Building a PSO “Field of Dreams” for Emergency Medical Services
November / December 2010
![]()
Building a PSO “Field of Dreams” for Emergency Medical Services
“Oh… people will come, Ray. People will most definitely come.”
– Terrance Mann, Field of Dreams, 1989.
For emergency medical service (EMS) providers in the state of Missouri, patient safety organizations are a “field of dreams”—a field of legal protection, learning, collaborating, and most of all, improving pre-hospital care.
While many hospitals and other providers are still struggling to fully appreciate the breadth of federal legal protections and other benefits available from working with patient safety organizations (PSO), the Missouri Ambulance Association (MAA) recognized the value months before the final rule was even published. In Missouri, EMS providers—the paramedics, EMTs, and others who respond to 911 calls—have no peer review protection for their quality improvement and patient safety work. Their principal fear was that any well-intentioned efforts at safety and quality improvement had the potential to be subpoenaed and used against them in legal proceedings. When representatives from the MAA began hearing about the Missouri Center for Patient Safety (MOCPS) and PSOs in general, they paid attention.
It was not for lack of trying that Missouri’s EMS providers had no peer review protections. Since 1996, the MAA had lobbied for nearly 20 different bills, only one of which came close to passing. Ultimately, according to Jason White, consultant for the MAA, the bills were mired in other political agendas, and the pieces related to peer review protection for EMS were always removed. In 2006, Becky Miller, executive director of the MOCPS, was making a series of presentations to various groups around the state to introduce the Center and to provide early education on PSOs. Miller presented to the EMS State Advisory Council in 2006, and got the attention of the late Dr. Bill Jermyn, then EMS medical director for the Missouri Department of Health and Senior Services (DHSS). After hearing Miller speak, Jermyn informed White that working with the PSO might very well be the solution to peer review protection. At the time, the MAA dismissed the idea. They still hoped they would succeed in getting a bill passed, but came to realize 2 years later they needed to search elsewhere for a solution.
Missouri EMS providers historically have desired to improve the quality and safety of their services; in fact, at one point in time, Missouri was considered to be very progressive with EMS data collection. Missouri ambulance services have been required by statue to report trip information for all life-threatening responses to the Missouri Ambulance Reporting System (MARS), operated by the Missouri DHSS, since late 2004. In return for this data submission, ambulance services thought they would be able to obtain meaningful reports to assist with performance and quality improvement activities, but they have been extremely disappointed. White notes that reports are available, but they are rudimentary and not very useful. State budgetary issues have hindered the DHSS from developing more robust reporting capabilities.
National Efforts
On a national level, the EMS industry is making great efforts to catch up with hospitals in the world of quality improvement and patient safety. A national EMS database was formed in 2003 through a project called the National EMS Information System (NEMSIS). This system was developed as a means to capture ambulance trip information from all 50 states in a national repository to provide the ability to examine EMS systems at local, state, and national levels; evaluate patient outcomes; and provide other valuable information on areas of need (NEMSIS, 2010). The Missouri DHSS has been transmitting all of the MARS data to NEMSIS since July of 2008 and was recognized as being NEMSIS compliant in April of 2009.
A new EMS reporting system called EVENT—The EMS Voluntary Event Notification Tool—was recently launched by the Center for Leadership, Innovation and Research in EMS. It allows any EMS provider in the United States or Canada to anonymously report any type of event via a website (CLIR, 2010). The data elements are based upon those first developed by the Commonwealth of Pennsylvania for use by their EMS providers, and are somewhat limited; for Missouri EMS providers, however, there is no legal protection for data they might enter in to this system. Additionally, The University of Pittsburgh Center for Research in Emergency Medical Services established the EMS Agency Research Network (EMSARN) in January of 2010. They are focusing on specific aims to improve quality, safety, and performance in EMS systems nationwide through research and data collection (EMSARN, 2010). Other EMS patient safety and quality improvement work has been carried out on an organized basis in several parts of the country—North Carolina; Rochester, New York; Minnesota; and Contra Costa County, California to name a few—but streamlining an industry-wide national effort at improving EMS patient safety has been a challenge. As throughout healthcare, these efforts are only a beginning.
First Pitch
In early 2008, after more failed legislative attempts at peer review protection, White, then director of compliance and government relations for MAST Ambulance in Kansas City, Missouri, and Mark Alexander, director of pre-hospital services for CoxHealth EMS in Springfield, Missouri, began to talk with MOCPS to learn more about the Patient Safety and Quality Improvement Act, PSOs, and what type of data and information could be submitted and protected under the PSO umbrella. They began by meeting with the Missouri Hospital Association (MHA), one of the Center’s founding members, to discuss EMS’s desire to enhance quality, and its need for peer review protection similar to that available to hospitals. Miller recalls receiving a call from the MHA that same day, to let her know they were sending White and Alexander her way, and within 24 hours, Miller, White, and Alexander were discussing PSOs face-to-face. Their meeting quickly led to a mutual agreement that the Center, as a PSO, would help Missouri’s EMS providers not only establish a coordinated way to report, learn, and improve the quality and safety of pre-hospital care, but also provide the necessary federal legal protection and confidentiality for such work. The relationship would also integrate Missouri’s EMS providers with other work of the Center, including efforts to improve the culture of safety. What was left to do? Final federal regulations were required so the Center could certify as a PSO; education of the EMS community was needed to obtain buy-in, and funding was an absolute essential. Each party left the meeting committed to continuing discussions to move the project forward.
November of 2008 marked the initial listing of PSOs by the Agency for Healthcare Research and Quality (AHRQ), and the MOCPS was the tenth organization in the nation to do so. The Center’s meetings with the MAA continued; the more they learned about the possibilities of working with a PSO, the more the MAA wanted to find a way to make this a reality.
Throughout 2009, White and Alexander began a grassroots campaign among their membership, educating the gamut of ambulance services—from very large, hospital-based or city fire department-based systems, to very small, rural ambulance districts—on the potential benefits of working with a PSO. A meeting was hosted by MOCPS in June of 2009 that included numerous paramedics, nurses, flight medics, medical directors, and ambulance service directors that represented well over 65% of Missouri’s EMS call volumes, as well as representatives of the Missouri DHSS, Bureau of EMS. It became apparent to MOCPS very quickly that this group was serious about wanting a way to collect patient safety information, learn from it, and gain legal protection in the process. As the attendees asked thoughtful, pointed questions, and the discussions continued throughout the day, the energy and ideas were pulsing around the room. Everyone slowly began to understand how this would work, and the possibilities of “what could be.” By the end of that meeting, the Center was certain there was enough support to carry the project through from concept to implementation.
The Dream Begins
From the beginning, MOCPS knew that building customized PSO data collection services for EMS providers would not be an inexpensive or easy task. Existing software platforms are built from the Agency for Healthcare Research and Quality’s (AHRQ) common data formats for PSOs, which are geared mostly for hospital-oriented medical errors and adverse events. However, the Missouri EMS community was not interested in just capturing “the things that shouldn’t happen.” They envisioned the opportunity to capture data proactively, such as key quality indicators for pre-hospital care of ST-elevation myocardial infarction (STEMI), stroke, and trauma patients. They also recognized the need to improve the overall culture of safety in EMS, not only in Missouri, but across the industry nationwide.
Even beyond that, the “home run” they are truly aiming for is an electronic means of obtaining hospital outcomes—what happens to their patients after arrival in the emergency department? Currently, very little outcomes data is shared, which is attributable to the lack of legal protection for ambulance services in the state. Particularly if there is a negative patient outcome, Missouri hospitals in general have been reluctant to provide this information to the originating ambulance service. Obtaining outcomes data through electronic data collection under the PSO umbrella could be a solution.
So without a readily available cornfield to devote to this endeavor, a flurry of activity began with drafting a grant proposal to the Missouri Foundation for Health. A committee was formed from the attendees of the June 2009 meeting, each helping to build the case for why this capability was needed, how much it would cost, and where the funds would be expended. There wasn’t long to wait. In September 2009, only 3 months after the Missouri EMS community and MOCPS began working together, they received word they had been awarded $595,000 over 3 years to build their “field of dreams.”
Off and Running
The project went from possibility to reality very quickly, and so did the work group. The team met in October of 2009 to formalize the membership; agree on a mission, vision, and project plan; and strategize recruitment of other EMS agencies. The goals for the grant period appeared simple enough:
- obtain at least 50% of Missouri’s EMS agencies participating in the PSO by end of the grant;
- develop a minimum set of at least 10 patient safety and quality indicators; and
- establish an organizational safety culture within a minimum of 30 EMS agencies by the end of the grant.
Two subcommittees were established: one to work on the data system specifications and another to tackle the safety culture project, with most of the core work group members signing up for one or both.
With a project of this magnitude and little previous work to build upon, MOCPS had to find where the “start here” arrow pointed. Without knowledge of what specific issues were “burning” with Missouri EMS providers, a very informal survey was sent to ambulance services around the state to ask their opinion on reporting events based on a broad, general definition compared to specific, individually-defined events. Responses favoring one method over the other were split almost in half. However, the comments supporting reporting by individually defined events were all in agreement; reporting on broad-based definitions leaves too much open to interpretation and would lead to inaccurate reporting.
That confirmed the work group’s initial impression, so the survey was refined to drill down into the specifics: what types of errors did the respondent feel to be most frequent and which are most likely to be reported to a PSO if legal protections were in place? Out of a list of eight potential events provided, respondents were asked to choose four events they felt were the highest priority and/or most frequently occurring. From 125 responses to those questions, MOCPS gleaned a list of five top concerns: medication errors; equipment failures/malfunctions with adverse outcome or patient injury; intubation errors (all types); incorrect paramedic impression leading to incorrect treatment protocol; and ambulance crashes with patient injury (Fig. 1).
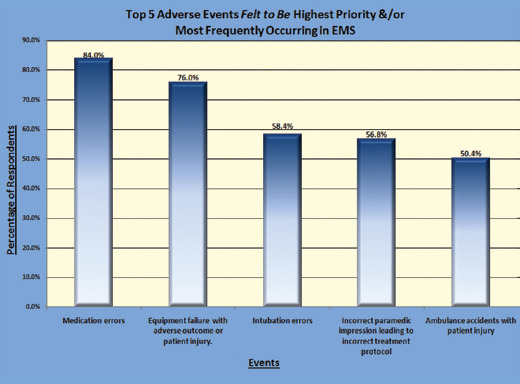
Figure 1: Top 5 Adverse Events Felt to be Highest Priority/Most Frequently Occurring in EMS
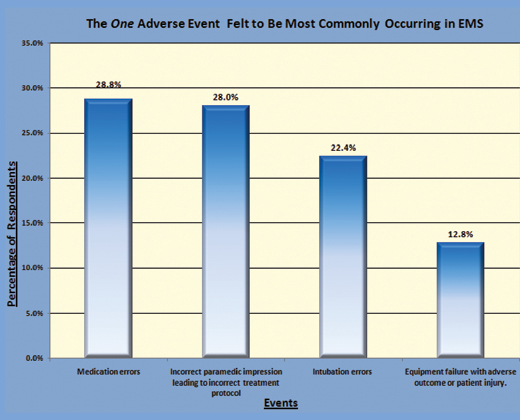
When asked to narrow the list down to the single most commonly occurring event, medication errors and incorrect paramedic impression leading to incorrect treatment protocol almost tied, followed by intubation errors, and equipment failures (Fig. 2, pg. 24).
Finally, for curiosity, the work group wanted to know which events the respondents felt were most likely to be reported with the appropriate PSO legal protections in place. Ambulance crashes came in first, followed by equipment failures and medication errors (Fig. 3, pg. 24). With this information in hand, the committees were ready to begin.
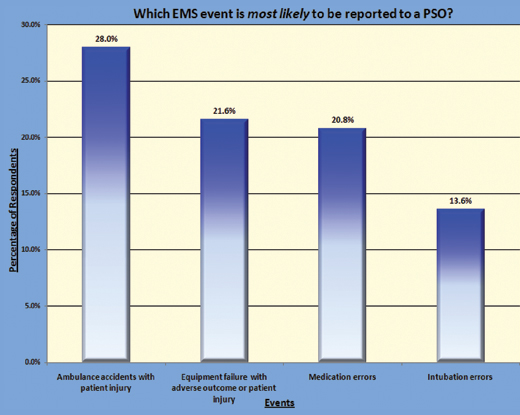
Figure 3: EMS Event Most Likely to be Reported to a PSO
Building the Data “Field”
As previously mentioned, the existing data elements contained within the common data formats are not necessarily congruent with EMS settings. The Center consulted with Quantros, its PSO data vendor, to confirm that it would be best to begin by dissecting the common data formats as they already existed in the data system. The data sub-committee began in earnest.
Charged with the arduous task of combing through the Center’s PSO database, the data committee has met every other week since December of 2009 via a 90-minute conference call to discuss, propose, (and sometimes disagree) over every data point in the system. Ideas were generated at nearly every turn; the committee has been challenged to stay focused on first steps before moving on to create what truly does not exist. Modifications for the EMS environment were made where possible, some new data points added, and other items hidden or removed. The committee has been extremely fortunate to have one member who is a physician and owner of a private ambulance service, who also happens to have a computer science and programming background. He has assisted by informing the group of some of the “ins and outs” related to programming logic, and how this dataset can mesh with other EMS data sets, such as the previously mentioned NEMSIS data standards, or state crash reporting databases.
With the makeover of the existing PSO database completed, the data committee turned to creating some of what did not exist. Airway management events are a known problem throughout EMS, as are ambulance crashes, both of which came out in the survey. Our committee was able to borrow some elements from the NEMSIS data set to capture much of the needed information for airway management errors, which Quantros was more than willing to mesh in to the existing PSO data system. Ambulance crashes followed, borrowing elements from highway patrol accident reports and other data collection mechanisms, to begin building an entirely new set of data that does not exist in any type of organized or structured basis.
Quality indicators for pre-hospital care of STEMI and stroke patients, such as time to diagnosis, transport times, 12-lead EKG acquisition and interpretation, and transfers between Basic Life Support and Advanced Life Support units, are also slated to be included in the initial data set. Quantros has been flexible and responsive in working with the committee’s ideas, offering suggestions and guidance where needed, and a willingness to do whatever they can to meet our aggressive timeline. Testing of the data system is slated to begin in November 2010, with live data collection commencing in January or February of 2011.
Building a Culture of Safety
While the data “field” is being built, the EMS safety culture “field” is getting a good turnover and some new sod. The safety culture subcommittee, or “Culture Club,” began meeting early in 2010 to brainstorm about the best and most practical method of planting the seeds of a non-punitive safety culture in EMS. Members from hospital-based ambulance services had received some prior instruction and training on Just Culture from Outcome Engineering when their organizations participated in the MOCPS statewide Just Culture collaborative in 2007 and 2008. The basic concepts of Just Culture were offered to this group, and all were confident this philosophy would resonate with their peers. The committee also discussed the communication and team-building tools from the TeamSTEPPS™ program from AHRQ, offering an overview of those materials and viewing the video scenarios. The committee felt it would be important to add this as part of the safety culture project.
To help demonstrate the establishment of an organizational safety culture within participating EMS agencies by grants’ end, we needed a method of measurement. Research on safety culture and attitudes in the EMS industry has begun to appear in the literature in recent years. Fairbanks et al. (2008) utilized in-depth interviews with EMS personnel to get a sense of provider perceptions regarding near misses and adverse events. Common themes emerged, with specific comments from participants such as “When you ask (medical control) for an attending (ER physician), you get an attitude,” and “What happens in the rig stays in the rig,” suggesting a climate of “blame-and-shame” and a tendency to not report events and near misses when they occur. Patterson et al. modified the validated Safety Attitudes Questionnaire (SAQ) to capture safety culture in EMS, and after an initial study, have built a national database specifically for various EMS agencies to enter or upload survey results from their service. They recently published results of over 1,700 respondents and found great interagency variation in workplace safety culture. The real question lies, however, in whether or not a patient’s safety is more at risk in the hands of those working in the lower scoring agencies, versus the higher scoring ones—and there is currently no answer for that question (Patterson et al., 2010).
The group’s overall goal for participating ambulance services is not only for the service to receive legal protection for this information, but to help them begin to change the safety attitudes and culture among supervisors and front line staff. Therefore, administration of a shortened version of the EMS-SAQ to obtain a baseline safety culture measurement is a requirement of participation in the EMS PSO, with a follow-up survey to be completed by those same agencies post-intervention at the end of the grant.
The intervention piece began with a Just Culture Manager’s Training workshop held in July 2010 with more than 100 Missouri EMS providers in attendance. The class and content received rave reviews, but a common theme emerged: the training materials and workbook needed modification to better suit an EMS audience, as most of the case studies are geared towards hospital environments. MOCPS had collected some EMS scenarios, which were utilized for group work and discussion, but many felt very strongly that more could be done.
The work group approached David Marx, the creator of the Just Culture materials and asked if his materials, including the staff training video, could be re-created for an EMS audience. He accepted the idea enthusiastically. The Missouri EMS providers have agreed to assist with the technical aspects of providing ambulances, helicopters, locations, and other details, and Outcome Engineering will work on the rest. It is anticipated the new materials will be available in early 2011. A mechanism to recreate some of the TeamSTEPPS™ training video scenarios in an EMS setting is also being developed.
|
TECHNOLOGY & PARTNER OVERVIEW
Outcome Engineering – Curators of the Just Culture Community. http://www.outcome-eng.com/justculture.html |
If You Build It…
…people will come. All indicators point in that direction. The project has already received interest from national EMS organizations and highly regarded industry professionals, as the EMS world is ripe for significant change. This project offers an opportunity for EMS providers to progress into the wider mainstream of healthcare as they begin to learn and use the terminology, tools, and techniques that have become commonplace in the acute care setting. The coming year will be exciting as live data is collected, data system development continues to include interfacing with the MARS and hopefully with hospital discharge data, and the seeds of a safety culture are planted, where street-level medics can feel safe reporting errors without retribution.
REFERENCES
EMS Agency Research Network. Retrieved September 9, 2010, from http://www.emsarn.org/About_EMSARN.html
Fairbanks, R. J., Crittenden, C. N., O’Gara, K. G., Wilson, M. A., Pennington, E. C., Chin, N. P., & Shah, M. N. (2010). Emergency medical service provider perceptions of the nature of adverse events and near-misses in out-of-hospital care: An ethnographic view. Academic Emergency Medicine, 15, 633-640.
NEMSIS Technical Assistance Center – What is NEMSIS? Retrieved August 7, 2010, from http://www.nemsis.org/theProject/what?IsNEMSIS/index.html
Patterson, D. P., Huang, D. T., Fairbanks, R. J., Simeone, S., Weaver, M., & Wang, H. E. (2010). Variation in emergency medical services workplace safety culture. Pre-Hospital Emergency Care, 14(4), 448-460.
|
ACKNOWLEDGMENTS |
