Care Management: Patient Safety and Quality Healthcare Measure, Compare, and Improve
January / February 2007
Care Management

Measure, Compare, and Improve
How Memorial Hermann The Woodlands Hospital used decision support to improve quality, safety, and care management.
At an early morning department meeting in the fall of 2005, the physicians and nurses of the Critical Care Committee at Memorial Hermann The Woodlands Hospital in Texas gathered over coffee and bagels to review the latest data from the hospital practice. The LCD projector hummed as Tami Wheeler, RN, BSN, MBA, director of clinical effectiveness, began. However, rather than showing the usual PowerPoint presentation, she logged on directly to Memorial Hermann’s decision support system, and began to show the department’s performance in key areas for the past quarter.
“In the past, we had a difficult time identifying problems,” Wheeler reports. “Staff would have a gut feeling or hunch about an issue, but it was hard to gather the right kind of data to confirm that a problem existed. And, when we did, we didn’t have reliable comparative data, so it was unclear which problems were worthy of work, and if you had several, which one should come first. With the new system, we can do it differently now.”
The Woodlands is one of 10 hospitals of the Memorial Hermann system in metropolitan Houston that has implemented a system to provide real-time data on current inpatients and recent discharges, as well as historical data measured against the vendor’s comparative database. During implementation, more than 100 people were trained at 10 sites, including William Parks, MD, chief medical officer at Memorial Hermann The Woodlands Hospital. Training consisted of two 2-hour remote sessions, which reviewed the functionality of the system so that users could immediately begin applying the system to their own data inquiries.
Clinical Data and Performance
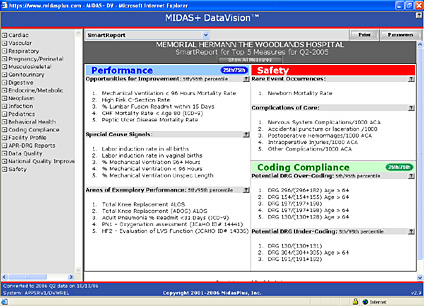
Parks and Wheeler meet weekly to go over current issues on quality or utilization, and to review performance data. With the new information system, they can quickly check their “hunches” against appropriate data with standardized definitions and compare themselves to peer hospitals by bed size, region, academic teaching status, or acuity. Built into the software is a comparative report that displays their last quarter’s data against a comparative database, showing measures that exceed desired thresholds (Figure 1, p.36). Once opportunities are identified, Parks and Wheeler can look back at prior performance over past months or years to see if the findings are new or part of an ongoing issue.
![]()
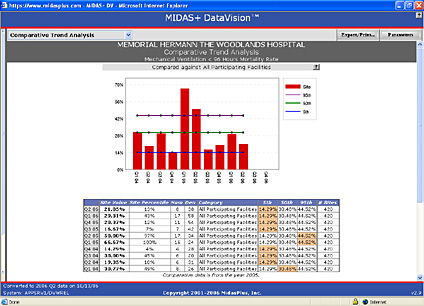
That morning in 2005, the Critical Care Committee discussed rumors that reported, “there are a lot of patients at the end of life in the ICU, many of them on ventilators.” Wheeler and Parks discovered a high mortality rate for patients on ventilation for less than 96 hours. The average mortality rate for this group of patients (acute care inpatients with a principal ICD-9 procedure code for continuous mechanical ventilation for < 96 hours) among 420 hospitals in the comparative database was 30%, whereas Memorial Hermann The Woodlands was running at 66.67%, well above the 95th percentile. These numbers were high.
Parks and Wheeler used the application to drill down to patient-level detail for the population at risk, including those who died. Patient-specific data, including principal and secondary diagnoses, and all procedures, were analyzed. Further analysis showed combinations of diagnoses consistent with the end of life. The committee reviewed the data and decided to investigate further by conducting a chart review of these patients on ventilators for less than 96 hours.
The committee discovered that many of the patients in the data set had reached the end of life and presented to the emergency room in respiratory failure, then were intubated and admitted to the ICU. At this point, caregivers and family realized that comfort care was more appropriate and consistent with the patient’s course and their wishes. These patients were taken off of ventilation and transferred out of the ICU. If these ICU admissions could have been avoided, patients would have been saved the discomfort of intubation and ventilation, and precious resources could have been saved for the next trauma patient.
Once this issue was identified, the team began planning a palliative care program for end-of-life patients to intervene earlier in the hope of preventing inappropriate or undesirable intensive care.
Four quarters later, the mortality rate at Memorial Hermann The Woodlands Hospital for mechanical ventilation less than 96 hours is 21%, just above the 10th percentile, a remarkable improvement (Figure 2).
![]()
Beyond Critical Care
In addition to critical care, the system is used routinely in medical staff meetings to show physicians’ current, standardized, severity-adjusted data, and comparative data. Other departments that use this data in real time include pediatrics, internal medicine, family practice, critical care, and emergency medicine. The tools are also used by the interdisciplinary Clinical Effectiveness and Resource Management Committee, the Patient Care Committee, and the Medical Executive Committee.
The system is very helpful for nursing issues as well. The department of nursing monitors a battery of related measures on hospital-acquired deep venous thrombosis (DVT) and plots it against its own compliance with DVT prevention measures. The system provides measures based on complication codes (ICD-9 800 and 900 codes) as well as all the AHRQ Patient Safety Indicators (PSIs). The DVT measures that are monitored as outcomes include:
- Hospital-acquired DVT frequency/1000 acute care admissions. This is a count of acute care inpatients with a secondary ICD-9 diagnosis of deep venous thrombosis, minus all inpatients with a principal ICD-9 diagnosis code for pulmonary embolus. It creates a good estimate of acquired DVTs.

- Peripheral vascular complications/1000 acute care admissions. This is a count of all inpatients with an ICD-9 diagnosis of 997.2, peripheral vascular complications, phlebitis or thrombophlebitis during or resulting from a procedure.

- Iatrogenic pulmonary embolus/1000 acute care admissions. A discharge diagnosis code of ICD-9 415.11, iatrogenic pulmonary embolism and infarction.

- Postoperative pulmonary embolism (PE) or DVT/1000 surgical discharges with an operating room procedure. Count of discharges with DVT or PE in any secondary diagnosis field out of the population of all surgical discharges (DRG or ICD-9 code for an operating room procedure).
These are plotted against nursing process data on compliance with DVT prevention, which is recorded with the help of an internally built Web-based tool.
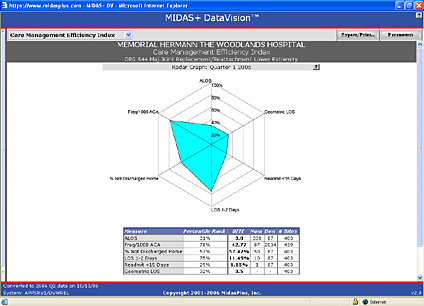
Now the director of care management, Wheeler checks her IT systems every day or two for ongoing monitoring of utilization review. She is always asking, “Do we have the right programs in place? How are we now compared to a year ago? Where do we need to go next?” She can check key data in graphic format by DRG or ICD-9 code, with special attention to average length of stay, geometric mean length of stay, and patients not discharged home (Figure 3). In addition, the system supports data entry for all JCAHO and CMS Core Measure elements and reports the results against the rest of the Memorial Hermann system, as well as against the national comparative database. It is also easy to check current performance in their system, well before the data is harvested and sent to JCAHO and CMS.
![]()
Chart Documentation
Correct and complete chart documentation is essential to support patient care decisions, and in turn ensure the hospital achieves payments commensurate with the resources required for care. Tami Wheeler, together with the director of health information management, regularly looks at the Coding Compliance section, where these key metrics are displayed (Figure 1).
One of these metrics measures the accuracy of coding for patients with urinary tract infections (UTIs), and urinary tract infections with sepsis. If all the patients with DRG 416 (Septicemia age >17 Relative Weight of 1.6774) are counted, and divided by the sum of DRG 416 plus DRG 320 (Kidney and Urinary Tract Infection age >17 with CC, Relative Weight 0.8658), a ratio is obtained that varies nationally anywhere from 30% to 80%. Low ratios imply fewer patients with sepsis, and more with simple UTI; high ratios imply more patients with sepsis, and fewer with UTI. Lower ratios are associated with lower reimbursement, due to the difference in relative weights for the two DRGs. Although patient populations clearly vary by site and time frame, in general, variations in this ratio reflect the difference between a physician note stating “UTI” or “Urosepsis” (DRG 320 RW 0.8658) versus “UTI with Sepsis” (DRG 420 RW 1.6774). In 2005, for all MedPar patients* the average ratio was 56%, and for the vendor’s comparative database, 57%.
*MedPar: The Medicare Provider Analysis and Review (MEDPAR) file contains records for 100% of Medicare beneficiaries who use hospital inpatient services.
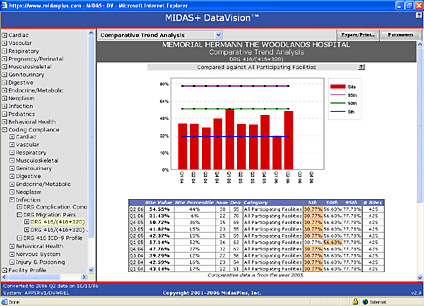
In the summer of 2006, the Care Management Steering Committee noticed that the ratio at Memorial Hermann The Woodlands Hospital for Quarter 1 2006 was very low at 31% (Figure 4), implying insufficient chart detail for patients with UTI. Wheeler was able to rapidly identify the patient population behind the ratio and select a random sample of charts for review. She found that many doctors were seeing seriously ill patients with sepsis (SIRS** with infection) of urinary tract origin, which should be DRG 416, but labeling them as “Urosepsis” which by coding guidelines translates to the lower relative weight DRG 320, UTI. Discussion began with physicians about more accurate documentation to better reflect the care being given to the patients, with early data suggesting a reversal of the coding ratio trend. This creates more accurate medical records and public health data, as well as ensuring the hospital is being paid appropriately for care delivered.
![]()
As well, the system can help discover errors in data entry. For example, Wheeler identified inaccuracies in discharge status that made it appear that mothers admitted for vaginal delivery were not going home on discharge, a highly unusual finding. However, chart review showed that these mothers were going home with their infants. Examination of the data entry processes showed that there were some recent changes. For years, the billing office coded discharge disposition with a few dedicated staff accurately entering data using actual dictionary codes, “02” for “home.” However, the process changed, with discharge disposition being entered by clerks on the nursing units. Multitasking, the clerks depended on the drop down menus in the hospital information system, where the second choice was “home,” which unfortunately in the dictionary did not match to the correct code, “02.” Unbeknownst to the clerks, the patients were coded in the system as not going home. Once discovered, the mismatch in the dictionary was corrected, and mothers are now correctly listed as discharged home. A process error has been discovered and corrected, creating more accurate data.
“Having access to a variety of valid, standardized information, with comparative data and the ability to drill down to the patient level, has enabled us to be more focused in our approach to quality, safety, and care management,” Wheeler says. “Relevant information is now accessible if you are willing to look for it. Healthcare professionals should embrace this information to recognize trends and then identify and change processes requiring improvement.”
The Woodlands is one of 10 Memorial Hermann hospitals that have implemented the system. Winda Antoine, manager of information systems, notes, “For our whole system, this is an amazingly robust tool that allows us to not only compare each of our hospital’s performance to the others in our system, but allows benchmarking to other hospitals of like sizes and case mix indexes in the United States. We can find out how we are performing against over 425 other sites nationwide.”
Henry Johnson is medical director of the MIDAS+ software division of ACS Healthcare Solutions, in Tucson, Arizona. Previously, he served the five-hospital Scripps Health system in San Diego as vice president of clinical measurement and outcomes. Johnson has also been an Institute of Medical Quality (IMQ) surveyor for the Consolidated Accreditation and Licensure Survey program in California. He served on the Patient Safety Taxonomy Steering Committee of the National Quality Forum (NQF) and is currently co-chair of the NQF Patient Safety Taxonomy Consensus Standards Maintenance Committee. Johnson may be contacted at henry.johnson@acs-inc.com.
Tami Wheeler is currently director of case management at Memorial Hermann The Woodlands, a 214-bed hospital in metropolitan Houston. Wheeler received her nursing degree from Capital University in Columbus, Ohio, and an MBA from Nova University, Ft. Lauderdale, Florida. She has worked in critical care, neonatal ICU, and post-surgical care in hospitals from 40 to 800 beds, and has 18 years of experience in quality and case management. She may be contacted at tami.wheeler@memorialhermann.org.
William Parks is the chief medical officer at Memorial Hermann The Woodlands Hospital. Parks received a bachelor of arts degree in microbiology and his MD from the University of South Florida, with postgraduate training in pediatrics at the University of Texas Medical School at Houston. He has received the Certificate in Medical and Healthcare Management from Rice University. Prior to 2005, Parks was in private practice as a pediatrician, and also has been actively involved with The Community Clinic, a not-for-profit indigent care facility. Parks may be contacted at william.parks@memorialhermann.org.
Winda Antoine is manager of information systems at Memorial Hermann Healthcare System, a corporate site supporting approximately 17,000 employees using information technology at 15 hospital campuses. Antoine received her bachelor’s degree in medical record administration from the University of Texas Medical Branch in Galveston, Texas, and a master’s degree in management, computing, and systems from Houston Baptist University in Houston, Texas. She has worked in medical records, risk management, quality management, and information technology at pediatric and general medical/surgical for-profit and not-for-profit teaching and non-teaching hospitals for more than 20 years. Antoine may be contacted at winda.antoine@memorialhermann.org.
