Creating and Sustaining a Culture of Safety
September / October 2008
![]()
Teams & Communication
Creating and Sustaining a Culture of Safety
Healthcare consumers are increasingly aware of medical error and publicly reported quality measures. Additionally, the Centers for Medicare and Medicaid Services’ (CMS) pending refusal to pay for certain “never events,” the advent of the Hospital Consumer Assessment of Healthcare Providers Survey (HCAHPS), and the work of the Institute for Healthcare Improvement (IHI), the National Patient Safety Foundation (NPSF), and Joint Commission have combined to produce conditions where creating and sustaining a culture of safety is a priority for many healthcare organizations. That was the case for The Nebraska Medical Center (TNMC) in Omaha. The academic medical center realized in 2004 that their patient safety efforts needed a boost to move from very good to great. A focus on quality and safety was one of four CEO leadership priorities, and the focus on quality and safety was incorporated into the hospital’s strategic plan with full approval of the Board.
Chief Medical Officer Steve Smith, MD, spearheaded the effort to change TNMC’s culture: “We want a safer place to practice medicine with the confidence that all steps necessary to ensure our patients’ safety to the highest degree are taken into account for all cases.” Based on a recommendation from the chief of surgery, Smith elected to join forces with LifeWings, a consultancy group that works with clients to create a culture of safety by adapting the best practices of aviation and other high reliability organizations.
TNMC chose to follow a five-point plan for creating and sustaining an improved culture of safety. In a 6-month period of 2005 and 2006, the first four steps of the plan were conducted in perioperative services as proof of concept with follow-on implementation planned for other areas after success in the OR.
Step 1. Develop change-initiative skills for key leadership positions and an organizational structure that will support the new culture. Realizing no change would occur without partnership with the institution’s physicians, TNMC recruited physician champions, briefed all physicians in perioperative services through monthly meetings and surgery Grand Rounds, and made sure each physician understood the methodology, potential results, and “what’s in it for you” for supporting the initiative. This was an important step, as TNMC already had very high levels of patient safety in other areas. Next, key leaders at both the institutional and departmental level were trained on leading change initiatives. Skills learned included:
- responding to difficult questions about the initiative,

- recruiting champions and coaching low performers, and

- conducting rounding for patient safety.
Organizational development to support the initiative included:
- a project oversight and steering committee,

- revisions to policy and procedure manuals,

- alignment of leadership assessment systems to support the culture,

- a data collection and analysis plan for project measurement, and

- making the training and new safety tools mandatory for all physicians and staff — including consequences for non-compliance.
Step 1 was perhaps the most important part of the methodology as research shows that “end user” adoption of culture changing behaviors and tools is primarily a function of effective leadership action.
Step 2. Provide training in teamwork and communication to support desired culture-changing behaviors. Following a site visit, a thorough patient care processes review, and preparation of a teamwork scorecard as part of their needs analysis, LifeWings prepared customized courseware targeting the needs of TNMC and presented it to physicians and staff. The training was interdisciplinary, experiential, and based on healthcare case studies. It provided evidence-based teamwork skill sets based on team training from the aviation industry — called Crew Resource Management (CRM) — and adapted for the needs of the OR team. CRM is based on the best science and research on high performing teams.
Step 3. Create and implement site-specific safety tools to hardwire the teamwork behaviors into daily work life. Using a process based on Lean, a small work group of physicians and staff met to 1) identify points in their workflow where improvements in patient safety were most needed and 2) create safety tools such as checklists, structured handoffs, protocols, and communication scripts to facilitate the needed improvements. An education and implementation plan was created for each tool. Tools were implemented over a period of weeks. The first tool completed and implemented was a Pre-Procedure Briefing (Figure X) for surgical cases that incorporated the elements of the Universal Protocol (which is available online at www.psqh.com/xxx. It also included checklist items to ensure all staff and needed equipment were available and operational, and that the patient was completely ready for the procedure to begin.
Step 4. Collect and analyze data to document results. TNMC created a measurement plan to analyze results by examining safety measures including safety climate surveys, teamwork and communication issues, and process reliability and efficiency.
Step 5. Conduct training for “master trainers.” TNMC wanted to bring the culture-changing initiative in-house as quickly as possible and avoid an extended engagement with an outside consultant. To develop their internal capacity, three trainers were chosen in 2006 to learn to provide the teamwork skills training and to create and implement the safety tools. Two trainers were from the Six Sigma department and one was hired externally. Once qualified by LifeWings, these trainers assumed responsibility in 2007 and 2008 for the roll out of Steps 1 through 4 in the emergency department, the cardiac catheterization and electrophysiology labs, and the obstetrics and gynecological services department. TNMC continues to roll out the system in its critical care areas with plans to implement the culture change in its entire hospital.
Results
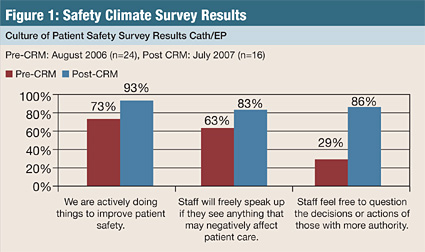
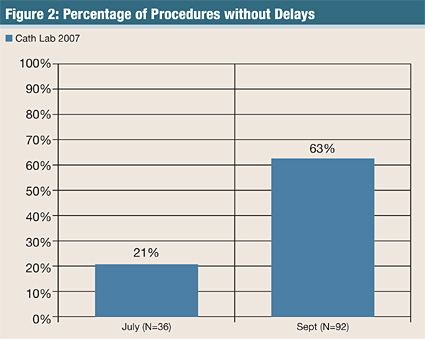
The culture of safety has improved at TNMC. Results of the safety-climate survey administered after the implementation in the areas listed above show dramatic improvement in the perception of staff, physicians, and residents on those indicators related to patient safety in their area (Figure 1). Additionally, the culture has produced multiple examples of “good catches” by the staff as they have intercepted potential errors that might have affected patient safety. In addition to improved patient safety, TNMC has seen an improvement in cases without significant events, reducing unexpected delays (Figure 2). As a result of their culture-changing efforts, TNMC recently won the “Quest for Excellence” award given each year by the Nebraska Hospital Association. The award represents “the highest level of professional acknowledgement in Nebraska’s hospital quality improvement arena.” TNMC has proved that though disciplined leadership action, effective interdisciplinary skills training, use of site-specific safety tools that hardwire behaviors, and program-guiding measurement, the safety culture can be changed and improved.
Stephen Harden is the co-founder and president of LifeWings Partners LLC. He is co-author of CRM: The Flight Plan for Lasting Change in Patient Safety (published by HC Pro) and is a nationally known speaker on creating a culture of patient safety. He can reached at sharden@SaferPatients.com.
