Decision Support and Clinical IT: Improving Safety in Obstetrics with Decision Support and Clinical IT
January / February 2006
![]()
Decision Support and Clinical IT
Improving Safety in Obstetrics with Decision Support and Clinical IT
Ensuring consistency of care and patient safety can be especially challenging in obstetrics — a complex specialty with unpredictable patient loads and nursing shortages. In addition, the expectations of the OB patient are arguably higher than those of patients in other areas of a hospital; each mother expects that her pregnancy will result in the delivery of a perfectly healthy baby.
Sainte-Justine, one of the leading institutions for maternal-fetal and pediatric medicine in Montreal, is well aware of this challenge. Their obstetrics department handles nearly 4,000 births each year and provides consultancy services for several thousand more through affiliated centers across the province. As the first step in a program to optimize patient care and safety, Dr. Robert Gauthier, a clinical professor in the Department of Obstetrics and Gynecology, University of Montreal, Sainte-Justine Hospital, instituted a clinical information system with a hard-wired decision support component.
When taking on this initiative, Dr. Gauthier had very specific goals in mind. First and foremost he wanted his department to be able to make better and timelier decisions in the diagnosis of dystocia — abnormally slow or difficult labor leading to potential fetal distress and/or maternal complications. In addition, he wanted to improve staff workflow and patient monitoring as well as simplify reporting and archiving tasks required to meet hospital quality standards.
Dystocia is loosely defined through conventional wisdom as the arrest of dilatation for a period of 2 to 4 hours or more, but wide variations in diagnostic standards can lead to both excessive intervention and, at the other extreme, delayed intervention with poor outcome. In the case of vaginal birth after cesarean (VBAC) this delay can lead to rare but devastating and costly outcomes such as uterine rupture, which has a high rate of associated birth-related brain damage.
Medical reports estimate that better care might reduce the incidence of birth-related brain injury by 33% to 50% (Ransom et al., 2003; Draper et al., 2002; JCAHO, 2004). The top contributors to these adverse outcomes include delay in recognition and response to abnormal fetal heart rate recordings and/or prolonged labor.›
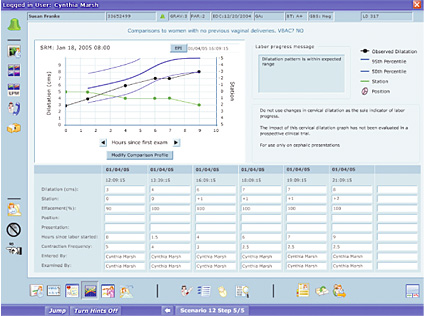
Dr. Gauthier was among the early adopters of a technology that provides decision support tools to assist clinicians with their clinical evaluations of labor and delivery. The system implemented at Sainte-Justine generates a labor curve with a continuous indication of the limits of normal labor over time for the patient’s specific parameters (i.e.: dilatation, cervical effacement, station, contraction frequency, epidural use; see Figure 1, pg. 42).
![]()
Figure 1: LMS CALM Curve Labor Progress Monitoring.
This system utilizes mathematical models to diagnose dystocia. Results from clinical studies with 11,000 patients in the United States and Canada have demonstrated that these models provide improvement›in optimizing›the use of cesarean sections (Hamilton et al., 2004). Other retrospective›studies of cases with uterine rupture›have shown that this catastrophic complication could have been›identified several hours in advance with›this computerized analysis of›labor progression (Hamilton et al., 2001).
According to Dr. Gauthier, “The Curve is a very effective way to follow patients; it provides a standardized approach in evaluating labor. With 40% of all cesareans performed due to failure to progress, this system really helps us to do better obstetrics. It provides me with information that was previously unavailable to support the diagnosis of dystocia. It offers objective and consistent data while always highlighting the normal limits of labor.”
The system is especially useful for women who are attempting a VBAC. “We did a retrospective study on our patients who had uterine rupture, and it was clear through the system that dystocia plays a major role and that without a complex model this is difficult to recognize. Now we are able to be more prudent and intervene earlier with a cesarean in order to prevent uterine rupture” (Hamilton et al., 2001).
As part of daily practice at Sainte-Justine, the system enables the team to work through the challenges of labor management with improved coordination between physicians and nurses and a better evaluation of labor progress. According to Dr. Marie-Anouk Blain, an OB resident: “When the pace picks up in the OB ward, and everything seems to be happening at once, the curve provides us with a common vocabulary and standard measurements that we can all relate to. Clarity in communications leads to sound action plans.”
To meet his other goals of improving efficiency and workflow in the labor and delivery unit, Dr. Gauthier’s implementation of the clinical information side of the system provided “a standardized way of entering information, of obtaining statistics, and improving how we do our jobs on a daily basis. The clinicians use the reporting module of the system for gathering, structuring, and aggregating patient data.” The system has also been helpful for meeting quality standards. “We use it to perform our semi-annual audit. The system documents various statistics such as number of deliveries, gestational age, forceps use, and cesarean rate — all of which help us look back and evaluate our practice,” said Dr. Gauthier.
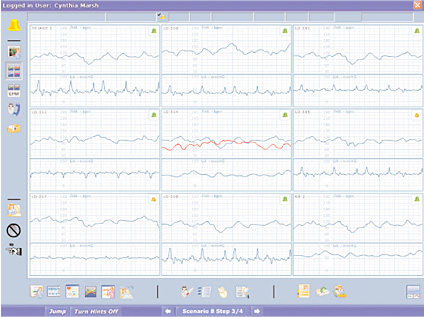
Further, the OB team relies heavily on the system for patient surveillance. “Because we can’t always be with the patient, it facilitates the way we do surveillance. Through centralized monitoring, we’ve got all the patient tracings on the screen (Figure 2). We can see right away if there is a problem with a patient and get to her immediately,” said Dr. Gauthier.
![]()
Figure 2: LMS CALM Surveillance Central Fetal Heart Rate Monitoring.
Overall, the use of a clinical information system and decision support tool has provided the Sainte-Justine team with a strong position to continue providing high quality patient care in their obstetrical unit — by supporting smart workflow and optimal outcomes.
|
Pamela Haswell (pamela@lmsmedical.com) is director of quality assurance and regulatory affairs at LMS Medical Systems in Montreal, Quebec. Her experience includes clinical trial design, training, and monitoring; preparation of regulatory submissions; development and auditing of quality systems; and management of software validation programs. She holds a master’s degree in pathology and is certified as a U.S. Regulatory Affairs specialist, a quality auditor, and a quality engineer. LMS Medical Systems is a provider of clinical information systems and dynamic decision support tools for obstetrics. LMS’s flagship product CALM has been adopted by Sainte Justine Hospital in Montreal, Canada, and by several other hospitals across North America.
References
Draper, E.S., et al. (2002). A confidential enquiry into cases of neonatal encephalopathy. Arch Dis Child Fetal Neonatal Ed 87,F176-F180.
Hamilton, E., et al. (2004). The effect of computer-assisted evaluation of labor on cesarean rates. J Healthc Qual 26(1), 37-44.
Hamilton, E.F., et al. (2001). Dystocia among women with symptomatic uterine rupture. Am J Obstet Gynecol 184(4), 620-624.
JCAHO Sentinel Event Alert,30. (July 2004).
Ransom, S.B., et al. (2003). Reduced medicolegal risk by compliance with Obstetric Clinical pathways: A case-control study. Obstet Gynecol101, 751 — 755.
