Clinical Vigilance: ICU Bouncebacks Present Opportunity for Improvement
January / February 2008
Clinical Vigilance
ICU Bouncebacks Present Opportunity for Improvement
With the advent of the 80-hour workweek for residents at academic health centers, there has been a predictable increase in the number of patient handoffs during a hospital stay. Shorter duty intervals require more frequent transfers of care — “handoffs” — which inevitably result in an undesirable fragmentation of care. Moreover, this discontinuity of care may lead to additional negative results with regard to incomplete communication of pertinent clinical information, lack of appreciation of subtle changes in a patient’s condition, and decreased patient satisfaction from an inability to bond with a physician.
These cumulative, suboptimal effects are most concerning because they impact patient safety and quality of care. The medical literature is replete with demonstrations of adverse effects that emanate from increased patient handoffs, since they interrupt the seamless and timely transition of care, whether they occur between units of a hospital or from one set of caregivers to the next (Arora, et al., 2005; Sutcliffe, et al., 2004; Petersen, et al., 1998). When patients are subjected to additional clinical handoffs, their safety is threatened. The fragmentation of care that results from interrupted workflow produces a tension, which may undermine the process of the patient’s recovery.
Denver Health is an academic, level-one trauma center that is the main safety-net provider for the city of Denver. It has two large intensive care units (ICU) staffed by a distinct set of physicians, different from those who manage patients on the medical wards. Recent studies suggest that the ideal ICU model may be a closed unit staffed by dedicated intensivist physicians (Chang, et al., 2005). Denver Health has adopted that model. However, in 2005 a concern was raised that at times patients were being transferred out of the ICUs only to “bounceback” to the ICU within 48 hours of transfer. In general, it seemed that some patients were not fully ready for a lower intensity of care. Their instability became manifest shortly after transfer, necessitating a transfer back to the ICU. The safety problems associated with increased patient handoffs also apply to unexpected readmissions to the ICU.
To address this problem, we convened a multidisciplinary group of physicians and nursing personnel to devise a system to reduce ICU bouncebacks and thus reduce the number of patient handoffs. A series of meetings were held with our clinical leadership at their bimonthly Director of Service meetings to review bounceback cases. As we learned more about this preventable adverse event, there was impetus to define a policy and procedure that increased vigilance for ICU patients who were being considered for transfer to the regular medical-surgery wards. Specifically, we mandated that any patient deemed appropriate for transfer from an ICU requires an attending note stating that the patient is safe to transfer based on a thorough concurrent review of his or her clinical course while in the ICU.
In addition, at about the same time, we initiated our “clinical trigger/rapid response” program, which is based on early detection of evolving clinical parameter instability and a process to escalate care of these patients with alacrity (Mehler, et al., 2007). This program is a variation of the rapid-response team concept (Bellomo, et al, 2004), which has gained popularity, but was not felt to be in the best interest of the patients at Denver Health. Our program involved a massive initiative to educate nursing, residents, and attending personnel about the need for increased clinical vigilance for patients who may be starting to deteriorate. Patients often exhibit measurable signs of clinical deterioration for many hours preceding an in-hospital cardiac attest (Buist, et al, 1999). Our program capitalizes on this available time to strategically intervene proactively and early in the course of events.
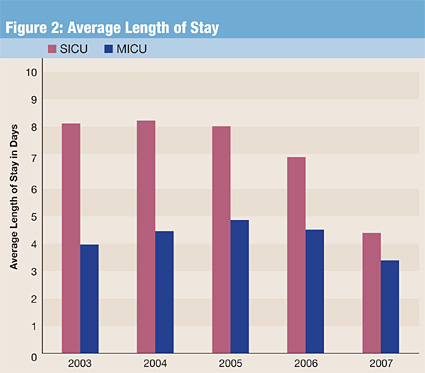
Preliminary results of our program to reduce ICU bouncebacks are most encouraging. As shown in Figure 1, our number of ICU bouncebacks per month has reduced substantially from 8.7 to 4.4 after implementing our program (t=5.0, p<0.001). of note, this is not simply due to a patient flow issue and patients remaining in the icu for longer periods of time; our average length of stay in the icus at denver health has been trending downward for the last 3 years (figure 2). both of these initiatives — rapid response and icu bounceback reduction — have at their core the thematic concept of increased and compulsive oversight of clinical care.
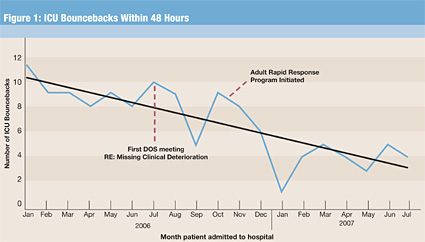
In summary, although it may be too early to draw definitive conclusions, unexpected ICU bouncebacks within 48 hours of transfer out of the ICU seem to be indicative of suboptimal clinical vigilance. However, the additional patient handoffs that result are irrefutably associated with significant potential for adverse effects on patient care. The reduction in the rate of ICU bouncebacks that we have observed may offer a surrogate marker for a clinical quality dashboard and affirms for us the opportunity to strive for additional ways to achieve excellence in the patient care experience.
Kendra Moldenhauer graduated from the School of Nursing at the University of Northern Colorado in 1983 and joined Denver Health as a staff nurse in 1984. She was the nurse manager for the outpatient surgical specialty clinics and adult critical care and the trauma program manager for the Level I trauma center at Denver Health Medical Center. Moldenhauer is currently the manager of patient safety and quality.
Philip Mehler was born in Denver, Colorado, and went to medical school at the University of Colorado. After completing a residency and chief residency in internal medicine, he joined Denver Health, Colorado’s public safety net hospital, in 1987. From 1993 to 2003, he was the chief of internal medicine, and in 2003 he was promoted to associate medical director and director of patient safety and quality. His research interests include hypertension control, cardiac risk modification, and the medical complications of anorexia and bulimia. He has authored more than 200 pieces of scholarly work and is a professor of medicine at the University of Colorado where he holds an endowed chair. From a patient safety and quality standpoint, his main focus is in the areas of hypertension and diabetes control, reducing failure to rescue occurrences and nosocomial infections, and on-time occurrence reporting. Mehler may be contacted at pmehler@dhha.org.
Allison Sabel is the director of medical biostatistics at Denver Health. She is a board-certified preventive medicine physician. She completed an MPH in epidemiology before entering a MD/PhD program at Tulane University with her PhD in biostatistics. Sabel was chief resident of both her transitional residency and preventive residency programs. She has taught biostatistics for 10 years at the graduate school level at Tulane University and University of Colorado. Sabel is currently an assistant professor in the Department of Preventive Medicine and Biometry at the University of Colorado Health Sciences Center.
References
Arora, V., Johnson, J., Lovinger, D., Humphrey, H.J., & Meltzer, D.O. (2005). Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Quality and Safety in Health Care 14, 401 – 407.
Bellomo, R., Goldsmith, D., Uchino, S., Buckmaster, J., Hart, G., Opdam, H., Silvester, W., Doolan, L., & Gutteridge, G. (2004). Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Critical Care Medicine 32, 916-921.
Buist, M.D., Jarmolowski, E., Burton, P.R., Bernard, S.A., Waxman, B.P., & Anderson, J. (1999). Recognizing clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a tertiary-care hospital. The Medical Journal of Australia 171, 22-25.
Chang, S.Y., Multz, A.S., & Hall, J.B. (2005). Critical care organization. Critical Care Clinics 21, 43-53.
Mehler, P.S., Moldenhauer, K., & Sabel, A. (2007). Clinical Triggers and Rapid Response Escalation Criteria. Patient Safety and Quality Healthcare, 4(2), 12-13.
Petersen, L.A., Orav, E.J., Teich, J.M., O’Neil, A.C., & Brennan, T.A. (1998). Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Joint Commission Journal on Quality Improvement 24, 77-87.
Sutcliffe, K.M., Lewton, E., & Rosenthal, M.M. (2004). Communication failures: an insidious contributor to medical mishaps. Academic Medicine 79, 186-194.
