Design for Reliability: Barcoded Medication Administration
July / August 2011
Design for Reliability: Barcoded Medication Administration
There is now widespread agreement that hospital patients can be harmed by medication errors. Providing patients with medications in the acute care setting is a complex process that requires coordination in the flow of information when individuals order, transcribe, verify, dispense, and administer a medication. Early studies quantified the extent to which errors occur at each of these stages; one of the most troubling steps in the process is the administration phase, when 26 to 38% of the errors occur (Bates et al., 1995; Leape et al., 1995). The majority of these errors are related to the nurse giving the wrong dose, the wrong medication, or missing medication altogether (Cochran et al., 2007). Further, it has been described that errors at the administration phase are likely to reach the patient since there are few safeguards in place to intercept the error before it is passed onto the patient (Bates et al., 1995; Douglas & Larrabee, 2003). Therefore it is critically important to patient safety that hospitals focus on building reliability in this phase of the process.
One strategy to reduce medication administration errors is barcoded medication administration (BCMA). Many institutions have adopted this technology as a computerized support system for nurses who are responsible for administering medications. Barcode technology has been an indispensible advancement for patient safety as it permits clinical staff to identify individual patients and their prescribed medications with increasing accuracy. BCMAs help confirm the five rights of medication administration: right patient, drug, dose, route, and time. BCMA technology involves placing a unique identifier (barcode) on each unit-dose of medication and the patient armband so that each can be read by an optical scanner. The nurse can safely administer the medication if the two barcodes match the drugs ordered and listed on the patient profile. Patient identification is confirmed with a barcode scan of the armband. Medication identification is confirmed with a barcode scan of the medication. But if the two scans do not match, then there is an alert that cautions the nurse about giving the medication. A recently published study by Eric Poon and his colleagues at Brigham and Women’s Hospital demonstrated a 41.4% relative reduction in medication administration errors using this type of system (Poon et al., 2010). Several other authors report significant reductions in medication errors from barcoding technology (Franklin et al., 2007; Neuenschwander et al., 2003; Patterson et al., 2002).
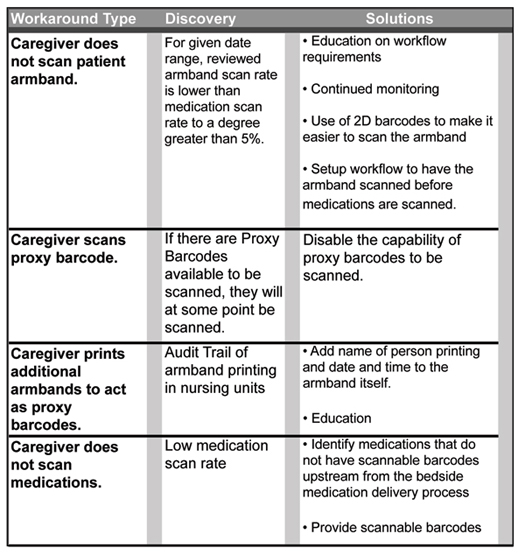
While the BCMA systems show tremendous promise, there are limitations and failures that must also be noted. A 2002 ethnographic study by Emily Patterson and colleagues distilled a number of unintended consequences inherent in the interactions between nurses and BCMA and outlined five that were likely to create medication errors: automation surprises, degraded communication between nurses and physicians, dropping parts of the process due to high workload, anxiety around timing of med administration, and decreased ability to deviate from the sequence (Snyder et al., 2010). Others have highlighted the propensity for technological failures due to scanner misreads and barcode errors (Douglas & Larrabee, 2003; Koppel et al., 2008). Koppel et al. studied BCMA at five hospitals and identified 15 types of workarounds, where nurses deviate from standard procedure due to deficiencies in the workflow design. They concluded that these deviations from safe-use protocols often are the result of sub-optimal design of the system and that unless the BCMA system was well understood and the problems addressed in situ, workarounds were likely to plague medication administration systems (Koppel, 2008).
The consensus for the moment is that the benefits of BCMA outweigh the risks, but that BCMA systems need to be implemented as highly reliable systems. In the conclusion section of their 2010 paper on the benefits of BCMA in the reduction of medication errors, Eric Poon and his colleagues recommend that “further research should focus on identifying factors that lead to optimal implementation” (p. 1712).
With that in mind, we turn to reliability science to look for ways to optimize processes. The Institute for Healthcare Improvement (IHI) teaches that reliability is the failure-free operation of a process over time. Healthcare presents a particular challenge to reliability in that many of the processes have evolved over time (not deliberately designed) and that process variation is widely tolerated (Resar, 2006). The IHI has developed a 3-step methodology for building reliable processes:
- Identify the process to standardize, articulate the key process metric, and understand the critical failure modes.
- Identify low performers; redesign parts of the process to overcome their barriers to success.
- Foster an atmosphere of continuous improvement by recognizing and mitigating failures, which begins with an intentional design to standardize a process so that it is performed in the same manner 80 to 90% of the time.
These early design efforts should not get overly bogged down in designing a process to address every contingency or to achieve error-free operation right from the start. Instead, the effort to achieve higher levels of reliability occurs in subsequent process rapid improvement cycles (RCI) where efforts are made to continually identify and mitigate process failures. It is important to point out that the improvements in the RCI phase of process design are typically quite different than those that were identified at the outset of the project and include such things as defaults and decision aids that go beyond humans having to remember something.
One of the keys to reliable design is the identification of a process metric, which enables the design team to readily identify failures and defects in the workflow. Hospitals typically examine outcome data associated with BCMA systems—how well the system reduces the rate of medication errors. Given the attention of late to workarounds and optimal implementation of the system in the real world, it is imperative that hospitals also take stock of process measures. One such process measure is the effective scan rate. Where hospitals have published scanning performance measures, we note scan rates of 85 to 90% (Galvin et al., 2007; Paoletti et al., 2007). This means that 10 to 15% of the time, the scanning is ineffective and nurses are working around the safe-use scan system in order to administer medications. This seems like an unacceptably low level of reliability for effective barcode scanning.
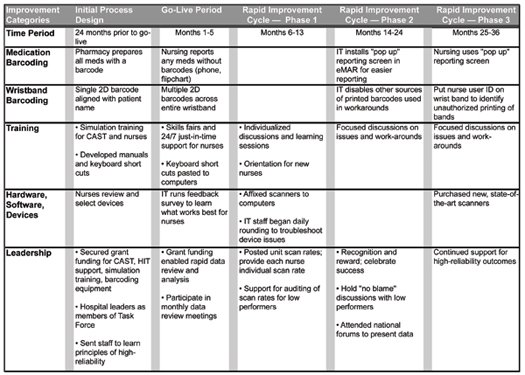
With urgency similar to that of other hospitals, Southwestern Vermont Medical Center (SVMC), a 99-bed, rural, acute care hospital, decided to implement a BCMA system. With funding assistance from the Agency for Healthcare Research and Quality (AHRQ), our hospital was able to focus intently on building the infrastructure necessary to move from paper to electronic medication administration records. Using the IHI model of reliability, the design team put in place a process measure—barcode scanning rates—that was used as the means to identify the failure modes of BCMA in situ. We believe that our success with this is worth sharing with other hospitals because we have achieved a level of reliability in barcode scanning that is among the best in the country. This article uses the framework of reliability theory to describe our 36-month experience of improving barcoded medication administration scan rates.
Methods
At the outset of our project, SVMC formed an interdisciplinary team called the eMAR Task Force, which was lead by a clinical nurse specialist and made up of nurses, pharmacists, IT analysts, nursing leaders, and a patient safety specialist. The team adopted a core philosophy, which became the central focus of all improvement decisions: make it easy for the nurse to do the right (safe) thing. Several nurses were given specialized training in informatics and served as the Clinical Application Support Team (CAST) to “bridge” between the realities of the clinical and IT domains (Novak & Lorenzi, 2008; Ash et al., 2003).
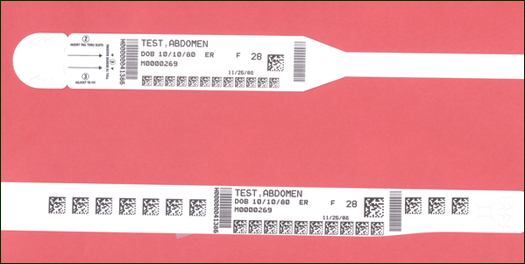
The team spent 2 years planning the transition from paper to electronic medication administration—focusing its activities on establishing barcodes for both the medications and the patient armbands. Perhaps one of the biggest breakthroughs of the initial design phase was the realization that the standard linear barcodes produced an unsatisfactory scanning experience for the nurse at the bedside. Their feedback was that the linear barcode was curved around the patient’s wrist and therefore difficult to scan. It required the nurse to free up one hand in order to stretch out the linear barcode, which created delays and out-of-sequence work. It often required that the patient had to be awakened during sleep so that the wristband could be scanned. The team decided to adopt a 2D data matrix barcode to rectify the problems brought out during the testing with linear barcodes. The IT personnel replaced the linear patient armband barcodes with an innovative 2D data matrix technology that, when trialed by the nurses, was easier to scan because nurses no longer needed to free up both hands in order to stretch out the length of the linear barcode. Figure 1 (pg. 12) displays the original linear armband prototype (right) and the redesigned armband with 2D barcodes. Nursing personnel engaged the attention of all hospital nurses in the trial and selection of hardware and scanning devices along with simulation training for every end user.
SVMC has four inpatient nursing units. The strategy for bringing the BCMA system on line was to do it one unit at a time, with 2 weeks of intensive engagement from the CAST nurses, who were on the units 24/7 to provide just-in-time instruction and troubleshooting. To minimize use of the keyboard and create a more continuous process for the nurses, IT created barcoded keyboard short cuts that were affixed to the computer workstations. These allowed the nurse to respond to eMAR prompts with a scanned response versus a keyboard stroke.
The focus of the Task Force at this phase was to get the process right—knowing that if the process was working successfully, then the outcomes (reduction in medication errors) would likely follow suit. Consistent with the tenets of reliability science, the team identified a process metric for the project: the scan rate. The justification for this is that if the nurse is not scanning either the patient armband or the medication (or both), then s/he is bypassing the safe-use features of the BCMA system. The team set up systems where nurses could report any and all scanning failures. Nurses were encouraged to contact the pharmacy whenever they came across a medication that could not be easily scanned. It was discovered that items such as multidose nitropaste tube, needed to have a portability option. This involved generating flag labels on the large tube so that the nurse could remove one label to take with the product to the bedside. IT personnel conducted a survey of the scanning devices and based on what they learned, they modified the patient wristband so that the 2D barcodes would be accessible to the optical scanner from any angle (see Figure 2). This innovation made it much easier for the nurse to have a successful scan when the patient was sleeping or the armband was partially covered by clothing or equipment.
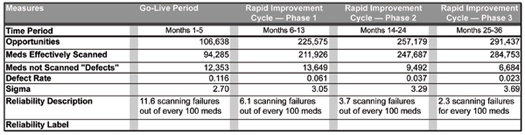
This phase of the project lasted 5 months, until each of the four nursing units was completely electronic. During this period, the nurses administered 106,638 medications and of those, 13,223 were administered without being scanned (88.42% scan rate; 11.58% failure rate).
Although other hospitals were reporting scan rates of 85 to 90%, the Task Force felt that higher rates would indicate a more reliable and safe process. After the go-live period, the members of the Task Force did not need to be on the units, so they established a series of weekly meetings to review scan-rate data, to identify barriers, and discuss in situ observations—all with the purpose of mitigating the failures. The specific metrics the team analyzed were: a) patient armband scan rate and b) the medication scan rate. At each Task Force meeting, the team leader posted both sets of scan rates by department and then drilled down into the data so that the lowest individual performers could be identified by name. Each nurse’s medication scan rate performance was analyzed via standard deviation within his/her peer group. This quickly identified those individuals who were outside of statistical norms for their unit. It might also identify situations where a specific medication barcode was substandard. This methodology enabled the Task Force to differentiate individual versus systemic failures and address them accordingly. All efforts focused on mitigating these failures. Additional improvement efforts at this phase involved posting scan rates on each unit along with a report to each nurse with his/her individual scan rate. At this phase in the improvement activities, the team sought to celebrate the overall success of the project; leadership held pizza parties, “good catch” stories were posted on the units, and graphs showing the hospital-wide scanning rate were posted in prominent locations. The team made a decision to accentuate the positive. Certainly the project scan rate data was moving in a positive direction, now at a 93.95% scan rate (6.05% failure rate) for 225,575 meds.
Phase 2 encompassed a full 12 months of work and brought scan rates to a new level. The leadership continued to review the scan rate data for each nurse; those who continued to have lower rates than their peers would engage in a “no blame” conversation with the clinical nurse specialist (CNS) from the unit. The purpose of this discussion was to identify and understand the barriers to scanning; the CNS brought the compiled list of barriers to the team meeting so that rapid action could be taken to mitigate the problems, with the goal of bringing the lower performing nurses in line with their peers. As identified in Koppel’s recent taxonomy of common BCMA workarounds (2008), the team members observed medication passes on the nursing units and worked to spot these in situ. Each workaround was discussed at the weekly meeting, and the IT analysts figured out a technological “stop” to that activity.
Sometimes the team learned that these coaching sessions resulted in nurses who sought to raise their scan rate even if this required by-passing the safe-scan system. The downside of setting a process metric is that human beings will figure out ways to thwart the aims of the measurement system. When a nurse was confronted with a bad scan rate, she could respond by scanning auxiliary (admission) labels instead of the official barcoded patient armband. The Task Force adopted a surveillance program for workarounds to identify instances where this was happening. The continued observation of this workaround led the team to modify all auxiliary labels so that they were incompatible with the BCMA system. The goal was to make doing the right thing the easiest thing—and with that in mind, unsafe use of the technology was not tolerated.
Table 1 lists the four workarounds identified during the SVMC project and the methods of discovery and mitigation. In addition, the IT analysts, created a field within the eMAR system that enabled a nurse to quickly report the reason for a failed scan—these reports were also reviewed at the team meetings. At the conclusion of Phase 2, the scan rate increased to 96.31% (3.69% failure rate) for 257,179 medications.
During this phase, the team continued efforts to identify and mitigate failures, but used a tighter threshold. The most significant technology change at this time was the purchase of state-of-the-art optical scanners, which were more sensitive in reading the barcode symbology. At the time this article goes to press, the leaders have put forward a goal of having a 99.5% scan rate. The Rapid Improvement Cycle phases of this project spanned from 2008 to present. Table 2 displays the various and continued improvements that the team put in place in order to increase the rate of successful barcode scanning.
Results
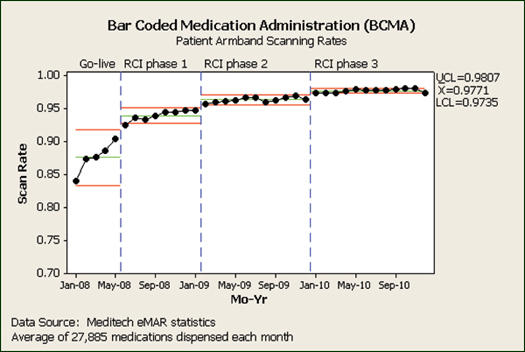
The performance metrics that show the results for each improvement phase of this project are displayed in Table 3. The successful medication scan rate increased from 88.42% to 97.71% over 36 months. Figure 3 displays the same data in a control chart, which captures the statistical significance of each bump in the scan rate.
This interdisciplinary improvement project, which has spanned more than 3 years since the go-live date, included a phased implementation of a bedside medication verification program using barcoded patient wristbands and medications. This scanning process is but a part—albeit an important part—of the hospital’s move to an electronic medication administration record. The hallmark of this effort was the team’s desire to stay with the improvement activities and not give in to the feeling that the process was “good enough.” Our success in achieving a scan rate of 97.71% is attributed to four key aspects of our methodology:
- Standardizing the initial design and aiming for a modest 88% medication scan rate during the go-live period.
- Identifying a process metric that was relatively easy to measure and allowed for identification of poor performers.
- Becoming obsessed with failures and reviewing data at regular intervals to identify and mitigate these failures.
- Listening and learning from the poor performers.
The first 5 months of this project were considered the go-live period, where each nursing unit was converted from paper to electronic MAR. This period involved a good deal of support and just-in-time training to ensure that the basic mechanics of the new system were in place and that nurses could adjust to the new work flow. In the 8 months following that, the Task Force began surveillance of scanning data to identify those nurses who were having the most difficulty with the new process; individualized coaching helped improve the scan rates to 94%. These rates were higher than anything we had seen published, but the Task Force was not comfortable knowing that 6% of the time, the meds were not being scanned correctly.
SVMC’s ability to develop and sustain a reliable scanning process for BCMA may serve as a model for other healthcare institutions as they embark on electronic medication administration programs. We recommend that other hospitals that seek to reduce medication administration error rates through BCMA embrace the concepts of reliability science. We recommend that design teams establish a process metric—perhaps scan rate—in order to identify process defects. We encourage teams to assiduously focus on failures because each failure identified and understood can then be fixed. We caution that the metric of scan rates can put pressure on nurses to develop workarounds, in an effort to keep their scan rate high enough to go undetected. To that end, we advocate for periodic in situ observations to both solicit feedback and detect workarounds. And lastly, we suggest that hospitals prepare to resource BCMA project teams with at least 24 months of dedicated effort to complete a series of rapid improvement cycles.
In April 2011, Southwestern Vermont Health Center (SVMC) received the Way-Paver Award for Patient Safety Initiative at the unSummit for Bedside Barcoding (www.unsummit.com) for the BMAC project described in this article. Shown above (l. to r.) are Diana Daniels, RN, who gave 6,681 medications with scan rates of 99.24% (medications) and 99.54% (patients) over 12 months; Charles Still; Barbara Richardson, MS, RN-BC, CCRN, clinical nurse specialist at SVMC; and Edward Lanoue.
The authors work at Southwestern Vermont Medical Center (SVMC) in Bennington, Vermont. Avis Hayden is a patient safety and quality specialist and may be contacted at hayav@phin.org.
Edward Lanoue is an informatics pharmacist in the pharmacy department and may be contacted at etl@phin.org.
Charles Still is a project manager of information systems. He may be contacted at stich@phin.org.
Acknowledgment
This project was supported by an HIT demonstration grant through the Agency for Healthcare Research and Quality.
We would like to thank the members of the eMAR Task Force for all their thoughtful reflection about the timing of their rapid cycle improvements. We also want to express our gratitude to Billie Lynn Allard, Alex Heintz, and Barbara Richardson for their assistance in editing earlier drafts of this article.
References