Be Prepared: Anticipating Pediatric Emergencies in Ambulatory Surgery
March / April 2010
![]()
Be Prepared: Anticipating Pediatric
Emergencies in Ambulatory Surgery
Imagine a 2-year-old patient coming to your ambulatory surgery center for a simple tonsillectomy. You accompany him and his parents to the operating room where they are supported by the team — nurses, the surgeon, and the anesthesiologist. The team is caring, cheerful, competent, and professional. You know they will care for the patient as if he were their own son. The parents summon the courage to hold him as he is put under the anesthesia and kiss his soft cheek. You escort the parents to the lobby and reassure them, saying, “Help yourselves to coffee. We will take good care of him and see you soon.”
As the case progresses, an emergency occurs, and the nurse, surgeon, and anesthesiologist rush to intervene, asking, “What is this child’s weight?” At that moment, precious time is wasted looking for information in a scramble to treat the emergency. The caregivers will never forget this experience.
Emergencies cause pediatric caregivers great anxiety. Just talking about it causes many nurses and physicians to cringe.
Hunterdon Center for Surgery (a partner of Hunterdon Healthcare) provides patients with a convenient location for same-day surgical procedures. The facility mirrors the look and comfort of a typical doctor’s office, yet its four operating rooms house the same sophisticated medical equipment found at Hunterdon Medical Center. Many surgeons and anesthesiologists from Hunterdon Medical Center provide services at the Center for Surgery, where we perform approximately 4,600 cases per year, 350 of which are pediatric surgeries. Our most common pediatric cases are tonsillectomies, myringotomies, adenoidectomies, circumcisions, and hernia repairs. Our pediatric patients are well children who need outpatient surgery for a specific problem; once their procedures are completed, children spend a brief time in recovery and are discharged to home and resume normal activities.
|
Hunterdon Medical Center (HMC) is a 178-bed, non-profit community |
At a Pediatric Advanced Life Support (PALS) recertification class, our nurses, anesthesiologists, and PALS teacher began to discuss what we could do to make the care of children safer. The general feeling was that we are well prepared, trained in protocol, and have all the proper equipment available. However, our gut instinct said we could do better. We know that the unexpected can happen (Weick & Sutcliffe, 2001, chap. 1). We also understand that latent error and unintended actions emerge from systems over time, when least expected (Reason, 1990, pp. 173, 205–209). Our goal is to anticipate errors, to anticipate how the unexpected will emerge from our “normal” practices. As a team, therefore, we looked for failure points in our current practice and created a safer system of patient care. Anticipating error and looking for failure points is part of the science of patient safety and is one of the characteristics of a high reliability organization (Joint Commission Resources, 2002, pp. 1-6, 51-61). By being prepared for the unexpected, we can mange it.
Process Improvement
Our existing process involved having a registered nurse interview a parent or guardian of each pediatric patient by telephone to assess the patient one week prior to the date of surgery. Our anesthesia providers are experts in pediatric anesthesia, and all of our nurses are PALS certified. We use industry-standard Broselow bags that contain an endotracheal tube, intravenous catheter, intraosseous catheter, and suction catheter. Each bag is color coded according to the Broselow-Luten system of weight ranges for pediatric patients. The bags are located in the operating room hallway, close to the pediatric operating room, and in the post-anesthesia care unit (PACU). Despite all of this preparation, anxiety levels ran high when pediatric cases were on the schedule.
Technology Aid
During our discussions, we learned about a computer tool available for entering a patient’s weight and generating weight-based emergency drug doses. This program calculates dosages for emergency drugs and also calculates joules for defibrillation, all custom designed for the entered weight. The program lists all emergency protocol drugs in alphabetical order and provides the exact dosing and mixing requirements for the weight of the child. This computer program was available in our healthcare system but underutilized at our facility. We always obtained weights for our pediatric patients, but did not connect the weight-based information to the drug calculations.
A flow analysis of our current practice determined there was no universally held knowledge of this essential piece of patient information—the weight of the child. In the rare case of an emergency, the nurse would have to access the chart and look up the weight, or the anesthesiologist would have to call out the weight to the staff so they could go for the proper Broselow bag. Meanwhile, anesthesiologists would have to calculate weight-based calculations. In pediatric emergency situations, under intense pressure, the potential for human error is high. We identified a human factors gap between our knowledge, our system, and our ability to perform perfectly in a rare and undrilled pediatric emergency.
Implementing New Best Practice
How could we assure with 100% reliability that the correct weight would be known by all without delay? We decided to prepare every pediatric case as if there would be an emergency by using the computer program to generate specific medication protocols and color coding all the pieces of the process with the corresponding Broselow color.
We begin with the drug/joule calculation tool. We validate and confirm the child’s weight, enter it into the computer, and print the unique weight-specific emergency protocol. The protocol is placed on the front of the child’s chart. This position allows easy access to the protocol during an emergency. Next, we color code the protocol and the patient identification band (Figure 1).

Figure 1. Color-Coded Wristband on a Pediatric Patient
Photo courtesy of Lisa York
We purchased Sharpie markers in the colors we use for this system and placed them on a ring to keep them together. The markers are kept in the pre-op nurses’ station. Both the protocol and the identification band are color coded when placed on the chart two to three days prior to surgery and validated upon admission by the admitting nurse.
Our new system — preprinted weight-based, color-coded protocols and color-coded patient identification wristbands — eliminates relying on memory, enhances visual and verbal communication in the surgical team, and immediately provides important patient information to the entire team.
|
Hunterdon Healthcare uses Micromedex from Thomson Reuters for drug information and calculations. Although we were not aware of it when developing the color-coded system at the Hunterdon Center for Surgery, a there is a zone dosing system based on the Broselow color coding program available from the Broselow-Luten system. The “Color Coding Kids Hospital System™” is “a standardized therapeutic system whose goal is to increase safety, efficiency and comfort level whenever and wherever children receive medical treatment both by health care professionals and the lay public…. development of color-coded dosing zones which are specifically designed to accommodate not only equipment selection as in the present system but also to fall within the therapeutic ranges of medications, thus allowing ‘zone dosing’ for medications.” For more information, visit www.colorcodingkids.com. |
Prior to implementing this process, we held staff meetings and in-services for all team members and obtained their understanding, cooperation, and support. Charge nurses trained and coached pre-op nurses to color code the computer protocol and, later, the patient identification wristband upon arrival and verification of the child’s weight. We coached the operating room charge nurse to see that the operating room team was familiar with the location and content of the computer protocol and to verify color-code congruence before leaving the pre-op area. Surgeons and anesthesiologists supported these improvements and participated in the education and development of policy.
Parents are educated on our safety process so they understand why there are colored circles on their child’s identification band and medical record. This is another opportunity to involve parents in the safe care of their children, and to help them feel more secure that we do indeed treat each child as if “he were our own.” We have met with positive reactions from parents.
These discussions began in July 2008, and the process was implemented in October 2008. In April 2009 we presented a poster and abstract at the national conference for ambulatory surgery centers in Nashville, Tennessee. Upon our return, we shared our poster and idea with the Medical Center, and in July 2009 we were awarded a Patient Safety Champion Award by Hunterdon Healthcare. At the present time, this process is being replicated and implemented hospital-wide at Hunterdon Medical Center.
As part of our quality improvement program, we conducted a retrospective chart review six months after implementation to determine if the process was hardwired, i.e., utilized 100% of the time.
That review indicated we did not yet have 100% compliance with this new best practice (Figure 2), which led us to re-educate the staff on the details and importance of the new process.
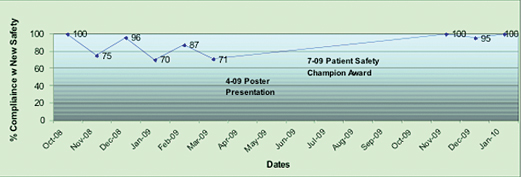
Figure 2. Percentage of Compliance with New Best Practice for Pediatric Emergency Preparedness
Our plan for hardwiring this best practice is to observe performance and measure compliance to the new procedure. In November 2009, an observational performance measurement was completed. We observed that the weight was verified with the identification band and the weight-specific emergency protocol was placed on the chart 100% of the time for all pediatric cases.
Conclusions
In this quality improvement process, we concentrated on a high-risk, rare event and improved our current best practice for anticipating and preparing for pediatric emergencies. This process can be replicated in any pediatric environment. Recognizing that a pediatric emergency is a universally feared event and that we deal with well children who have the potential to decompensate rapidly, we have provided a team-based assessment and communication tool to reduce the potential for human error and system failure.
Lisa York is the director of nursing at the Hunterdon Center for Surgery. She has an extensive nursing background in the peri-operative arena in hospital and ambulatory settings. She holds certifications as a legal nurse consultant and is a certified gastroenterology nurse. York holds bachelor’s and master’s degrees from Seton Hall University in New Jersey. She is a member of the New Jersey State Nurses Association and Sigma Theta Tau, International Honor Society of Nursing. York may be contacted at york.lisa@hunterdonhealthcare.org.
Stephanie Dougherty is director of patient safety and risk management at Hunterdon Medical Center. She has an extensive nursing background including critical care nursing, gastroenterology, and risk management. She has presented patient safety topics at state and national patient safety programs. Dougherty holds a bachelor’s degree in nursing from William Paterson University in New Jersey, is a graduate of the Patient Safety Fellowship program at Virginia Commonwealth University, and is currently a master-of-science candidate in patient safety leadership at the University of Illinois, Chicago. She is a member of the New Jersey Maternal Mortality Review Committee and has published previously in Patient Safety & Quality Healthcare. Dougherty may be contacted at dougherty.stephanie@hunterdonhealthcare.org.
References
Acknowledgments
We thank Dr. Ed Wang, anesthesia director of Hunterdon Center of Surgery, and Jackie Jerko, executive director of Hunterdon Center of Surgery, for their leadership and support for this best practice. We also thank Karen Beam, RN; Mary Ann Holgash, RN; Dr. Ed Spector; Dr. Robert Pickoff, CMO, MMM; Pat Steingall, MS, RN, NE-BC; Rob Church, RN; Leo Ryan, RT, BS, CHE; Denise Ryan, RN; Donna Cole, RN; Ellen Deshazo, RN; all the HMC Operating Room Nurses for adding this pediatric emergency ID band process to their WHO Surgical Safety Checklist; and the HMC Nurse Practice Council for supporting this best practice through Hunterdon Medical Center.
Figure 2. Percentage of Compliance with New Best Practice for Pediatric Emergency Preparedness
