Building a Culture of Safety
September / October 2007
Building a Culture of Safety
Creating a Reliable and Sustainable Patient Safety Infrastructure through Teamwork Training
The healthcare industry is held increasingly to a standard of flawless performance in an environment where it can be very difficult to manage human error. There is little disagreement about the vital need for effective communication and collaborative decision-making in healthcare scenarios. However, these behaviors are often the missing components in achieving higher standards of patient safety and satisfaction, resulting in unnecessary and tragic outcomes that might be prevented with the implementation of human interaction training. These curriculums establish and maintain permanent processes of teamwork and a true culture of safety in medical settings, ultimately improving patient care.
Several reports have highlighted the impact human coordination and decision-making errors have on patient safety. In 1999, the Institute of Medicine released a landmark report entitled, To Err Is Human: Building a Safer Health System. This report became a catalyst for research into healthcare errors and injuries, as well as potential solutions to improve care and create safer processes. The years since this report was published have demonstrated that patient safety is a public health priority and that attacking medical mistakes effectively requires new mental models, research, technologies, and training.
Moreover, in review of national sentinel event statistics, the Joint Commission has identified that problems in communication and teamwork have an overall effect on healthcare facilities’ culture of safety. Specifically, the Joint Commission found that 72% of injuries in the perinatal setting were related to a breakdown in communication, as stated in the most current review of Root Causes of Perinatal Death and Injury (The Joint Commission, 2007). More than half of the surveyed organizations cited organizational culture, such as hierarchy, as a barrier to effective communication and teamwork.
These studies and others indicate that teamwork training is imperative to patient safety. Team-training programs seek to bridge the gap between autonomous decision-making and a system of empowered individuals truly working as a team to ensure results that are in the best interest of healthcare workers’ number one priority — the patients.
Team Training in Action: Catholic Healthcare West
One healthcare system that is currently experiencing the benefits that teamwork training can bring to patient care is Catholic Healthcare West (CHW). Headquartered in San Francisco, CHW is a system of 43 hospitals and medical centers in California, Arizona and Nevada. Founded in 1986,ÝCHW isÝthe eighth largest hospital system in the nation and the largest not-for-profitÝhospital provider in California. The CHW hospital network is implementing team training as a means of reducing medical errors, especially in the area of perinatal care, where CHW determined the need for teamwork to be particularly pronounced.
 Public expectations and attitudes regarding the delivery process and newborn care are very high. Medical errors leading to injury or death often result in patients and families seeking legal restitution, leading to costly lawsuits. Because nurses practice with great autonomy in these specialized units, accurate assessment and communication of fetal and baby well-being has an effect on overall patient outcome. Teamwork is essential in this dynamic environment, of which a culture of safety is a core component. In analysis of the network’s perinatal services, CHW determined that one of the most common causes of injury involved lack of communication and utilization of the chain of command.
Public expectations and attitudes regarding the delivery process and newborn care are very high. Medical errors leading to injury or death often result in patients and families seeking legal restitution, leading to costly lawsuits. Because nurses practice with great autonomy in these specialized units, accurate assessment and communication of fetal and baby well-being has an effect on overall patient outcome. Teamwork is essential in this dynamic environment, of which a culture of safety is a core component. In analysis of the network’s perinatal services, CHW determined that one of the most common causes of injury involved lack of communication and utilization of the chain of command.
CHW implemented team training as part of the organization’s Pursuit of Excellence initiative, which seeks to ensure that employees are adequately trained and supported to provide the best patient care possible. The 3-year initiative combined data collection, teamwork training and structured leadership oversight to improve the climate of safety in perinatal services at 38 CHW facilities. An ongoing project, the goal of this implementation is to improve the culture and attitude of patient safety that has been associated with a reduction in staff turnover rates, patient length of stay and errors in care. Four of the CHW hospitals do not have a perinatal service. In those hospitals, the focus area is the emergency department.
The CHW Pursuit of Excellence initiative began data collection for the training program with the administration of the Safety Attitudes Questionnaire and Safety Climate Survey™ (SAQ) (Sexton 2006) prior to the initial training. This tool was selected based on its high reliability and validation. The hospitals were provided their results, allowing them to identify their key areas of concern.
CHW then selected a teamwork training program to use at all of the facilities. To begin the training process at CHW, each hospital selected two or three individuals to become certified teamwork trainers. These participants included physicians, nurses and educators who were responsible for teaching the aspects of teamwork to the perinatal or emergency department staff and physicians from their facilities. In June 2006, the selected CHW trainers were brought to one location for the instructor training program. Outside of the military, this was the largest undertaking of a teamwork training program to date. The initial training session certified 86 individuals in a train-the-trainer methodology that enables each site to become grounded in the concepts.
Each of the 38 sites determined the staff to be trained at their site. In larger organizations, this usually included all of the perinatal services as opposed to the smaller or rural sites where it was just the OB/GYN physicians and the L&D nursing staff. Once the target audience was determined by a site, the metric for progress and completion of the training was based on the identified target audience. Various staff participated in the teamwork training classes and programs, including RNs, certified nurse midwives, OB/GYN physicians, family practice physicians, anesthesiologists, residents, respiratory care providers, neonatology physicians, perinatologists, neonatal intensive care unit nurses, postpartum nurses and unit support staff. The program is currently in progress; there are 3,100 total staff members participating at the hospitals, and 600 physicians have participated in education sessions to date.
Structured consultation by teamwork experts and follow-up activities to monitor the sites’ progress were ongoing throughout the process. Scheduled conference calls allowed the sites to discuss their training and implementation status and seek suggestions for similar problems. Staff from CHW Risk Services and the teamwork consultants worked with individual sites if needed to problem-solve any issues that arose around the initiative.
Although each CHW site teaches the same basic course, training is just the beginning of the process of change. The implementation of learned behaviors into the day-to-day life of the units is the critical part of the intervention. Since the sites vary from rural hospitals to large, metropolitan, teaching medical centers, the implementation process is as diverse as the facilities. One consistent factor is the support from the executive leadership at each of the 38 sites. Experience has shown that the combined effort of the teamwork trainers, executive leadership, and department leadership makes the implementation of teamwork behaviors successful in most units.
At this point in the program at CHW, there are a few common stumbling blocks that have been observed across the system. Most sites have been able to easily and effectively manage these challenges. Some of the more common issues have been:
Identifying champions. Making sure that the right individuals and groups are part of the change team is a key step. In order to model the multidisciplinary, collaborative environment that is the goal of teamwork training, it is important that both nurses and physicians are on the initial change team. In coordinating the CHW train-the-trainer program with 38 sites, not all sites were able to send a MD “champion” to the training. This meant that the nurses needed to go back and relay information from the initiative to MD champions, causing delays. The program is strongest when clear champions from both groups are working together to facilitate the training and implementation.
Physician buy-in and participation. Most CHW sites are primarily staffed with private practice physicians. Recognizing the unique challenges in motivating the physicians to participate in the training and creating opportunities to facilitate their training was identified as a major concern for most of the sites. Numerous sites provided training after regular office hours, on Saturday mornings or associated with a meal to encourage the physicians’ attendance. Use of mid-point metrics to monitor physician participation in the training allowed the sites to identify when different tactics were needed to accomplish the 100% teamwork trained goal. This sometimes included bringing in an “outside” MD champion to provide the training or a motivational presentation identifying the benefits of a teamwork trained environment.
Changing leads. These days, attrition of staff is part of the healthcare world. In a program of this magnitude, the vacancy created by one of the initial champions leaving the hospital created difficulties for a few sites. In some instances, offering an additional instructor training session provided the opportunity for the new lead to learn the program facilitated by support from the CHW Risk Services staff and the teamwork consultants.
Maintaining momentum. Changing behavior takes time. Above all, the first priority of health care workers is to care for patients. For most of the sites, momentum was maintained through the CHW- imposed timeline for initial training, data collection and implementation. On-going encouragement from the sites’ executive leaders is vital as the network rolls out the mid-point data results to the sites and moves toward sustainment.
While success stories have been reported since the training was rolled out, real validation comes from the numbers. The initial SAQ focused, for measurement purposes, on the safety climate subset of questions. These results serve as the baseline for pursuant surveys and show that 76% of CHW sites were in the safety climate danger zone. This means that less than 60% of the participating staff agreed that patient safety was going well in the unit. However, the second survey, given following the implementation of team behaviors and approximately 1 year after the baseline study, indicated only 47% were still in the safety danger zone, an improvement of 13%.
Improvement in the score for the “teamwork” subset of the SAQ was identified after the second administration. When interpreting the results, it was noted that improving “teamwork” domain scores is a precursor to improved “safety climate” scores. This information proved to be an encouragement for the system overall.
The final application of the SAQ will be conducted in April 2008 as a final measurement of progress in improving the climate of safety.
Team Training as a Patient Safety Infrastructure for the Future
Although research demonstrating the value of teamwork in the clinical setting is in its infancy, results continue to indicate that the use of a concrete teamwork model, based on the aviation principles of CRM, can improve the efficiency of care delivery and outcomes for patients. Early research of the teamwork model has successfully demonstrated its usefulness as a patient safety and performance enhancement intervention in emergency care to reduce medical errors and improve patient satisfaction.
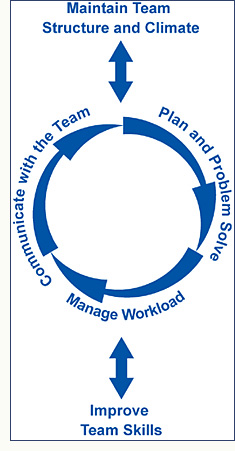
In team training, teamwork is seen as an infrastructure for decision-making, care delivery and communication within patient focused units. This is what CHW seeks. Having all clinical or patient-centered staff trained in teamwork principles creates a standard of care and communication at every level that will improve safety for patients.
Team-training initiatives involve not only the training of teamwork behaviors, but from a broader perspective, require a change in the conditions and working arrangements within the patient care units. Viewed as an infrastructure, teamwork must be approached by the organization as a fundamental culture change initiative that has its best chance of succeeding using solid culture change theory and principles (Kotter 1995; Katzenbach and Smith, 1993).
As with any quality improvement strategy, a timeline exists for adopting a teamwork system. This timeline includes a wide variety of short-term preparations, mid-term training and implementation activities, as well as long-term follow through to sustain the program. When viewing teamwork as an infrastructure, the transformation of the healthcare environment also depends on the vision and commitment of both senior leaders and clinical staff. Some effects of teamwork training may be felt almost immediately, while the full integration of teamwork at every level of the organization is a longer process. It must be understood that the complete change to teamwork may take several years to accomplish.
Vinette Langford is director for MedTeams and Healthcare Programs for the Training Development and Implementation Business Unit of Dynamics Research Corporation in Andover, Massachusetts. Langford provides expert consultation and program management services for all of DRC’s MedTeams customers and other healthcare contracts related to high performance team training or medical skills training. Possessing over 25 years of experience in emergency nursing covering both clinical and management roles, Ms. Langford also maintains extensive experience in educational program planning relative to both individual offerings and multiple-day programs. She may be contacted at or VLangford@drc.com.
Victoria Rollinsis a loss prevention specialist in risk services for Catholic Healthcare West in San Francisco. The focus of this work is risk prevention, patient safety, risk analysis, risk reduction, and risk mitigation. As a registered nurse with more than 25 years of healthcare experience, Rollins has practiced in settings including medical, surgical, ICU, and cardiac catheterization laboratory. Her management experience includes ICU, post-ICU and telemetry units, nursing administration, nursing project management, and administrative supervisors. Rollins holds an associate degree in nursing, a bachelor’s degree in health sciences, and a master’s degree in healthcare administration. She is a Certified Professional in Healthcare Risk Management, a member of the national nursing honor society, the American Society of Healthcare Risk Managers, and the California Society of Healthcare Risk Managers.
References
The Joint Commission (2007). Perinatal deaths & injuries. Sentinel Event Statistics-March 31, 2007: Root Cause Statistics. http://www.jointcommission.org/SentinelEvents/Statistics/
Katzenbach, J. R., & Smith, D. K. (1993). The discipline of teams. Harvard Business Review, 111, 120.
Katzenbach, J. R., & Smith, D. K. (1993). The wisdom of teams: Creating the high-performance organization. New York: Collins.
Kohn, L. T., Corrigan, J. M., Donaldson, M. S. (1999). To err is human. Washington, DC: National Academy Press.
Kotter, J. (1995). Leading change: Why transformation efforts fail. Harvard Business Review. PN4231, March-April; 59-67.
Kotter, J., & Rathgeber, H. (2006). Our iceberg is melting: Changing and succeeding under adverse conditions. New York: St. Martin Press.
Morey, J. C., Simon, R. J., Jay, G. D., Wears, R. L., Salisbury, M., Dukes, K. A., & Berns, S. D. (2002). Error reduction and performance improvement in the emergency department through formal teamwork training: Evaluation results of the MedTeams® project. Health Services Research 37(6), 1553-1581.
Sexton, J. B., Helmreich, R. L, Neilands, T. B., Rowan, K., Vella, K., Boyden, J., Roberts, P. R., & Thomas, E. J. (2006). The safety attitudes questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Services Research, 6, 44. http://www.biomedcentral.com/1472-6963/6/44/abstract
Sexton, J. B., & Thomas, E. J. The Safety Climate Survey: Psychometric and Benchmarking Properties. Technical Report 03-03. The University of Texas Center of Excellence for Patient Safety Research and Practice (AHRQ grant # 1PO1HS1154401 and U18HS1116401).
