deep vein thrombosis Radiation errors
Restraint-related harm Retained foreign bodies Surgical injuries
(12.5% of all surgeries) (4,000 surgical errors/year)
Unsafe injections Wrong-site surgery
(40/week nationwide)
Traditional healthcare practices, despite a robust injection of EBP, remain suboptimal. As things stand, individual variation in perception, memory facility, work attitudes and ethics, and professionalism makes it difficult if not impossible to keep practice consistent, stable, and dependable. With regard to a majority of errors, if “fault” applies, it lies in the neurological pathways and uncommunicative memory regions of the human brain.
Sadly, we’re not like a computer’s relational database, allowing access to the same data point or string of information from multiple memory locations. Instead, our brain possesses evolved components similar to those in the brains of fish, reptiles, and of course other mammals. These components are all connected, and they operate pretty amazingly overall—but not to the extent we’d prefer. Embedding reliability in healthcare practice will work to make up for the shortcomings of our brains, and impose the necessary formal boundaries that we can agree the industry lacks.
Benjamin E. Ruark is a former learning & development and continuous quality improvement professional. He now devotes his time to writing on important subjects for various industries, healthcare included.
