Cardiac Telemetry Guidelines Improve Bed Utilization and Resources
September / October 2008
![]()
Cardiac Telemetry Guidelines Improve Bed Utilization and Resources
Jackson Memorial Hospital is a 1,600-bed tertiary care facility in Miami, Florida, and serves as the primary teaching hospital for the University of Miami — Miller School of Medicine. At one time, the majority of the medical services were teaching services run by house staff physicians; today approximately half of the general medical inpatient services are run by the non-teaching hospitalist services.
Much like other institutions, Jackson Memorial Hospital was experiencing an increased need for adult cardiac telemetry beds, to the point where an excessive number admitted patients were waiting in the emergency services department for telemetry beds daily. While some suspected that many of the patients did not truly require telemetry, we needed to perform a study to validate or refute the suspicions.
A Telemetry Utilization Review project was implemented by the directors of inpatient services in conjunction with the Patient Placement Center. This project was implemented for several purposes:
- to evaluate whether patients currently on telemetry still required continuous cardiac monitoring,

- to evaluate the length of time patients remained on telemetry,

- to improve the emergency department’s throughput, and

- to evaluate the potential need for additional telemetry beds within the adult medical division.
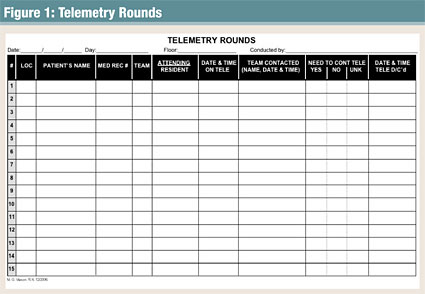
An audit tool (Figure 1) was developed and implemented to determine if patients currently admitted to telemetry truly needed to continue with cardiac monitoring or if telemetry could be discontinued. The associate medical director of inpatient services, who reviewed each chart and discussed the patients’ needs with their admitting physicians or teams, completed the utilization review twice a week. The clinical decision of need was based on the guidelines set forth by the American College of Cardiology (ACC; Emergency Cardiac Care Members, 1991). On the first day of the audit, more than 50% of the patients on telemetry monitoring were identified as not requiring further monitoring and were subsequently discontinued after case-by-case discussions were held with the admitting physicians. Over the course of 6 months, over-utilization of telemetry was prevalent during each audit. A total of 736 charts were reviewed from the two telemetry wards, of which 651 were ordered for and were placed on telemetry. Of the 651 telemetry patients reviewed, 354 (54.4%) were identified as no longer meeting the criteria set forth by the ACC. The audits also revealed 120 (18.4%) of these patients did not meet any criteria for cardiac monitoring upon admission (Table 1, pg. 28).
![]()
| Table 1: Most Commonly Misused Telemetry Diagnoses |
||
Although prior to the audits a hospital-wide guideline existed regarding which patients should be placed on telemetry monitoring, the guideline was largely ignored by the house staff and was in need of revision. The audit tools again came into play as a valuable resource of information in revising the outdated guideline. The audit tool conveniently included a justification column for why the patient required telemetry (Figure 1). The justification column eventually served as the basis for the revised guideline; the diagnoses led to the development of the specific criteria for the new guideline as well as selected literature researches (primarily that of the ACC criteria).
Once the new guideline was accepted and approved by the various medical directors, reinforcement was the next task. A Telemetry Authorization Form was developed (Figure 2, pg. 29), and both the medical and nursing staff were instructed on the purpose and use of the form. The form initially was considered a “work product” and not part of the patient’s medical record; however, with the recent implementation of computerized charting within the facility, the justification has become part of the permanent medical record. The admitting physician is required to complete the justification form at the time of ordering telemetry. Based on the diagnosis selected, the physician is required to renew the telemetry order at 24, 48, or 72 hours. All new telemetry orders and renewal orders are reviewed by a registered nurse. If the order is questionable or appears unnecessary, the directors of inpatient services are called to review and approve or deny the telemetry order. While the computerized documentation is being implemented, the paper form is still being required of the admitting physician as part of the ongoing study.
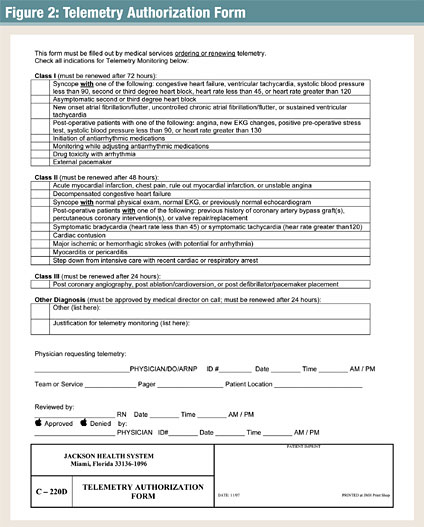
![]()
The authorization form is divided into 3 major classes and is directly based on the revised guideline: Class I contains criteria for telemetry monitoring typically for up to 72 hours, Class II for up to 48 hours, and Class III for up to 24 hours of cardiac monitoring.
If a patient does not meet any of the criteria listed within the three classes, a fourth section on the form allows the physician to write in the justification. The non-classified justification requires written approval by the in-house hospitalist director on call. Prior to issuing telemetry beds to admitted patients (from either the emergency services department or the various adult floors), the patient placement coordinators (registered nurses with strong clinical and administrative backgrounds) require the requesting physician to complete the form and are notified by the various charge nurses of the form’s completion and the validated need for telemetry.
Since the facility has recently implemented a hospital-wide computerized documentation system for medical records, electronic order sets are being developed to incorporate a mechanism for automatically notifying the physicians for the need to review, renew, or discontinue telemetry orders based on the guideline. The automated telemetry order expiration/renewal alerts would help to eliminate the manual task of reviewing each patient’s orders in accordance to the telemetry guideline, reducing the manpower hours in ensuring appropriate adherence to the guideline.
The new guideline also encourages the admitting physicians to employ better critical thinking by considering more aggressive plans of care to expedite patient care, maximize throughputs, and initiate earlier discharge planning. A list of the commonly misused diagnoses was shared with the physician group to help them to rethink or reconsider when ordering cardiac telemetry monitoring (Table 1).
Results
After 6 months of the implementation of the Telemetry Authorization Form, the number of patients waiting for a telemetry bed was significantly reduced. On a typical day, the number of patients waiting in the emergency department for a telemetry bed decreased by an average of 60%. Some of this decrease was attributed to the rapid identification and discontinuation of patients from the individual telemetry floors. Part of this decrement was also due to the denial of inappropriate admissions to the telemetry wards.
With the decrease in the use of telemetry beds, the need for telemetry beds in the emergency services department has been notably decreased. Unused in-house telemetry beds are often utilized for general medical admissions not requiring telemetry in an effort to meet the increased need for general medical beds and to offset and maintain a balanced budget for the affected floors. In short, instead of leaving staffed telemetry beds unoccupied, the beds (and nursing personnel) are being utilized to alleviate the burden of non-telemetry admissions being held in the emergency department.
With the acquisition of two more hospitals to form the Jackson Health System (JHS), the telemetry guideline and authorization form were shared with Jackson North Medical Center (formerly Parkway Hospital, North Miami, Florida) and Jackson South Medical Center (formerly Deering Hospital, Homestead, Florida). The guideline and form were well received by the respective medical directors and subsequently adapted for the entire Jackson Health System.
Other Institutions Study Overuse of Telemetry
Jackson Health System is not the only healthcare institution looking at the overuse of telemetry. A recent publication by The Joint Commission Journal on Quality Improvement revealed a similar quality improvement program at Hackensack University Medical Center (Hackensack, New Jersey) in 2002. In this program, nurse practitioners found a decrease of 34% of time on telemetry monitoring over an 11-month period (Gross, 2002). Similarly, at Jackson Memorial Hospital, the need for continuous and ongoing utilization review was identified as each academic year brings new house-staff onto the various medical teams and services.
Additionally in 2005, the medical administration at Portland Veterans Affairs Medical Center implemented a utilization guideline system, which incorporated stop times for telemetry. These were incorporated to have physicians review the need for continued telemetry monitoring (Church, n.d.). This project was then shared throughout the Veterans Affairs system.
Likewise, in a study performed by Dr. Carlos Estrada (1994) and his colleagues at the Henry Ford Hospital in Detroit, Michigan, 467 patients were admitted to telemetry based on the ACC guideline for telemetry monitoring. Of these patients, telemetry contributed to the decision of transferring patients to intensive care in 1% of these cases. Furthermore, patients who did deteriorate while on telemetry wards were identified clinically without findings on the monitor. In another study by Estrada (1995), data was collected from 2,240 patients admitted to telemetry with chest pain, arrhythmias, heart failure, and syncope. From the second study, Estrada found telemetry helpful in modification of management in only 7% of patients.
Initially many of the physicians at Jackson Memorial Hospital saw the revised telemetry guideline as a bit radical in nature and the justification process as “another hoop to jump through.” Ultimately the same physicians admitted the new guidelines and justification process have had a positive impact from many aspects.
In summary, deployment of both the new guideline and justification process has significantly reduced over-utilization of telemetry services while decreasing some of the overburdening of the emergency services department. As a result of this study and subsequent implementations, the length of stay has been decreased on the telemetry wards and the need for an additional telemetry ward was deemed unnecessary.
Mitchell Mason is a patient placement coordinator at the University of Miami/Jackson Memorial Hospital. He is a 1985 graduate of Hocking College School of Nursing in Nelsonville, Ohio, and a 1981 graduate of Ohio University’s College of Education. For 17 years, he worked in the emergency department as a trauma nurse specialist, assistant nurse manager, and clinical resource coordinator. Mason has authored several other publications and freelances as a professional consultant/expert witness for various attorneys throughout Florida.
Richard Lapin is the chief of service of the hospitalist service of the Jackson Health System. He received his undergraduate and medical degrees at UCLA, along with a master of public health degree. He is board certified in internal medicine. He is currently involved in numerous projects to expand the hospitalist service along with the Jackson Medical Group. He has also been involved in forming partnerships with the Florida International University College of Medicine.
References
Church, V., et al. (n.d.). Improving outcomes with telemetry monitoring performance improvement initiatives, Available at http://www1.va.gov/
nursing/docs/7_ImprovingOutcomesWithTelemetry.doc.
Emergency Cardiac Care Committee members. (1991). Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Journal of the American College of Cardiology, 18, 1431-1433.
Estrada, C. A., et al. (1994). Outcomes of patients hospitalized to a telemetry unit. The American Journal of Cardiology, 74, 357-362.
Estrada, C. A., et al. (1995). Role of telemetry monitoring in the non-intensive care unit. The American Journal of Cardiology, 76, 960-965.
Gross, P., et al. (2002). A nurse practitioner intervention model to maximize efficient use of telemetry resources. The Joint Commission Journal on Quality Improvement. 28(10), 566-573
