Continuous Pulse Oximetry Monitoring in the Inpatient Population
May / June 2009
Continuous Pulse Oximetry Monitoring in the Inpatient Population

![]()
Photo Courtesy of Nancy Karon
John Smith is admitted late Monday afternoon to the post-surgical ward after a total knee replacement. John is overweight, though not morbidly obese, and has an undeclared history of snoring. He wakes up at 5:30 Tuesday morning with considerable pain; over the next hour he exhausts the opiate supply in his PCA pump, and his nurse inserts a new syringe before her shift ends at 7 a.m. It will be more than 45 minutes before John is next checked by the nurse starting his day shift — plenty of time for John’s high dosage of opiate analgesics, exacerbated by his undiagnosed sleep apnea, to send him dangerously deep into respiratory depression.
Similar scenarios play out daily at hospitals across the country, leading to increased length of stay, costly ICU admissions, and even preventable patient deaths. Patients under moderate sedation can deteriorate rapidly due to respiratory depression, airway obstruction, etc. In many procedural settings, such as colonoscopy, this risk is managed with individual attention from a highly-trained nurse and continuous physiological monitoring. However, floor nurses in a surgical ward routinely manage multiple patients at an equivalent level of sedation for days at a time, with vitals checks occurring only every several hours.
Automated electronic physiological monitoring presents a possible solution to this safety gap, but high cost and high false alarm rates have prevented its widespread acceptance to date. One institution’s experience with a new pulse oximetry-based system, combined with careful implementation and optimization strategies, suggests that it is possible to mitigate these shortcomings and bring about a sustainable increase in patient safety.
For patients like John Smith, this extra protection is critical. His continuous pulse oximetry monitor identifies his deep desaturation and alerts the nurse coming on duty. The respiratory depression is reversed without intubation, and John is able to avoid an increased length of stay on the inpatient ward.
The Setting
At Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, New Hampshire, the new monitoring system has been implemented on a 36-bed inpatient ward primarily handling orthopedic surgery, as well as trauma and plastic surgery. Nominal nurse-patient ratio is 1:5, with beds laid out in a pod structure that increases patient privacy but makes direct observation by clinical staff more difficult. The focus on orthopedics, and particularly joint replacement, means that many patients are on high levels of opiate analgesics for extended periods — making the ward an ideal setting for an early-detection safety initiative.
The System
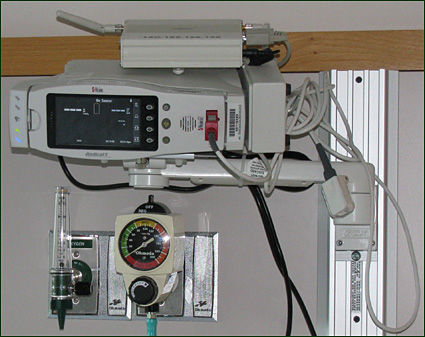
DHMC uses a pulse oximetry-based floor monitoring system with direct nurse notification via pager specifically designed for the general floor environment. Standard bedside pulse oximeters communicate over the hospital’s wireless infrastructure, connecting to a computer server and admitting station (Figure 1). Nurses receive direct notification via pager when an alarm condition is violated. The default definitions of these alarm conditions are configurable by biomedical engineering.
![]()
Clinicians use the nursing station to admit, discharge, and modify alarms for their patients. When a patient violates an alarm condition, a page is first sent to that patient’s nurse; if the condition is not corrected within 2 minutes, a secondary page is sent to the second nurse on the pod, as well as the resource nurse on duty.
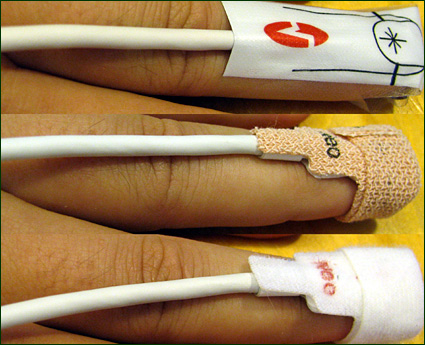
The PSN system works with any oximetry probe fitting the bedside oximeter unit (Figure 2). It is important to avoid spring-loaded clip-style probes for surveillance monitoring, as they carry a risk of pressure necrosis, generate more false alarms, and introduce a source for infection. The trial unit began with adult disposable probes, before switching to micropore tape probes, which were found to offer better adhesion over time. Velcro probes are also in use, which are more compatible with the frequent washing required by a hand hygiene initiative on the unit.
![]()
The Process
Managing early detection and response takes cooperation from multiple disparate entities, both inside and outside the hospital. At DHMC, the major stakeholders are:
- Industry: designs and builds technology.

- Biomedical engineering: installs and configures technology.

- Clinical leadership: designs and implements monitoring policy, procedure and practice.

- Nursing staff: carries out monitoring; interacts with technology.

- Rapid response team: often called to respond to deterioration events.

- Doctors: write monitoring orders, determine treatment plans.
In order to make sure that a monitoring solution took all of these viewpoints into account, planning meetings for the new monitoring system included representatives from all of the above groups. This enabled a holistic design process, which was able to uncover and address issues from all elements of the early detection system, from installation to event detection to event response.
Human factors engineers also participated in the design process, first by studying the practices already in place on the target unit, then through input to the design and implementation process, and finally by observing the new system as it was put in place. These observations inform implementation planning for new installations of similar systems.
A key observation from prior floor monitoring experiments at DHMC was the problem of oversensitivity: when a monitoring system generates a high number of false positives, nursing staff begins to ignore the alarms, and the system loses almost all utility. In order to prevent this process, a target was chosen of one false alarm per patient per shift.
Reducing false alarms requires optimization of each component within the end-to-end system. The sensor selection and application must take into account the unique setting of general patient care. Single use disposables are preferred in order to minimize false alarms due to patient movement and meet infection control objectives. The bedside device must mitigate false alarms with measure-through-motion algorithms as well as provide an easy to use interface for the nursing staff. Connectivity to the bedside device must be both highly reliable and affordable so the system is scalable throughout the hospital. Alarm notification to the assigned nurse must filter non-treatable events from those that require urgent intervention. The entire system must be a trusted tool that enhances the normal work flow within the general care environment.
Alarm conditions for this trial were chosen with this goal of false alarm mitigation in mind. False readings in pulse oximetry often come as brief spikes due to patient motion or other factors. For example, a patient repositioning him- or herself in bed may grab a trapeze that momentarily obstructs blood flow to the finger on which the sensor is placed, causing a brief, localized but non-treatable drop in oxygen saturation. Averaging can help to mitigate these spikes, but excessive averaging reduces the responsiveness of the monitor signal to real physiological changes. In addition to configurable averaging, the system has the ability to delay audio annunciation of alarms both at bedside and prior to issuing an alarm page. Delays at the bedside reduce noise within the patient room from non-actionable alarms and thereby improve the patient care environment. Additional delays within the system allow a nurse in proximity to the patient to respond before an alarm page is initiated. Using a 30-second delay (15 seconds at bedside and an additional 15 seconds before paging) was found to drastically reduce the number of non actionable alarms transmitted to nurses. With the only pre-existing physiological monitoring being 4- or 8-hour vitals checks, even this relatively low-sensitivity alert setting represents a major improvement.
Similarly, while procedure-level patient monitoring often uses very tight physiological thresholds in order to identify minor deviations from baseline, surveillance monitoring can use looser limits which, when violated, raise the probability of a legitimate deterioration significantly. For this trial, the oxygen saturation lower alarm limit started at 75%. After a week of testing, this was raised to 80%, which has yielded a good balance of sensitivity and specificity for the surveillance monitoring environment. Heart rate limits were set at 50 and 140 beats per minute. While extreme, these alarm thresholds are appropriate for interrupting a busy nurse.
Posters and presentations during the design phase helped communicate to the nursing staff that their feedback would be used to tune the technology during installation and would ultimately determine whether it would stay in place long term. This was reinforced with a month-long period of daily rounding by clinical and technical staff. Directly soliciting feedback from clinicians, rather than waiting for them to take the initiative, yielded valuable insights into the strengths and weaknesses of the technology.
Preliminary Results
The trial at DHMC has shown that floor-wide pulse oximetry-based surveillance monitoring can feasibly be implemented using current technology. Critically, there have been only about four alarms per patient per day, which approaches the goal of one per patient per shift. Nursing satisfaction has been very high: front-line staff were overwhelmingly in favor of keeping the system after the initial trial period.
Rapid-response activations have dropped significantly, which the team attributes to improved ongoing awareness of patient state. Fewer patients have been transferred to intensive care because clinicians are responding to early warning indicators identified by the system — nurses often use the term “drift” to describe a slow deterioration detectable over the course of a couple hours, even before alarms have been tripped. A wide array of physiologic deteriorations has been noted, including preliminary indications for several that are not commonly associated with pulse oximetry: poor heart rate control, acute bradychardia needing atropine, new onset atrial fibrillation, and pulmonary complications such as fat emboli syndrome, pulmonary embolus, and pulmonary edema. It is hypothesized that longer-term data will demonstrate improvements in length-of-stay and patient throughput resulting from the early detection and treatment of these conditions. Anecdotal evidence already exists for improved length-of-stay in individual cases, such as the use of the low saturation alarm as a reinforcement tool for incentive spirometry use.
One unanticipated effect is new diagnoses identified by the system. Many obstructive respiration patterns, likely undiagnosed sleep apnea, have caused repeated alarms at night and led to increased collaboration with the on-site sleep lab. In the extreme case, discovery of previously-undiagnosed respiratory irregularities can delay placement of post-operative patients into recovery care. Nurses also identified some usability difficulties with the system, particularly associated with the specific pagers used in this trial. This feedback is being used by the company to improve human factors within the system.
Conclusions
Overall, the trial has been a solid success, and DHMC plans to install the system at other sites in the institution. The lessons of the trial, particularly in the importance of understanding the existing practices, limitations and priorities of new sites, serve as a useful guide for future implementations.
Josh Pyke is a PhD candidate at Dartmouth’s Thayer School of Engineering. Pyke holds a BA in engineering from Dartmouth and a BE in computer and electrical engineering. He has worked as a researcher in Susan McGrath’s lab at the Thayer School, where he was involved in software development, human factors research, and systems design for several projects, including a tele-ultrasound system for real-time ultrasound exams at a distance. Josh is currently pursuing a doctorate in computer and electrical engineering, with a planned thesis project that will leverage database design, data mining and human factors engineering to extend the capabilities of inpatient monitoring systems across multiple hospital units. Pyke may be contacted at Joshua.B.Pyke@dartmouth.edu.
Klaus Christoffersen is adjunct assistant professor in the department of anesthesiology at Dartmouth Medical School in Hanover, New Hampsire. Klaus’ background is in cognitive systems engineering, which focuses on designing tools and work processes to support human performance in knowledge-intensive domains such as healthcare. In addition to his work in healthcare, he is co-founder and owner of AcuitÔ Technologies Ltd., a company specializing in human factors engineering and user interface design for industrial applications. Klaus received his PhD in industrial and systems engineering from The Ohio State University. He is a member of the Human Factors and Ergonomics Society and sits on the Interface Standards Development committee of the Instrumentation, Systems and Automation Society.
Jean Avery is a registered nurse working in the department of quality and patient safety at Dartmouth-Hitchcock Medical Center. Jean has 30 years of nursing experience, the last 18 of which have been focused on quality and patient safety. Her primary focus has been on medication safety and system improvement. Jean received her undergraduate degree from the University of Vermont and her MBA from Plymouth State College in Plymouth, New Hampshire.
George Blike is the quality and patient safety officer, medical director of the Patient Safety Training Center, and a staff anesthesiologist at Dartmouth-Hitchcock Medical Center, and a professor of anesthesiology at Dartmouth Medical School. His career is devoted to creating high performance in complex systems as they relate to patient safety. He recently co-created an 8,000 square-foot, multidisciplinary simulation training center that provides patient safety training to all clinicians and employees in a safe environment. Blike received a BS in biochemistry from Case Western Reserve, his MD from the University of Cincinnati, completed his internship in medicine at Hartford Hospital, and his anesthesiology residency at Yale New Haven Hospital. Blike is a member of the American Society of Anesthesiologists, Human Factors & Ergonomics Society, International Anesthesia Research Society, Society for Pediatric Sedation, Institute for Healthcare Improvement, and Society for Technology in Anesthesia.
Susan McGrath is a research associate professor of engineering and senior lecturer at Dartmouth’s Thayer School of Engineering. McGrath holds a BS in electrical engineering from Drexel University and an MS and PhD in biomedical engineering from Rutgers University. Her graduate research focused on biomedical instrumentation and biomedical image processing and classification. Prior to joining Dartmouth College, McGrath worked at the Naval Air Warfare Center in Lakehurst, New Jersey, and at Lockheed Martin’s Advanced Technology Laboratories (ATL) in Camden, New Jersey. At Dartmouth, McGrath was associated with the Institute for Security Technology Studies (ISTS) and was Director of Emergency Readiness and Response Research Center at ISTS from 2004-2006. Her current research interests include mobile computing and intelligent software applications for biomedical, emergency management and command and control applications.
Nancy Karon is a graduate of Massachusetts General Hospital School of Nursing and of Vermont College/Norwich University, where she graduated Summa Cum Laude with a BSN degree. She has 36 years of nursing experience in acute care nursing. Karon has 33 years of experience as a nurse leader in an academic medical center in the Northeast. Her areas of interest and expertise are medication safety, patient safety, medical/surgical nursing, trauma, and orthopaedics.
